OU THE UNIVERSITY OF OKLAHOMA EMPLOYEE BENEFITS 2016
advertisement

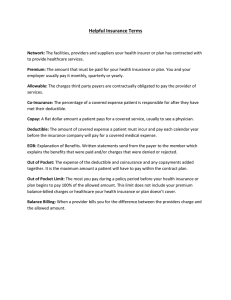
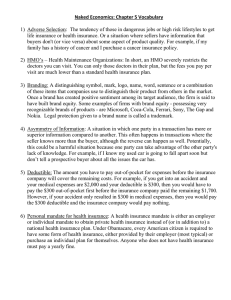
U O THE UNIVERSITY OF OKLAHOMA EMPLOYEE BENEFITS 2016 TABLE OF CONTENTS Benefit Enrollment & Making Changes During the Year . . . . . . . . . . . . . . . . . . . 1 Medical Plan Options. . . . . . . . . . . . . . . . . . . . . 1-3 BlueLincs HMOSM . . . . . . . . . . . . . . . . . . . . . . . . 4 BlueOptionsSM . . . . . . . . . . . . . . . . . . . . . . . . . . 4-5 BlueEdge HSASM . . . . . . . . . . . . . . . . . . . . . . . . . 6 What’s Not Covered. . . . . . . . . . . . . . . . . . . . . . . 7 ID Cards. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 Wellness Guide . . . . . . . . . . . . . . . . . . . . . . . . 8-10 Resource Guide. . . . . . . . . . . . . . . . . . . . . . . . . 11 Plan Comparison Chart . . . . . . . . . . . . . . . . . 12-17 Contacts . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 Through It All.® This enrollment guide highlights OU’s Benefits plans. A complete description of each plan can be found in your Certificate of Benefits Booklet or Member Handbook. Every effort has been made to provide an accurate summary of the plans. However, this is a summary guide. If there is a conflict between this material and the Certificate of Benefits or Member Handbook, the Certificate of Benefits Booklet or Member Handbook will govern. If you have any questions after reviewing your enrollment materials, please contact BCBSOK customer service. WELCOME Welcome to Blue Cross and Blue Shield of Oklahoma, and to your benefit 01 Except for coverage of a newborn or adopted child, all other enrollment period. This is your opportunity to select health benefits for you and Benefit Enrollment & Making Changes During the Year your family for the coming year. During the open and new member enrollment period, you on the child’s date of birth. Coverage for an adopted child is For 75 years, Blue Cross and Blue Shield of Oklahoma (BCBSOK) has delivered high value products and unrivaled customer service to more Oklahomans than any other health insurance plan. And our nationwide network of physicians and hospitals, coupled with local resources and friendly service, keeps you connected to your health care coverage no matter where you are. can add or delete dependents from your health care coverage without a “qualifying event”. The enrollment period is the time to make sure all of your eligible dependents are enrolled and that Human Resources has all the correct information about your dependents on file. The health care plan options you select during the enrollment period will remain in effect during the calendar year. Through the University of Oklahoma, we are pleased to offer benefits that give you and your family the best care possible and services that allow you to put your health care decisions and health education closer to your fingertips. Please take a few minutes to look through this summary guide and review the options that are available to you. You may also visit bcbsok.com/ou for more information. It is our desire during the enrollment period that you gain a clear understanding of each option and to help you decide what is best for your health care needs. In order to change benefit elections outside of the enrollment period, the employee must have: 1) Experienced an Applicable Qualifying Event, as defined by the Internal Revenue Service (IRS). Changes based on financial reasons alone are not allowed under the current IRS regulations. AND BCBSOK members don’t just have access to traditional insurance coverage; you also have a complete suite 2) The request for a change of benefits must be made within 31 of health and wellness resources and tools at your fingertips, to encourage healthier living and smarter health days of the Applicable Qualifying Event. decisions. Blue Cross and Blue Shield of Oklahoma is a health care industry leader in creating and promoting Within the context of changing benefits, “Applicable” refers to a wellness programs that you and your family can conveniently integrate into your daily life. Merging technology and change that is directly related to the individual experiencing the medical management with online resources, education, one-on-one coaching, rewards and multiple touch points, BCBSOK’s Blue Care Connection® program aims to ultimately improve you and your family’s health and wellness. Our goal at Blue Cross and Blue Shield of Oklahoma is to provide you with first class service, and to do the job Stephania Grober Vice President, Marketing and Sales Blue Cross and Blue Shield of Oklahoma the qualifying event. Coverage for the newborn is effective effective on the date of placement. In both instances, the employee must initiate and complete the appropriate paperwork. Changes in provider networks (for example, your doctor leaving the network) are not considered acceptable reasons for you to be able to change your product election outside of the enrollment period. Please visit the “Benefits” section of the OU Human Resources website for more information at hr.ou.edu. Eligibility Please visit the “Benefits” section of the OU Human Resources website for information at hr.ou.edu. Medical Plan Options The following pages provide an overview of the health benefits of each of the program options. These are only summaries – not the actual plan descriptions. If you have questions that qualifying event. aren’t answered in the summary information in this guide, A qualifying event includes: detailed Certificate of Benefits or Member Handbook. Dental please contact customer service at 888-881-4648 or review the care benefits are offered separately, and are not highlighted in n A birth or adoption n Marriage, divorce or legal separation n Death n Child loses eligibility because of age n Employee’s spouse gains or loses coverage through QUALIFYING EVENT. In no event will you be able to switch from employment one plan to another during the year, unless you are on the HMO right the first time, every time. We appreciate the opportunity to serve you. Sincerely, changes in coverage begin the first day of the month following n Significant change in the financial terms of health benefits provided through a spouse’s employer or another carrier this benefit guide. The medical plan you select during the enrollment period will apply for the calendar year. You will not be able to make changes to your medical plan during the year UNLESS YOU HAVE A plan and move outside the service area. A brief description of the various aspects of each program follows on the next pages. 