Document 12014624
advertisement
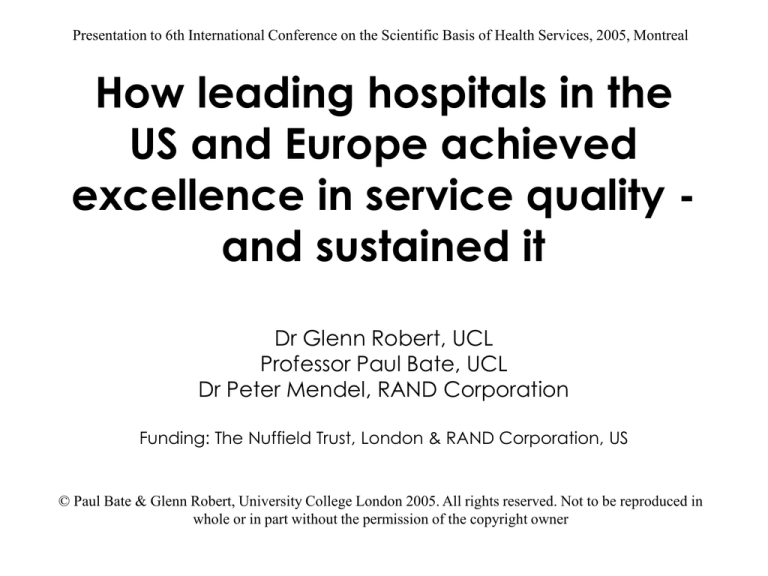
Presentation to 6th International Conference on the Scientific Basis of Health Services, 2005, Montreal How leading hospitals in the US and Europe achieved excellence in service quality and sustained it Dr Glenn Robert, UCL Professor Paul Bate, UCL Dr Peter Mendel, RAND Corporation Funding: The Nuffield Trust, London & RAND Corporation, US © Paul Bate & Glenn Robert, University College London 2005. All rights reserved. Not to be reproduced in whole or in part without the permission of the copyright owner Objective To re-trace the ‘quality journey’ of 8 high performing health care organizations in order to explore the processes that enabled them to successfully implement, spread and sustain quality improvement initiatives 2 Background The quality lottery: striking variation between health care organizations in how successful they are in implementing and sustaining Q & SI 3 One large study of American health care quality Source: McGlynn et al (2003) NEJM, 348, pp. 2635-2645 439 indicators of clinical quality of care Across 30 acute and chronic conditions Participants (N=6712) had received 54.9% of scientifically indicated care Conclusion: The ‘defect rate’ in the technical quality of American health care is approximately 45% It is probably the same in the UK! 4 Background • HSR getting better and better at measuring health outcomes and quality • Variation between (Jarman) and within (Adler) health care organizations • Strong on the ‘what’ but weaker on the ‘why’ and ‘how’ • Most HSR related to quality issues does not seek to explain the human and organisational causes of variation 5 Background • Move from describing to explaining • Processes and dynamics of improvement rather than list of ‘key success factors’ • Ethnographic case studies of organizations with a history and reputation for sustained quality improvement 6 Organizational sample • United States – – – – – Albany Medical Center (AIDS Treatment Center) Cedars-Sinai (Emergency Department) Luther Midelfort Mayo Health System (Critical Care Unit) San Diego Children’s Hosp. (Allergy & Immunology) SSM St. Joseph’s Health Center (Intensive Care Unit) • Netherlands – Reinier de Graaf Groep (Flow Varicies -- Vascular Surgery) • United Kingdom – Peterborough Hospitals (Radiology Services) – Royal Devon and Exeter (Orthopaedic Centre) 7 LOS ANGELES EAU CLAIRE PETERBOROUGH DELFT EXETER ALBANY ST. LOUIS SAN DIEGO 8 Study design • 15 days fieldwork in each site • Semi-structured interviews: macroand micro-system • Direct observation and documentary evidence • Draft narrative fed back to key informants • Analysed shared narratives and identified ‘challenges’, ‘elements’ and ‘processes’ that combine to explain improvement in health care 9 The generic challenges Despite huge variety similar sets of challenges: 1. Educational (a learning process to support continual improvement) 2. Political (addressing and dealing with the politics of change) 3. Cultural (giving ‘quality’ a shared, collective meaning, value and significance) 4. Emotional (engaging and mobilising people) 5. Structural (organising, planning and coordinating the improvement effort) 6. Physical and technical (supportive technologies and infrastructure) 10 Solutions to meet these challenges (elements) 1. Educational 1.1 A quiet, reflective form of leadership 1.2 Knowledge of ‘hard’ quality improvement methods and techniques … 2. Political 2.2 An agreed ‘compact’ for Q & SI between key interests 2.4 A dispersed, devolved/decentralised authority system … 3. Cultural 3.1 A philosophy and mission that highlights top quality patient care 3.7 An organisation whose image and identity are inextricably bound up with the concept of ‘excellence in quality’ … 11 4. 5. 