Oxford University Hospitals NHS Foundation Trust
advertisement
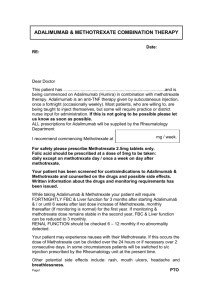
Oxford University Hospitals NHS Foundation Trust METHOTREXATE FOR USE IN Ophthalmology Shared care protocol This protocol provides prescribing and monitoring guidance for methotrexate therapy. It should be read in conjunction with the shared care responsibilities, the Summary of Product Characteristics (SPC) available on www.medicines.org.uk/emc and the BNF. BACKGROUND FOR USE Methotrexate (MTX) is a folic acid antagonist and is classified as an antimetabolite cytotoxic agent. It is prescribed for a wide range of conditions. It is also used as a disease modifying antirheumatic drug (DMARD) and as a steroidsparing agent. Indications, dose adjustments and monitoring requirements for DMARDs (licensed and unlicensed indications) defined in the Bucks shared care protocols are in line with national guidance published by the British Society for Rheumatology (BSR), the British Association of Dermatologists (BAD), the British Society of Gastroenterology ((BSG) and British Thoracic Society (BTS) (see references). The NPSA alert on improving compliance with oral methotrexate8 recommends the use of shared care guidelines based upon the BSR/BAD guideline. Methotrexate uses in this protocol are limited to: Ophthalmology For use in Ophthalmic conditions associated with rheumatological conditions. See below Scleritis Uveitis syndromes RHEUMATOLOGY Active rheumatoid arthritis (licensed): - It is commonly used as a first line treatment for this indication. - It can be used with other DMARDs such as leflunomide, sulfasalazine and hydroxychloroquine to achieve disease remission. - Parenteral methotrexate is licensed for rheumatoid arthritis and can be administered subcutaneously or intramuscularly. Other rheumatic conditions including psoriatic arthritis, early undifferentiated arthritis, juvenile idiopathic arthritis (JIA), spondylarthropathies, SLE, myositis, mixed connective tissue disease, scleroderma, vasculitis and polymyalgia rheumatica. Use in these conditions is unlicensed and recommended by the British Society of Rheumatology1. SUPPORTING INFORMATION Methotrexate is an established drug with a known side effect profile. CONTRAINDICATIONS TO METHOTREXATE Pregnancy. Both female and male patients should use effective contraception while on methotrexate and for at least 4 months after stopping it. Breastfeeding. Significant renal disease (GFR <10 ml/min). Untreated folate deficiency, leucopenia, thrombocytopenia. Suspected local or systemic infection. Oxford University Hospitals NHS Foundation Trust RELATIVE CONTRAINDICATION TO METHOTREXATE Chronic liver disease, alcoholism. PRECAUTIONS Elective surgery – methotrexate can be continued. Caution for early detection of infection and complications. Alcohol intake should be limited (maximum 4 - 6 units a week). Renal impairment – reduce the dose. Avoid if GFR <30 ml/min. Chickenpox/shingles – stop methotrexate if proven infection. For those with exposure to chickenpox or shingles and no history of infection/vaccination, passive immunisation with VZIG should be carried out. Infections - treat infection vigorously. Give methotrexate unless symptoms significant. DOSAGE2, 3 Indication Severe psoriasis Ophthalmology/ Rheumatology indications (above) Inflammatory bowel disease Respiratory indications (above) Dose Initial dose: 2.5 mg to 7.5 mg weekly, increasing to 15 to 25 mg weekly depending on response. 6 Initial dose: 10 mg weekly , adjusted to 7.5 to 25 mg weekly depending on response. Oral and s/c doses are usually the same. Usual dose: 15 to 25 mg weekly. 6 Initial dose: 10 mg weekly , adjusted to 7.5 to 20 mg weekly depending on response. Ref 1, 4, 9 1, 4, 6, 7, 9 2, 4, 5 3 Prescribing points Prescriptions must state the form, strength, dose and directions in full. The use of ‘as directed’ in prescribing should be avoided. A specific dose must be applied to each prescription8. Oral methotrexate This is available as 2.5 mg and 10 mg tablets. The NPSA recommends that only one strength of tablet should be supplied to the patient and that this should remain consistent in order to avoid confusion. It is therefore recommended to standardise on multiples of the 2.5 mg tablet which also allows for dosing flexibility. The tablet strength should be recorded in the monitoring booklet8. There is no commercially available suspension. Parenteral methotrexate This is licensed for use in rheumatoid arthritis only. Consider using it by s/c administration and only on the advice of a specialist for: - Patients with severe GI side effects despite regular folic acid 5 mg, 6 days a week. - Non-responders to oral therapy after an 8 - 12 week trial in order to improve drug bioavailability. It is available as a pre-filled pen . In order for a patient to use the product under the care of the GP, he/she should be able to administer the injection. Training on self-administration will be given by the hospital specialist nurse. After 2 to 3 months of s/c injection the specialist will re-assess if the treatment is of benefit and should be continued. Disposal of sharps. Cytotoxic sharps boxes will be provided by the hospital specialist nurse on initiation of treatment when attending for the self-administration training. Once full, the sealed sharps boxes should be exchanged for a new box at the GP practice or, in exceptional pre-arranged circumstances, as