02 03 Medical Plan Comparisons 1) Benefit design – Each of the three plans promotes wellness, 3) Provider access – The Blue Choice PPO network is The Away From Home Care Program does not cover the offers preventive care and has unlimited lifetime maximums. BCBSOK’s largest network. BlueEdge HSA utilizes the Blue entire United States. If you are considering the HMO, and Available Health Care Plans However, there are notable differences among the plans, which Choice PPO network, which means you will have the lowest out- you have an out-of-state dependent or plans to move out- There are 3 notably different benefit plans: BlueLincs HMO, impact the coverage and out-of-pocket costs you’ll have when of-pocket costs when you see providers in the Blue Choice PPO of-state, please contact BCBSOK at 888-881-4648 to discuss BlueOptions or BlueEdge HSA. The BlueLincs HMO plan is you utilize your benefits. network. The Blue Preferred PPO network is BCBSOK’s second your options. closed to new participants in 2016. BlueLincs HMO is a health maintenance organization type of plan, otherwise known as a “managed care” plan. It requires selection and use of a primary care physician (PCP), and referrals are usually needed for specialty care. organization (PPO) types of plans. Blue Cross and Blue Shield of Oklahoma has negotiated discounts with medical providers (doctors, hospitals etc) to reduce the cost of health care. The discount is applied before there is any payment for services from you or BCBSOK. lowest out-of-pocket expense because the cost of services is usually lower and the benefits you receive are higher. SM network, which is BCBSOK’s largest PPO network. n applicable to some services. There is no calendar year deductible to satisfy except for certain services such as inpatient/outpatient equipment, and certain imaging services such as MRI, PET and CT scans. BlueOptions has a calendar year deductible to satisfy before coverage begins. However, like the HMO plan, many services are covered with just a copayment, so depending on the type of services you need, you may not even need to meet your When you see a provider that is in-network, you will have the BlueEdge HSA uses the Blue Choice PPO applicable copayments and a low calendar year deductible that is hospital services, skilled nursing facilities, durable medical BlueOptions and BlueEdge HSA are preferred provider n The BlueLincs HMO has very low out-of-pocket costs with only BlueOptions offers a unique tiered structure that allows you the flexibility to see providers in the Blue Choice PPO or Blue Preferred PPOSM networks. However, you will have the lowest out-of-pocket expense when you see providers in the Blue Preferred PPO network because the discounts are greater. The Blue Preferred PPO network has fewer providers than the Blue Choice PPO network. BlueOptions and BlueEdge HSA also give you the flexibility to choose an out-of-network provider, with whom BCBSOK does not have a contract, and still receive health care benefits. However, you may have more out-of-pocket expense when you choose an out-of-network provider. The BlueEdge HSA pairs a high deductible and the Blue Choice PPO network with a health savings account (HSA). The HSA can be used to pay for certain out-of-pocket medical expenses. deductible during the year. Most preventive care services are fully covered under BlueOptions if using in-network providers, which largest network, including providers in the Tulsa and Oklahoma City metro areas as well as many providers in the rest of the state. BlueOptions offers a unique tiered structure that allows you the flexibility to see providers in the Blue Choice PPO or Blue Preferred PPO networks. However, you will have the lowest out-of-pocket costs when you see providers in the Blue Preferred PPO network because the discounts are greater. BlueOptions and BlueEdge HSA also give you the flexibility to choose an out-of-network provider, with whom BCBSOK does not have a contract, and still receive health care benefits. However, you may have more outof-pocket expense when you choose an out-of-network provider. There are fewer providers in the BlueLincs HMO network such as well child and adult immunizations, routine exams, than there are in the Blue Choice PPO or Blue Preferred PPO gynecological exams, mammograms and prostate specific antigen network. Be sure to verify that your current physicians are in (PSA) tests. When you see providers in the Blue Preferred PPO the network for the plan you are considering. If you are joining network, you will have the lowest out-of-pocket expense because the HMO and want to choose a new primary care physician the discounts are greater. (PCP), make sure that physician is accepting new patients. The BlueEdge HSA has a notably higher deductible to satisfy With BlueLincs HMO, out-of-state coverage is generally limited each year, and some services, except for some of your to emergency treatment. If you have a dependent living out-of- preventive care benefits, are subject to that deductible before state (for example, a college student), or if you are moving out- your coverage begins. To help offset the higher deductible, of-state during the year, you may be eligible to enroll in the Away money is put into a health savings account each year on your From Home Care® Program, which connects BlueLincs HMO behalf, which can be applied to your deductible or other eligible members to a participating out-of-state HMO. Choice PPO network, so you will have the lowest out-of-pocket costs when you use providers in the Blue Choice PPO network. access to contracting providers through