6. Emotional 4.2 Building communities of practice and wider social commitment to Q & SI 4.6 Emotional involvement in the organisation improvement effort … Structural 5.1 An explicit and formally signed off strategy for Q & SI 5.10 Specialist interlocutor/connector roles with regard to quality: ‘boundary spanners’ (linking resources, people and ideas) … Physical & technical 6.1 A leadership that is aware of the material and symbolic/aesthetic importance of buildings and architecture, and incorporate this into its concept of service design 6.2 Whether it is free-standing and has control over its own buildings and space, data and technical systems … 12 Regulatory Environments Professional & Social Movements Outer Context Market & Resource Environments Inner Context Organization Performance Organization Size Technological Environments Organization Structure Educational Structural Task-centred leadership Quality strategy & plan Whole-systems design Devolved authority Multi-level leadership Quality leadership positions QI governance structure Quality department/group QI training programs Communities of practice Data & monitoring systems Results-oriented planning Enabling Admin role Boundary spanner roles Organizational ‘slack’ Pedagogical leadership Organizational change knowledge QI techniques knowledge Knowledge harvesting Experimentation & piloting Evidence-based learning Experience-based learning Physical & Technological Technology/design leadership Functional design of built env Aesthetic design of built env Info technology design Medical technology design Locating of built env & tech Cultural Values/symbolic leadership Culture of excellence Patient-centered ethic Culture of mindfulness Group/collaborative culture Scientific culture Culture of learning Formality-savvy culture Culture of empowerment Cosmopolitan culture Long term perspective Organizational identity Recruitment Acculturation Political Emotional Inspirational leadership Clinical & other change champions Collective momentum Professional & social affiliations Quality as a mission/calling Emotional commitment Improvement campaigns Politically-credible leadership Clinical engagement Peer-to-peer relationships Clinical-Managerial partnering Empowering staff Empowering patients External partnering 13 Regulatory Environments Professional & Social Movements Outer Context Market & Resource Environments Inner Context Organization Performance Organization Size Technological Environments Organization Structure Educational Structural Task-centred leadership Quality strategy & plan Whole-systems design Devolved authority Multi-level leadership Quality leadership positions QI governance structure Quality department/group QI training programs Communities of practice Data & monitoring systems Results-oriented planning Enabling Admin role Boundary spanner roles Organizational ‘slack’ Pedagogical leadership Organizational change knowledge QI techniques knowledge Knowledge harvesting Experimentation & piloting Evidence-based learning Experience-based learning Physical & Technological Technology/design leadership Functional design of built env Aesthetic design of built env Info technology design Medical technology design Locating of built env & tech Cultural Values/symbolic leadership Culture of excellence Patient-centered ethic Culture of mindfulness Group/collaborative culture Scientific culture Culture of learning Formality-savvy culture Culture of empowerment Cosmopolitan culture Long term perspective Organizational identity Recruitment Acculturation Political Emotional Inspirational leadership Clinical & other change champions Collective momentum Professional & social affiliations Quality as a mission/calling Emotional commitment Improvement campaigns Politically-credible leadership Clinical engagement Peer-to-peer relationships Clinical-Managerial partnering Empowering staff Empowering patients External partnering 14 Regulatory Environments Professional & Social Movements Outer Context Market & Resource Environments Inner Context Organization Performance Organization Size Technological Environments Organization Structure Educational Structural Task-centred leadership