Oxford Molecular Genetics Laboratory
advertisement

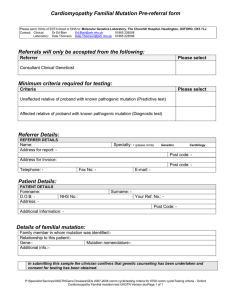
Oxford Molecular Genetics Laboratory Genetics Laboratories, Churchill Hospital, Old Road, Headington, Oxford, OX3 7LE www.ouh.nhs.uk/geneticslab FAMILIAL BENIGN HYPOCALCIURIC HYPERCALCAEMIA (FHH) OMIM: 145980/145981/600740 INTRODUCTION Familial benign hypocalciuric hypercalcaemia is an autosomal dominant disorder of extracellular calcium homeostasis, characterised by lifelong hypercalcaemia with inappropriately low urinary calcium excretion (mean urinary calcium:creatinine clearance ratio <0.01) Identification of pathogenic variants in the genes responsible for FHH can confirm the diagnosis based on clinical/biochemical presentation. This can assist in directing patient management and whether surgical intervention is required. It is a genetically heterogeneous condition where the types are clinically indistinguishable. To date the following genes have been identified as causative of FHH: CASR: Pathogenic loss of function mutations in the CASR gene account for FHH type1 (FHH1). ~65% of individuals with definite FHH are reported to have a pathogenic variant in this gene. GNA11: pathogenic variants in this gene are causative of FHH type 2 (FHH2). Nesbit et al, 2013, NEJM, identified pathogenic GNA11 variants in >10% CASR & AP2S1 negative FHH patients (although the cohort tested was small). AP2S1: The molecular basis of FHH type 3 (FHH3) has been identified as mutation of codon p.Arg15 of the AP2S1 gene. >20% of CASR negative FHH patients have this mutation (Nesbit et al, Jan 2013, Nature Genetics). TESTING Diagnostic: Presymptomatic/confirmation: Patients with a consistent “Clinical/Biochemical diagnosis”. Individuals at risk of developing FHH/ relatives of individuals in whom a pathogenic variant has been identified. REFERRALS All samples MUST be accompanied by a completed ‘Hypercalcaemia and Hyperparathyroidism’ pre-referral form (click here) o Clinical guidance is available from Professor Rajesh Thakker, Professor of Medicine, OCDEM, Churchill Hospital (rajesh.thakker@ndm.ox.ac.uk). o UK diagnostic referrals are accepted from Clinical Genetics, Endocrinology and consultants from other relevant specialties. o Familial mutation referrals should ideally be referred through/in collaboration with Clinical Genetics departments. o Requests for familial mutation testing should either be discussed with the laboratory in advance or be accompanied by details regarding the known pathogenic mutation in the family. STRATEGY & TECHNICAL INFORMATION o Mutation screening in diagnostic referrals is undertaken by fluorescent sequencing of the entire coding region and intron/exon boundaries of the selected gene (CASR and GNA11), or specific analysis of codon p.Arg15 in AP2S1. o Testing can be undertaken sequentially or simultaneous analysis of the 3 genes is available. o When a pathogenic mutation has been identified in an individual, subsequent testing of family members (presymptomatic or diagnostic confirmation) involves testing for the familial mutation only. TARGET REPORTING TIMES Diagnostic test: Presymptomatic/Familial Mutation test: 40 days 10 days N.B. Details are correct for the date of printing only – last updated 14/07/2015