the BlueCard® Program when you or your covered family members live, work, or travel anywhere in the country. Additionally, when you travel outside the United States, PPO members have access to contracting providers in more than 200 countries through BlueCard Worldwide®. You can verify that your current physicians are in the network for the plan you are considering by checking the online provider directory at bcbsok.com/ou. 4) Flexibility – BlueOptions and BlueEdge HSA give you the means you will pay no copayment or coinsurance for services out-of-pocket medical expenses. BlueEdge HSA uses the Blue BlueOptions and BlueEdge HSA members have nationwide most flexibility since you have coverage for both in-network (PPO) and out-of-network providers. Keep in mind that you will always receive your highest level of benefits and lowest out-ofpocket costs when choosing an in-network provider. BlueOptions gives you additional freedom of choice and flexibility because you can see providers in the Blue Choice PPO or Blue Preferred PPO networks and still receive benefits. (For BlueOptions members, you will have the lowest out-of-pocket costs when you see providers in the Blue Preferred PPO network.) The BlueLincs HMO plan is a managed care plan that requires the use of BlueLincs HMO contracted providers. You also are required to select a primary care physician (PCP) to provide or coordinate most of your care. Referrals are generally required from your PCP for most specialty care. BlueOptions and BlueEdge HSA do not have these requirements; you “manage” your own care. 2) Rates – It’s important to compare the rates of each plan, while keeping in mind the benefits that come with each plan. BlueLincs HMO has the most predictable out-of-pocket costs when you need to utilize your benefits. Keep in mind, however, that as an HMO, BlueLincs HMO has less flexibility than the Key Areas to Consider other two plans, and it has a smaller network of providers to You should choose the plan best suited for you and your family. choose from. BlueOptions provides a high level of flexibility There are important differences between the plans that should when choosing your providers and out-of-pocket costs. be considered. Details and benefits of each plan are listed on the BlueEdge HSA has the lowest premiums. It provides a high level People sometimes turn to popular diets to achieve quick weight following pages for easy comparison. Here are some additional of flexibility, but it has higher out-of-pocket costs than the other loss. For lasting changes and healthy eating, balance what you eat factors to keep in mind: two plans. to meet your need for nutrition and enjoyment. Enjoy a variety of Nourish to flourish. foods while keeping key food groups in mind and use moderation when choosing less nutritious foods. 04 05 BlueLincs HMO BlueOptions In BlueLincs HMO, you must specify a Primary Care Physician BlueOptions is a preferred provider organization (PPO) plan, which (PCP) during your enrollment. During your online enrollment gives you the flexibility to choose your provider and network at the process, you will be asked to provide your PCP’s National time of service. BlueOptions gives you the freedom to select any Provider Identification (NPI) number. health care provider (whether they are in-network or not). You do How do my benefits work when I am out-of-state? Choice PPO network. If you visit your doctor, your benefits will not need to select a primary care physician. Your choice of health BlueOptions members have nationwide access to contracting be applied for the Blue Preferred PPO network, which means care providers can affect the level of health care benefits (including providers through the BlueCard Program when you or your that you will have the lowest out-of-pocket expense. copayment and deductible amounts) – based on the network your covered family members live, work, or travel anywhere in the provider is in. With the BlueOptions plan, you can choose from two country. Your benefits will generally be paid at the highest different networks each time you need health care. Or, you may benefit level, since Blue Preferred PPO providers are mostly choose to see providers that are not in a network (out-of-network). located in Oklahoma. You can search for BlueCard providers in n You must select your own PCP from the HMO provider network, and you must see him or her to coordinate care for most services in order to receive benefits. n You may choose a different PCP for each family member, or you may select the same one for the entire family. n If you receive non-emergency care outside the HMO network n without a referral from your PCP, you receive no benefits. and pays your benefits at the highest level, which means you will have the lowest out-of-pocket costs when you use BlueLincs HMO Frequently Asked Questions Where do I get my PCP’s NPI number? Visit bcbsok.com/ou providers in the Blue Preferred PPO network. n and click on your plan type in the Find a Doctor section. There the same with the Blue Preferred PPO and Blue Choice PPO that is available through the BlueLincs HMOSM network. You online enrollment process. I want to change my current PCP. Can I do that during the enrollment period? Yes, and you are able to do that up to 4 times a year. Consult the provider directory on bcbsok.com/ ou to choose a PCP in the BlueLincs HMO network. During the enrollment period, include the PCP’s NPI. During the year, simply call BCBSOK customer service to make this change. My dependents live out-of-state. Can I choose BlueLincs HMO? With BlueLincs HMO, out-of-state coverage is generally limited to emergency treatment only. If you have a dependent living out-of-state (for example, a college student), or if you are moving out-of-state during the year, you or your dependent may be eligible to enroll in the Away From Home Care Program, The Blue Choice PPO network will pay your benefits at the second highest level, although some aspects of coverage are you can search for a PCP you currently use or locate a new PCP must enter the PCP’s NPI (as shown on the website) during the The Blue