part of a planned follow up clinical Oxford University Hospitals NHS Foundation Trust appointment to the rheumatology outpatient department. Patients are advised to return their boxes for disposal and replacement when full or approximately every 3 - 6 months. Folic acid Folic acid reduces the risk of hepatotoxicity and gastrointestinal side effects. For rheumatology and respiratory indications, folic acid should be prescribed routinely at a dose of 5 to 10 mg weekly, to be taken 2 days after methotrexate. Folic acid can be given more frequently but not on the day of methotrexate, up to 5 mg 6 times a week. For severe psoriasis, folic acid should be prescribed at a dose of 5 to 10 mg weekly, to be given 2 days after methotrexate. In inflammatory bowel disease, folic acid 5 mg is usually given daily for 2 to 3 days after the methotrexate, e.g. on days 3, 4 and 5 after the weekly methotrexate dose on day 1 (i.e. 3 x 5 mg weekly)4, 5. To aid monitoring folic acid usage, prescribe a quantity for the same duration of supply as methotrexate (e.g. four weeks). TIME TO RESPONSE Methotrexate can take between 6 weeks to 3 months to have a full effect. PRE-TREATMENT ASSESSMENT BY THE SPECIALIST FBC, LFT, U&E and eGFR. Chest X-ray if not done within the last 6 months. Lung function tests may be considered in smokers and patients with pre-existing lung disease. CRP or ESR for rheumatology patients. Procollagen 3 (P III NP) for patients with skin psoriasis. ONGOING MONITORING SCHEDULES Monitoring recommendations for the different indications are not the same because risk factors for methotrexate toxicity vary according to the patient population. Ophthalmology FBC, LFTs and U&Es 2 weeks after starting/ after any new change in dose and then monthly for 6. Thereafter, based on clinical judgement, consider reducing frequency of monitoring to every 2 to 3 months. If there are abnormalities in ALT, monitoring should be two weekly until blood tests stabilised Oxford University Hospitals NHS Foundation Trust SIDE EFFECTS 9 WBC <3.5 x 10 /l OR 9 Neutrophils <2 x 10 /l OR 9 Platelets <150 x 10 /l ACTION MCV >105 - 110 fl MCV >110 fl Check folate, B12 and TFT, and treat if appropriate. If WBC normal repeat in 4 weeks. Stop methotrexate and seek advice. Liver function tests 2 - 3 fold rise in ALT >3 fold rise in ALT Reduce the dose by 2.5 mg and repeat in 1 - 2 weeks. Withhold until discussed with specialist. Renal impairment Nausea Withhold and discuss with specialist. Patients who develop dehydration, pre-renal or acute renal failure while on methotrexate should have methotrexate withheld and FBC monitored closely. Review any changes in medication particularly ACEI and ARB. Usually improves over time. If troublesome consider: - Increasing the dose of folic acid to 5 mg daily up to 6 days a week - omitting on the day methotrexate is taken. - Splitting methotrexate dose over one evening and next morning. - A short-term anti-emetic. If unable to tolerate refer back to specialist for review. Hair loss Usually mild, rarely significant. Rash Withhold treatment and discuss with consultant. Mouth ulcers, mucositis Mouth ulcers may respond to increasing folic acid as above. If severe despite extra folic acid stop methotrexate and refer to a specialist for advice. Menstrual dysfunction/amenorrhoea May occur during treatment and for a short while after cessation. Otherwise unexplained dyspnoea or cough Methotrexate pneumonitis may occur. Withhold treatment, arrange chest X-ray and discuss urgently with consultant. Abnormal bruising Withhold until FBC result available. Sore throat or other unusual infection Urgent FBC and withhold until FBC result available. Please note that in addition to absolute values for haematological indices, a rapid fall or a consistent downward trend in any value should prompt caution and extra vigilance. In order to monitor trends, it is recommended that all blood test results are entered in the patient held monitoring booklet. DRUG INTERACTIONS (See SPC for full list http://www.medicines.org.uk/emc/.) Co-trimoxazole Trimethoprim Phenytoin (R) Malaprim (R) Fansidar Avoid co-prescribing: Increased anti-folate effect which may induce toxic effects of methotrexate on FBC. Non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin Under specialist advice this combination is not contraindicated. NSAIDs and aspirin may reduce tubular excretion of methotrexate and enhance its toxicity. Over-the-counter products containing NSAIDs or aspirin are NOT recommended. Ciclosporin Patients co-prescribed ciclosporin with methotrexate should initially be restabilised by the specialist as it can increase methotrexate toxicity. Live vaccines Avoid Oxford University Hospitals NHS Foundation Trust Leflunomide Although the BNF states that leflunomide is not usually used with methotrexate, it is appropriate to use the combination in rheumatoid arthritis 7 under specialists’ advice . There can be increased risks of side effects (e.g. liver and haematological), but with careful monitoring experience suggests they may be used together. NOTES One weekly dose of methotrexate can be withheld without inducing a flare. Annual ‘flu vaccination is recommended. Folinic acid (given as calcium folinate) should be used for methotrexate induced myelosuppression, severe mucositis or methotrexate overdose, in the initial dose 20 mg IV and followed by 15 mg qds orally until abnormalities improve.