Quality strategy & plan Whole-systems design Devolved authority Multi-level leadership Quality leadership positions QI governance structure Quality department/group QI training programs Communities of practice Data & monitoring systems Results-oriented planning Enabling Admin role Boundary spanner roles Organizational ‘slack’ Physical & Technological Technology/design leadership Functional design of built env Aesthetic design of built env Info technology design Medical technology design Locating of built env & tech Pedagogical leadership Organizational change knowledge QI techniques knowledge Knowledge harvesting Experimentation & piloting Evidence-based learning Experience-based learning ? Emotional Inspirational leadership Clinical & other change champions Collective momentum Professional & social affiliations Quality as a mission/calling Emotional commitment Improvement campaigns Cultural Values/symbolic leadership Culture of excellence Patient-centered ethic Culture of mindfulness Group/collaborative culture Scientific culture Culture of learning Formality-savvy culture Culture of empowerment Cosmopolitan culture Long term perspective Organizational identity Recruitment Acculturation Political Politically-credible leadership Clinical engagement Peer-to-peer relationships Clinical-Managerial partnering Empowering staff Empowering patients External partnering 15 RESULTS So what processes enabled these health care organizations to successfully implement, spread and sustain Q & SI initiatives? 16 A flavour .. two case studies Cedars-Sinai, Los Angeles Peterborough • 875 beds • 670 beds (2 sites) • 6,600 staff and 1,700 • 2,300 wte staff affiliated physicians • Acute medical services • Primary service area to 280,000 in east of consists of 2.3 million England people ($70m p.a on • Income of £89.1m in community outreach) 2001/02 • Major teaching hospital • 3 star Trust 2001/02 and (UCLA) 2002/03 17 Process mapping method – Step One Systematically coded the validated case narratives for mentions of processes between elements 18 An example In this spirit, the hospital decided to hire this physician to lend clinical background and credibility to the quality effort [2.1 to 2.2]: “So he… went around looking at evidence based stuff, and began to bring to the institution a whole discipline [3.8 to 5.15] around analyzing process, flow diagrams, cradle diagrams, privatization approaches,… and we began to infuse the organization with that approach. We linked up then with the national demonstration project later [1.4 to 3.10] becoming the Institute for Healthcare Improvement, [he] became faculty in the IHI, as you probably know, and kept us connected with a network of people who had a growing similar interest around these kinds of things” [5.10 to 1.4]. 19 Process mapping method – Step Two Employed social network analysis techniques to examine and visualize the patterns of relations among the organizational processes for each case study 20 Cedars-Sinai Sub-Process Mapping C3.10 PT6.6 S5.2 IC1.1 S5.3 S5.1 S5.5 OC1.4 C3.8 S5.4 S5.10 S5.7 P2.3 P2.2 EM4.4 ED1.5 ED1.4 S5.12 OC1.5 EM4.6 S5.6 S5.15 S5.9 S5.13 P2.1 ED1.3 ED1.2 EM4.2 S5.11 C3.6 C3.7 C3.11 C3.2 S5.8 ED1.1 P2.5 EM4.3 C3.5 EM4.1 P2.4 ED1.6 PT6.5 C3.1 PT6.1 C3.14 IC1.2 P2.7 S5.14 C3.12 C3.3 PT6.3 C3.13 PT6.2 EM4.5 OC1.6 IC1.3 ED1.7 Note: Dotted line indicates negative relationship. OC1.7 Educational Political Cultural Emotional Structural Physical/Technical Inner Context 21 Outer Context Cedars-Sinai Sub-Process Mapping C Cosmop ClinTechn Supp TaskLship OrgSize WholeSysDes QStrategy QLdrs C Formal Regulatory Environment DecAuth QIdept Peer-to-Peer Profl-Social Affiliations EmotInvlv KHarvest DistrLdrs DataSys QI Training QGovern Enabling Admin C Science QTraining Programs Pedag Lship Values Lship StaffEmpw ICTSupp PT6.1 QSlackRes ClinEng Experm Plan Process Mrkt/Resource Environment Bndry Spans Patient Centred Comm-of Practice LearnC Clin Champions OrgChng Training LTermC GroupC Evid-based