Preferred PPO network provides the biggest discount networks. n If you see out-of-network providers, you will receive no discounts and your benefits will be paid at the lowest allowed amount. Finding out which network your providers are located in is easy! Simply visit bcbsok.com/ou and click on your plan type in the Find a Doctor section. You can search for a doctor by name, location, network, or specialty, such as dermatology or cardiology. BlueOptions Frequently Asked Questions How do I find a doctor in the Blue Preferred PPO or Blue Choice PPO network? Go to bcbsok.com/ou and use the provider directory, or call BCBSOK customer service. the online provider directory at bcbsok.com/ou. Do I need a referral from my doctor to see a specialist? No. With the BlueOptions plan you can see any doctor at any time without a referral. If you see a specialist who is part of the Blue Preferred PPO network, your benefits will be paid at the highest level and your out-of-pocket costs will be lowest. You can also see a specialist in the Blue Choice PPO network or not part of the network, but your benefits will be paid at a lower level. Can I see providers in both the Blue Preferred PPO and Blue Choice PPO networks? Yes, with BlueOptions, you have the freedom to see any doctor you choose at any time. You can choose different networks for different health care services and/ or for different members of your family. For example, you can see a physician in the Blue Preferred PPO network while your spouse and children see a physician in the Blue Choice PPO network. Your benefits are determined at the point of service, The office copayments and deductible are lower for the Blue which means that your copayment and deductible amounts Preferred PPO network than the Blue Choice PPO network. The depend on which network you choose. Your choice can affect coinsurance paid by BCBSOK and the out-of-pocket maximums the amount of benefits you receive. You will have the lowest are the same for the Blue Preferred PPO and Blue Choice PPO out-of-pocket expense when you see providers in the Blue network. Preferred PPO network. Keep in mind that deductibles vary depending on the network you choose. The deductibles update which connects BlueLincs HMO members to a participating out- Most preventive care services for in-network providers are fully each other, which means that at one point during the year, you of-state HMO. The program is designed for members who: covered under the BlueOptions plan, which means you will pay may have satisfied your Blue Preferred PPO deductible but still no copayment or coinsurance for services such as well child have more to satisfy for the Blue Choice PPO network. If you and adult immunizations, routine exams, gynecological exams, were to continue to see Blue Preferred PPO providers, then mammograms and prostate specific antigen (PSA) tests. your deductible is met. If you visit a Blue Choice PPO (or out- n n have a child attending school out-of-state have family members living in different service areas n have a long-term work assignment in another state n are retired with dual residence The Away From Home Care Program does not cover every area in the entire United States. If you are considering BlueLincs HMO, and you have an out-of-state dependent or plans to move out-of-state, please contact BlueLincs HMO at 800-580-6202 to discuss your options. of-network) provider, you will first have to satisfy the difference between the deductible for that network and the Blue Preferred PPO deductible before coinsurance applies again. Can my doctor be a part of both networks? What happens if this is the case? Be sure to ask your provider which network(s) they are in. They may be in more than one network. If that is the case, your benefits will be applied at the highest network level. For example, your doctor is in the Blue Preferred PPO and Blue Can I see a doctor or use a service that is out of network? Yes. However, the amount your plan pays for covered services is based on the allowed amount described in your Certificate of Benefits. If an out-of-network provider charges more than the allowed amount, you may have to pay the difference. 06 07 BlueEdge HSA What’s Not Covered ID Cards What is it? Your plan options do not cover all health care expenses, and You should present your ID card when visiting a physician’s office include exclusions and limitations. You should refer to plan- or hospital, and verify that they have the correct insurance never need a referral to see a specialist. specific documents to determine which health care services information on file for you. Your card will resemble the card are covered and to what extent. The following is a partial below, and will be customized with your name and plan Under BlueEdge HSA, some of your well child and adult list of services and supplies that are generally not covered. information. Additional cards can be ordered through BCBSOK preventive care services are covered at 100% of allowed However, your plan documents may contain exceptions customer service or by logging in to the Blue Access for amount, including routine OB/GYN exams and mammograms, to this list based on state mandates, the plan design or MembersSM (BAM) website at bcbsok.com/ou. and well child immunizations. rider(s) purchased. Visit the “Benefits” section of the OU HR With the BlueEdge HSA plan, a specific amount of money is n deposited each benefit year in a health savings account (HSA). When you need any covered medical care, the first out-of-pocket costs you have can be paid from available funds in this account. The money paid from your health account is applied toward meeting your annual plan deductible or other copayment or coinsurance amounts you may be responsible for. Benefits n You do not have to select a primary care physician, and you n n providers that are covered under the BlueEdge HSA is the Blue n As an HSA member, you have access to an extensive network of providers and hospitals throughout the country. You can n Services that BCBSOK determines are experimental/ Group Number Effective Date Subscriber: BenefitQ. Network John Sample Plan Name Any condition to the extent payment would have been made Office Visit Copay: The University of Oklahoma Specialist Copay: Identification Number: Rx Copay: Group Number Effective Date Benefit Network Office Visit Copay: ABC12345678 Specialist Copay: Rx Copay: Diagnosis, treatment or medications for infertility and fertilization procedures, including artificial insemination; ovulation induction www.bcbsok.com/OU procedures; in vitro fertilization; embryo transfer. (Coverage for level of benefits and lowest out-of-pocket costs. When you infertility is limited to diagnosis and treatment of underlying receive care from an out-of-network provider, you receive a www.bcbsok.com/OU cause.) lower level of benefits. The amount the plan pays for covered n Certificate of Benefits. If an out-of-network provider charges more than the allowed amount, you may have to pay the The University of Oklahoma Identification Number: claimed Medicare benefits a Blue Choice PPO network provider, you receive the highest services is based on the allowed amount described in the John Q. Sample under Medicare if the member had applied for Medicare and select any provider for care within the Blue Choice PPO network or outside the network. When you receive care from Subscriber: ABC12345678 investigational in nature Choice PPO network. n Charges above the allowed amount for out-of-network services The HSA plan that Blue Cross and Blue Shield of Oklahoma offers is called BlueEdge HSA. However, the network of Plan Name website for plan-specific information at hr.ou.edu. Cosmetic surgery or complications resulting there from, including surgery to improve or restore your appearance n Reverse sterilization n Treatment of sexual problems not caused by organic disease n Foot care only to improve comfort or appearance, such as care difference. for flat feet, subluxation, corns, bunions (except capsular and Customer Service Preauthorization Provider Locator 24/7 Nurseline RX Tech Support RX Cust Svc* 1-800-XXX-XXXX 1-800-XXX-XXXX 1-800-XXX-XXXX 1-800-XXX-XXXX 1-877-XXX-XXXX 1-877-XXX-XXXX Customer Service Preauthorization Provider Locator 24/7 Nurseline RX Tech Support RX Cust Svc* 1-800-XXX-XXXX 1-800-XXX-XXXX 1-800-XXX-XXXX 1-800-XXX-XXXX 1-877-XXX-XXXX 1-877-XXX-XXXX L13 L13 bone surgery), calluses, toenails, etc n Acupuncture, whether for medical or anesthesia purposes except for services in relation to tobacco cessation n Massage Therapy If you lose or misplace your ID card, you can print a temporary ID card and order a replacement card by logging in to Blue Access for Members (BAM) at bcbsok.com/ou. 9 8 Tools for Healthy Living Blue Care Connection Well onTarget® – A Dynamic Wellness Program Through the Blue Care Connection program, you’ll find tools and At Blue Cross and Blue Shield of Oklahoma, we believe in supporting your health and well-being. Well onTarget offers personalized tools and resources to help all members— no matter where you may be on the path to health and wellness. Program highlights include: onmyway Health Assessment (HA) The HA features adaptable questions to learn more about you. onmywayTM Health Assessment n onmytime Self-directed Courses on topics such as healthy eating, stress, weight management and fitness n Health and Wellness content n Tools and Trackers such as a food diary n Blue PointsSM program participate call BCBSOK customer service. There is also a tobacco cessation benefit described on the plan comparison Support for a slimmer, healthier you chart. The program offers guidance and support through behavioral and 24/7 Nurseline Your answers will be used to tailor the Liveon portal with the Blue Points n discounts for wellness-related products and services. To The confidential record offers tips for living your healthiest life. The Liveon portal is the heart of the Well onTarget program. offers you a gateway to a suite of interactive programs: The program provides personal coaching, online tools and Weight Management programs that may help you reach your goals. online courses, tools and trackers. Leading-edge technology to wellness. Support for tobacco users who want to quit After you take the HA, you will get a personal wellness report. Liveon Member Wellness Portal It inspires and supports you through healthy living programs, services that inform, support and motivate you on your journey Tobacco Cessation With the Blue Points program, you can earn points by taking part motivational coaching, personalized goal setting with an action plan, online tools and discounts to wellness-related products and services. To get started, call BCBSOK customer service. in healthy activities. This program makes it easy for you to track Fitness Program your points from 1 screen. Real-time granting of points lets you Join a network of gyms instantly use your points. Points can be redeemed for a host of products from the online shopping mall. To earn a larger reward, you can add to your point total at checkout. Well onTarget is a registered mark of HCSC. Blue Points Program Rules are subject to change without prior notice. See the Program Rules on the Well onTarget Member Wellness Portal for further information. Health concerns don’t always follow a 9-to-5 schedule. Fortunately, you can call the toll-free 24/7 Nurseline 24 hours a day, 7 days a week to get the information you need…when you need it. The 24/7 Nurseline is staffed by registered nurses who can Take advantage of a gym membership to a nationwide network answer your general health questions, direct you to your doctor of fitness centers. To get started, access the Well onTarget or encourage you to seek emergency services if necessary. A portal, or call BCBSOK customer service. nurse can help identify options and provide information to help you choose the appropriate care for your concerns. Plus, when you call, you also have the option to access an audio library of more than 1,000 health topics. Call the 24/7 Nurseline toll free at 800-581-0407. 