Learning Org Identity QMission Note: Dotted line indicates negative relationship. CollMoment OrgPerf InspLship Clin-Mgt Prtnr CExcell Socializ OrgStruc Techn/Design Lship Recruit Retain Phys Aesthetics CredLship ExtPrtnr Social Mvmnts Exp-based Learning AvailTechn Educational Political Cultural Emotional Structural Physical/Technical Inner Context 22 Outer Context Cedars-Sinai Process Mapping Process Structural Cultural Educational Political Emotional Physical & Technical Outer Context Inner Context Total SubProcess Ties (#) 80 69 41 30 13 11 4 3 W/in Process (%) 30% 23% 5% 13% 15% 0% 25% 0% IN-ties (%) 29% 39% 51% 50% 62% 27% 75% 33% OUT-ties (%) 41% 38% 44% 37% 23% 73% 0% 67% Most Central Sub-Processes Communities-of-Practice, Quality governance systems, Distributed leadership, Data and monitoring systems, Boundary-spanner roles Group culture, Values/symbolic leadership, Culture of learning Clinical engagement 23 Peterborough Sub-Process Mapping IC1.3 IC1.1 C3.2 PT6.6 ED1.1 P2.1 OC1.5 C3.11 S5.11 C3.5 C3.9 IC1.2 P2.3 S5.6 ED1.5 EM4.1 C3.7 C3.1 S5.5 S5.4 P2.7 P2.5 ED1.2 C3.6 PT6.5 P2.2 S5.7 OC1.6 S5.3 S5.10 S5.8 C3.12 ED1.3 OC1.4 ED1.4 S5.9 W4.3 EM4.6 C3.13 S5.15 P2.4 S5.14 S5.13 ED1.6 S5.2 ED1.7 Educational Political Cultural Emotional Structural Physical/Technical Inner Context 24 Outer Context Peterborough Sub-Process Mapping OrgPerf OrgSize ClinTechn Supp Pedag Lship CredLship Values Lship Mrkt/Resource Environment LTermC Comm-of-Practice GroupC Peer-to Peer InspLship EmpwC OrgStruc LearnC CExcell QLdrs Social Mvmnts ExtPrtnr OrgChng Training QIdept Recruit Retain DecAuth StaffEmpw KHarvest Enabling Admin Coll Moment ClinEng ScienceC ICTSupp DataSys Clin-Mgt Prtnr WholeSysDes BndrySpans QTraining Programs EmotInvlv DistrLdrs Experm Org Identity QI Training Regulatory Environment QSlackRes QGovern TaskLship Exp-based Learning Evid-based Learning Educational Political Cultural Emotional Structural Physical/Technical Inner Context 25 Outer Context Peterborough Process Mapping Process Total SubProcess Ties (#) W/in Process (%) IN-ties (%) OUT-ties (%) Structural Cultural Political Educational Outer Context Inner Context Physical & Technical Emotional 52 49 43 26 7 6 6 5 25% 14% 7% 8% 0% 0% 0% 20% 10% 71% 56% 50% 29% 0% 33% 60% 65% 14% 37% 42% 71% 100% 67% 20% Most Central Sub-Processes QI facilitating team, Enabling administrative role Culture of empowerment, Group culture Empowering staff, Clinical engagement Experimentation & pilots 26 Comparative Process Mappings Peterborough Cedars-Sinai 27 .. and the emotional “People here aren’t just motivated. This isn’t their job, it’s a mission, it’s their life, it’s the cause they’re committed to. For them, it’s personal.” (Director HIV AIDS Programme, Albany Medical Centre, New York) “Perfect care is something we never reach, but like the North Star, it serves as a beacon to guide us … Every day Children’s should strive to be even better than before. Our physicians, our nurses, and our staff seek to attain it; our families deserve it.” (Foreword of the Children’s Agenda, Children’s Hospital and Health Centre’s strategic and business plan, June 2001) 28 Conclusions • The generic but variable thesis: ‘many paths up the mountain’ • Failures and ‘bumps in the road’ • Multi-level, multi-dimensional process based model of service improvement • Context and physical/technology factors important in realising quality but cultural and structural response of organizations largely determine whether QI is sustained • Yes, human and organisational factors are important – and need to understand ‘how’ and ‘why’ 29 Jeopardising change Lack of a … Learning process Political process Cultural process Mobilisation Planning & co-ordination Physical infrastructure & technical systems Can lead to… Amnesia or frustration Inertia Evaporation Energy-sink Fragmentation Exhaustion 30 For comments and further information: g.robert@chime.ucl.ac.uk 31 Organizing for Quality: Journeys of Improvement at Leading