10 11 Special Beginnings® – Maternity Program Biometric Screenings If you are expecting, this prenatal program can help guide you Biometric screenings will continue to be available to all OU through your pregnancy and postpartum care. The program employees in 2016. Please watch your email and employee provides support and education, pregnancy risk assessment and bulletin boards for more information on dates and locations. ongoing attention/monitoring. A biometric screening provides a detailed assessment of your Enrolled members receive frequent, personal contact from obstetrical nurses who can help them better understand and manage their pregnancies. Educational materials promote healthy behaviors, preventive care, and identify warning signs of complications. Topics also include nutrition, fetal development and newborn care. Additionally, members can call a 24-hour tollfree BabyLine staffed by maternity nurses. For more information or to enroll in Special Beginnings, call 877-904-2229. basic health indicators, including blood pressure, body mass and LDL) and blood glucose. This screening will give you an awareness of potential health conditions. Other Resources to Help You made available via bcbsok.com/OU. This is a good source of If you have certain chronic health conditions or are at risk for associations. You can learn about recommended screenings, and through regularly scheduled telephone calls, these registered recommendations set by national health agencies and medical nurses and other health care professionals can help you learn to Be Smart. Be Well.® is our website dedicated to raising manage your condition more successfully, identify behaviors that awareness of largely preventable health and safety issues. may be barriers to better health, set goals for improving your You’ll find in-depth information on a variety of issues, including health and help you adopt healthier habits. traumatic brain injuries, drug interactions and mental health at Case Managers In the event that you or a covered family member experiences multiple or complex medical problems, our case management nurses – registered nurses with specialized training and clinical experience – can work with you. At a time that’s usually stressful, case managers can be your advocate by: n Helping to explain your medical problem(s) and treatment plan(s) n Facilitating communication among your many health care providers n Coordinating a treatment plan(s) n Explaining your health care benefits and how to get the most out of them n n Helping you access the right resources and services Assisting with transitions from one health care setting to another Go to bcbsok.com/ou Blue Access for Members (BAM) Website provides: •Ability to print a temporary member ID card and order a new card •Claim Status •Find a doctor or hospital •Access to Well onTarget • Explanation of Benefits (EOB) Go to bcbsok.com/ou •Enter Blue Access for Members user ID and password •If you do not have a user ID and password, click on “Register Now” Blue Points Earn points, redeemable for rewards, for health-related activities Go to BAM at bcbsok.com/ou • Click on Well onTarget Locate a Health Care Provider Find a doctor, specialist, or hospital in your area Go to bcbsok.com/ou • Click on your plan type in the Find a Doctor section OU Benefits website Find benefit related information Go to hr.ou.edu Pharmacy • • • • Go to myprime.com immunizations and doctor visits for all ages, from prenatal care and infancy through the senior years. HOW TO ACCESS • Log in to Blue Access for Members to access the Well onTarget portal or view claims • View/print benefit brochures • Locate a doctor or hospital health and wellness information. Preventive Health Care Guidelines are published each year and PURPOSE BCBSOK website for OU Blue Cross and Blue Shield of Oklahoma also provides other information on preventive care guidelines, which are based on offer health counseling, coaching and support. Working with you RESOURCE index (calculated from height and weight), cholesterol (HDL Blue Care AdvisorsSM medical complications, a Blue Care Advisor may contact you to ONLINE BENEFIT RESOURCES Compare drugs Find generic alternatives Obtain cost estimates View drug formulary besmartbewell.com. Glucose Meters help members with diabetes manage their condition and can be ordered at no charge. For information on available meters and how to place an order, call customer service. Start your journey to wellness today! Prime Therapeutics LLC, a separate company, is a pharmacy benefit management company. Blue Cross and Blue Shield of Oklahoma (BCBSOK) contracts with Prime Therapeutics to provide pharmacy benefit management and other related services. In addition, contracting pharmacies are contracted through Prime Therapeutics. The relationship between BCBSOK and contracting pharmacies is that of independent contractors. BCBSOK, as well as several other independent Blue Cross and Blue Shield Plans, has an ownership interest in Prime Therapeutics. 12 Plan Comparison Chart 13 The amounts shown below are what you are responsible for paying for each type of service or treatment. Coverage BlueLincs HMO BlueOptions Traditional Indemnity†† BlueEdge HSA HMO Network Only Blue Preferred PPO Network Blue Choice PPO Network Out-of-Network Blue Choice PPO Network Out-of-Network No Network Calendar Year Deductible Individual/Family $300 per person $400/$800 $500/$1,000 $1,000/$2,000 $1,500/$3,000 $2,500/$5,000 $300 Out-of-Pocket Maximum Individual/Family $2,000/$4,000 Includes deductible & medical copay amounts $3,000/$6,000 Includes deductible & medical copay amounts $3,000/$6,000 Includes deductible & medical copay amounts $4,000/$8,000 Includes deductible & medical copay amounts $3,000/$6,000 Includes deductible & medical/pharmacy copay amounts $5,000/$10,000 Includes deductible & medical/pharmacy copay amounts $3,000/$6,000 Unlimited Unlimited Unlimited Unlimited Unlimited Unlimited Unlimited $25 copay per visit ($35 copay for specialist) $20 copay per visit ($30 copay for specialist) 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Physical, Occupational, Speech, and Chiropractic Therapies (60 visit maximum combined for all therapies) $35 copay $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Allergy Injections $25 copay $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Allergy Testing $35 copay $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Allergy Serum Covered at 100% of allowed amount $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Inpatient Physician Services Subject to deductible then Covered at 100% of allowed amount 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Outpatient Physician Services / non-routine office services Subject to deductible and applicable copay 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Routine Exam Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30% after deductible Covered at 100% of allowed amount 40% after deductible Covered at 100% of allowed amount Adult Immunizations Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount Covered up to the allowed amount† Covered at 100% of allowed amount Covered up to the allowed amount Covered at 100% of allowed amount Well Child Exams Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30% after deductible† Covered at 100% of allowed amount 40% after deductible Covered at 100% of allowed amount Routine Eye Exam* (does not include hardware) $25 copay $30 copay $35 copay 30% after deductible† Covered at 100% of allowed amount 40% after deductible Covered at 100% of allowed amount Routine Hearing Exam* (does not include hardware/hearing aids) $25 copay $30 copay $35 copay 30% after deductible† Covered at 100% of allowed amount 40% after deductible Covered at 100% of allowed amount Routine Ob/Gyn Exam Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount Covered up to the allowed amount† Covered at 100% of allowed amount Covered up to the allowed amount Covered at 100% of allowed amount Routine Mammograms Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount Covered up to the allowed amount† Covered at 100% of allowed amount Covered up to the allowed amount Covered at 100% of allowed amount Routine Prostate Specific Antigen (PSA) Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30%, no deductible Covered at 100% of allowed amount 40%, no deductible Covered at 100% of allowed amount Routine Colonoscopy Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30% after deductible† Covered at 100% of allowed amount 40% after deductible Covered at 100% of allowed amount Well Child Immunizations Covered at 100% of allowed amount CoCovered at 100% of allowed amount Covered at 100% of allowed amount Covered up to the allowed amount† Covered at 100% of allowed amountt Covered up to the allowed amount† Covered at 100% of allowed amount Lifetime Health Care maximum (per person) PHYSICIAN SERVICES Office visit & related routine services / consultation / second opinion Lab & X-ray (Physician Office) $25 copay per visit ($35 copay for specialist) PREVENTIVE CARE SERVICES *Routine vision and hearing exams limited to once every 24 months. † Up to the allowed amount. If an out-of-network provider charges more than the allowed amount, you may be responsible for the difference. †† Medicare Part A and Part B coverage is required. 14 15 The amounts shown below are what you are responsible for paying for each type of service or treatment. Coverage BlueLincs HMO BlueOptions Traditional Indemnity†† BlueEdge HSA HMO Network Only Blue Preferred PPO Network Blue Choice PPO Network Out-of-Network Blue Choice PPO Network Out-of-Network No Network Inpatient Hospital Subject to deductible and $250 copay per admission 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Outpatient Surgery Subject to deductible and $100 copay per surgery 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Emergency Room Subject to deductible and $100 copay per visit – copay waived if admitted 20% after $100 copay and deductible 20% after $100 copay and deductible 20% after $100 copay and deductible 15% after deductible 40% after deductible† 20% after deductible $50 copay 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Subject to deductible and $250 copay per admission 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible No limit 90 days per calendar year, combined in- and out-of-network 90 days per calendar year, combined in- and out-of-network 90 days per calendar year, combined in- and out-of-network 90 days per calendar year, combined in- and out-of-network 90 days per calendar year Subject to deductible then Covered at 100% of allowed amount 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible No limit 120 days per calendar year, combined in- and out-of-network 120 days per calendar year, combined in- and out-of-network 120 days per calendar year, combined in- and out-of-network 120 days per calendar year, combined in- and out-of-network 120 days per calendar year, combined in- and out-of-network 120 visits per calendar year Subject to deductible then Covered at 100% of allowed amount 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible No limit 70 visits per calendar year, combined in- and out-of-network 70 visits per calendar year, combined in- and out-of-network 70 visits per calendar year, combined in- and out-of-network 70 visits per calendar year, combined in- and out-of-network 70 visits per calendar year, combined in- and out-of-network 70 visits per calendar year Subject to deductible plus $250 copay 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Subject to deductible then Covered at 100% of allowed amount 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible $35 copay for initial visit then no charge $20 copay/$30 copay for specialist for initial visit; all other services 20% after deductible $25 copay/$35 copay for specialist for initial visit; all other services 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Subject to deductible and $250 per admission 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Covered with applicable copay $20 copay per visit ($30 copay for specialist) $25 copay per visit ($35 for specialist) 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Voluntary Sterilization ( Subject to deductible and applicable copay 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Pregnancy