Healthcare Organizations in the US & UK James L. Zazzali, Ph.D., M.P.H., RAND Corporation Glenn Robert, Ph.D., UCL Medical School Peter Mendel, Ph.D., RAND Corporation Paul Bate, Ph.D., UCL Medical School Funding Sources: Nuffield Trust, London RAND Corporation Health Unit, Santa Monica Copyright, all rights reserved, 2005 Research Objectives • To present cross-site and cross-national findings regarding the ability of healthcare organizations to sustain QI programs and processes • To identify best practices in change management related to the introduction and implementation of QI • To approach this with a decidedly organizational perspective 33 Study Design • Mixed methods with a multilevel approach • Interviews with over 100 senior leaders at 11 Health care systems in 3 countries (results today only for US & UK) • Site visits to one “high performing” department within each of the 11 health systems to observe and interview staff • Interview data used to construct survey items • Survey of staff in the “high performing” departments 34 Organizational Sample • United States – Albany Medical Center (AIDS Treatment Center) – Cedars-Sinai (Emergency Department) – Geisinger Health System (Rheumatology) – Luther Midelfort Mayo Health System (Critical Care Unit) – San Diego Children’s Hosp. (Allergy & Immunology) – SSM St. Joseph’s Health Center (Intensive Care Unit) • Netherlands – Reinier de Graaf Groep (Flow Varicies -- Vascular Surgery) • United Kingdom – Kettering General Hospital (Accident & Emergency Services) – Kings College (Breast Unit) – Peterborough Hospitals (Radiology Services) – Royal Devon and Exeter (Orthopaedic Centre) 35 Survey of “High Performing” Departments • Survey measured: – The degree to which 9 key factors related to sustaining QI efforts were met in the department – Perceptions of importance of these factors for 5 of the 9 areas – The organizational culture of the department – The respondents’ level of QI training and QI team experience – Respondents’ socio-demographic characteristics • Survey sample – 477 respondents across 10 sites in the US & UK – 48% response rate with two mailings 36 Nine Factors Related to Sustaining QI • • • • • • • Organizational slack for quality improvement Quality resource infrastructure Availability and use of data Culture of sharing and learning Distribution of responsibility Organizational identity Senior leaders creating a vision, scripting & motivating • Communication and discourse • Systems perspective/thinking 37 Nine Factors Related to Sustaining QI • A. Organizational slack for quality improvement – 1) Our unit provides staff with time and other resources to work on implementing new ways of improving how we do things here. – 2) I have opportunities to visit or interact with people in other units or outside this organization to bring back new ideas which might improve how we do things here. • B. Quality resource infrastructure – 3) Our unit has access to people who can provide training, advice and support in quality improvement. • C. Availability and use of data – 4) Our unit has easy access to data that is useful for understanding the processes and outcomes of our work. – 5) Our unit routinely makes changes based on measurement of the processes and outcomes of our work. 38 Nine Factors Related to Sustaining QI • D. Culture of sharing and learning – 6) People in our unit like to share their ideas and expertise with one another. • E. Distribution of responsibility – 7) My efforts can play an important role in the success of quality improvement activities in this unit. – 8) Quality improvement activities can produce significantly better patient care and outcomes in our unit. • F. Organizational identity – 9) This organization has a mission or purpose that I strongly identify with. – 10) This organization has a particular history that I am proud of. 39 Nine Factors Related to Sustaining QI • G. Senior leaders creating a vision, scripting & motivating – 11) Senior management