Termination (therapeutic & non-therapeutic) Subject to deductible and applicable copay 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Covered with applicable copay Covered with applicable copay Covered with applicable copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible HOSPITAL SERVICES Urgent Care Facility EXTENDED CARE INPATIENT/HOME Skilled Nursing Facility Skilled Nursing Facility Maximum Home Health Home Health Maximum Private Duty Nursing Private Duty Nursing Maximum Hospice - Inpatient (no benefit limit) Hospice - Outpatient (no benefit limit) 90 days per calendar year, combined in- and out-of-network MATERNITY & FAMILY PLANNING Prenatal & Postnatal visits Inpatient Hospital Infertility Testing & Treatment ( Contraceptive Devices † Up to the allowed amount. If an out-of-network provider charges more than the allowed amount, you may be responsible for the difference. Medicare Part A and Part B coverage is required. †† 17 16 The amounts shown below are what you are responsible for paying for each type of service or treatment. Coverage BlueLincs HMO BlueOptions HMO Network Only Blue Preferred PPO Network Blue Choice PPO Network Subject to deductible and $250 copay per admission†††† 20% after deductible $35 copay†††† Traditional Indemnity†† BlueEdge HSA Out-of-Network Blue Choice PPO Network Out-of-Network No Network 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Subject to deductible and $250 copay per admission†††† 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible $35 copay†††† $30 copay $35 copay 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible $10/$30/$60 $10/$30/$60 $10/$30/$60 30% after $10/$30/$60† 15% after deductible 40% after deductible† $8/$35/50% ($100 minimum; $200 maximum) MENTAL HEALTH Inpatient Hospital/Facility Outpatient Charges SUBSTANCE ABUSE Inpatient Hospital/Facility Outpatient Charges PRESCRIPTIONS Retail Pharmacy Care Generic (Tier I)/Preferred Brand (Tier II)/ Non-Preferred Band (Tier III) (30 day supply with one copay or 31-90 day supply with two copays) $20/$60/$120 $20/$60/$120 $20/$60/$120 Not covered 15% after deductible Not covered Preferred Pharmacies††† $16/$70/50% ($100 minimum; $200 maximum) out-of-network not covered Specialty Pharmacy Medications (limited to 30 day supply) Covered Covered Covered Covered up to the allowed amount† Covered 40% after deductible† Covered Prescription Tobacco Cessation Products Covered Covered Covered Covered up to the allowed amount† Covered 40% after deductible† Covered Individual/Family Out-of-Pocket Maximum $1,000/$2,000 Includes pharmacy copay amounts $1,000/$2,000 Includes pharmacy copay amounts $1,000/$2,000 Includes pharmacy copay amounts $1,000/$2,000 Includes pharmacy copay amounts N/A Pharmacy and Medical Out-of-Pocket are combined N/A Pharmacy and Medical Out-of-Pocket are combined N/A Covered Covered Covered Covered up to the allowed amount† Covered 40% after deductible† Covered Not covered Covered Covered Covered up to the allowed amount† Covered 40% after deductible† Not covered Diabetic Supplies – Most Covered Covered Covered Covered up to the allowed amount† Covered 40% after deductible† Covered* Step Therapy – Applies Applies Applies Applies Applies Applies Applies Pre-Authorization – Applies Applies Applies Applies Applies Applies Applies Subject to deductible and $100 copay per occurrence 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Covered at 100% of allowed amount Covered at 100% of allowed amount Covered at 100% of allowed amount 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Applies Applies Applies Applies Applies Applies Applies Covered (subject to BCBSOK medical policy criteria) Not covered Not covered Not covered Not covered Not covered Not covered Subject to deductible then Covered at 100% of allowed amount 20% after deductible 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible Covered at 100% of allowed amount Covered at 100% of allowed amount Covered up to the allowed amount† 15% after deductible 15% after deductible† 20% after deductible 30% after deductible† 15% after deductible 40% after deductible† 20% after deductible ESN/Mail Order RX Generic (Tier I)/Preferred Brand (Tier II)/Non-Preferred Band (Tier III) (90 day supply) Oral Contraceptives Sexual Dysfunction Drugs (limited to eight doses per 30 days no mail order) OTHER SERVICES & SUPPLIES MRI, CT, PET, EEG, and other similar imaging tests Diagnostic Lab & X-ray Tobacco Cessation Benefit (non-RX) – 100% member reimbursement for over-the-counter medications, acupuncture, hypnosis, stop smoking aids, etc., to a maximum of 20 visits/services per calendar year (per person) Bariatric/Weight Loss Surgery Durable Medical Equipment Ambulance (Ground/Air) Routine Audiological Exam Covered at 100% of allowed amount $25 copay Up to the allowed amount. If an out-of-network provider charges more than the allowed amount, you may be responsible for the difference. Medicare Part A and Part B coverage is required. †††† Please see Annual Notice of Change (ANOC) for non-preferred pharmacy coverage. †††† These services are coordinated though Magellan. Please contact 877-794-0678 † †† $30 copay $35 copay 18 CONTACTS This enrollment guide highlights OU’s Benefits Program. A complete description of each benefit can be found in your Certificate of Benefits Booklet or Member Handbook. Every effort has been made to provide an accurate summary of the plans in this guide. However, if there is a conflict between this material and the Certificate of Benefits or Member Handbook, the Certificate of Benefits Booklet or Member Handbook will govern. If you have any questions after reviewing your enrollment materials, please contact BCBSOK customer service at the phone numbers below. SUBJECT CONTACT BCBSOK Customer Service 888-881-4648 Pharmacy 800-423-1973 BlueCard 800-810-BLUE (2583) 24/7 Nurseline 800-581-0407 Special Beginnings 877-904-2229 Through It All. Through It All.® bcbsok.com A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association Blue Cross®, Blue Shield® and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. 70450.1015