within this organization know how to inspire and motivate staff across areas to work toward common goals. – 12) Senior management within this organization make improving the quality of patient care a priority. • H. Communication and discourse – 13) People in our unit feel they can freely express their views and have their opinions listened to. – 14) There is good communication between our unit and others in the organization on important issues of delivering patient care. • I. Systems perspective/systems thinking – 15) People in our unit really understand how patients move across departments within this organization. – 16) There is strong inter-departmental coordination within this organization. 40 Challenges in Sustaining QI 1.0 2.0 3.0 4.0 4.0 Sr. mgmt. knows how to inspire & motivate staff across areas to work toward common goals. * 4.1 3.9 4.4 People in our unit like to share their ideas and expertise 6.0 * 3.8 Opportunities to visit or interact with people in other units or outside this organization to bring back new ideas 4.2 * 4.4 There is good comm. between our unit and others on important issues of delivering patient care 4.2 4.5 There is strong inter-departmental coordination 4.0 US * denotes p<.05 5.0 * UK 41 Advances in Sustaining QI 1.0 2.0 3.0 4.0 5.0 6.0 5.3 This organization has a mission or purpose that I strongly identify with. 4.7 QI activities can produce significantly better patient care and outcomes 5.2 5.0 My efforts can play an important role in the success of QI activities 5.2 5.0 This organization has a particular history that I am proud of. 5.1 5.0 * * * 5.0 4.8 People in our unit feel they can freely express their views and have their opinions listened to US * denotes p<.05 * UK 42 Importance of Factors Related to QI Sustainability 1.0 2.0 3.0 4.0 5.0 6.0 Training and time for improving quality of patient care and service 5.7 5.7 Senior management makes improving the quality of patient care a priority 5.6 5.5 This organization has a mission or purpose that I strongly identify with 5.5 5.1 People in department understand how patients move across departments in this organization 5.4 5.3 Access to professional staff for training, support and advice on quality improvement 5.4 5.4 US * denotes p<.05 UK * * * 43 QI Training & Participation 0 Have you been trained in formal quality improvement principles and techniques (e.g., principles espoused by Deming or Juran, Six Sigma, Rapid C ycle, Plan-Do-Study-Act, or other quality improvement techniques like Process Mapping, Root C ause Analysis, etc. Have you ever served on a quality improvement team in this organization (i.e., a team specifically formed to analyze and improve the quality of care or service)? 10 20 30 50 60 36 * 11 51 * 15 US (% Yes) * denotes p<.05 40 UK (% Yes) 44 QI Training 0 5 15 25 30 35 40 45 50 7 33 0 46 Nurses Total 20 23 Non- c linic al Physic ians 10 19 36 11 US % Yes UK % Yes 45 QI Team Participation 0 Non-clinical 10 20 40 50 60 38 7 56 Physicians 17 57 Nurses Total 30 22 51 15 US % Yes UK % Yes 46 Differences in Organizational Culture Group Culture (teamwork & affiliation) 35.0 30.0 25.0 20.0 15.0 10.0 5.0 Rational Culture (task oriented) Developmental Culture (risk taking/entrepreneurial) 0.0 Hierarchical Culture (bureaucracy) US UK 47 Conclusions • These organizations face similar challenges & successes for QI implementation and sustainability • QI training and participation are more diffuse in the US • The organizational cultures are different for the US & UK sites 48 Next Steps • Multivariate (and multilevel) models of individuals’ perceptions of key factors related to sustaining QI and their importance, predicted by organizational culture and QI training and participation • Book presenting case studies and synthesizing an organizational model of factors related to QI sustainability 49 Components to a process model of improvement Receptive context - Outer context - Inner context 6 generic challenges 63 elements ?? processes 50