Nursing Home Quality as a Public Good David C. Grabowski Jonathan Gruber
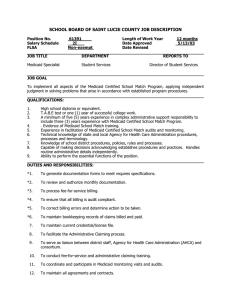
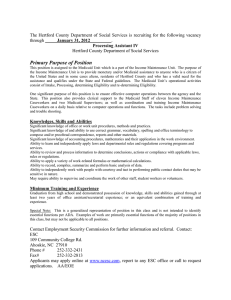
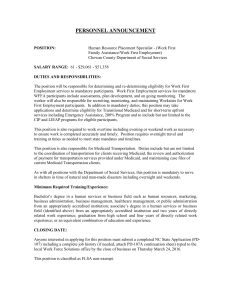
advertisement

Nursing Home Quality as a Public Good David C. Grabowski Harvard Medical School Joseph J. Angelelli Pennsylvania State University Jonathan Gruber Massachusetts Institute of Technology Medicaid and Private-pay prices, 1998 160 140 120 100 $ 80 60 40 20 0 KS ME MS ND OH SD WA Uniform Quality Assumption • Most economists have assumed that quality is uniform within facilities across payer types – – – – Federal law prohibiting discrimination by payer type Economies of joint production Professional norms Lack of individual data • If this is the case, Medicaid can free-ride on private-payers – Studies find association between payer mix and quality. Criticisms of uniform quality assumption • Oversight of federal law very difficult • Economies of joint production not relevant for most direct patient care activities – e.g., assisting residents with bathing, dressing, eating, toileting, and walking Our Contribution • To test whether quality is uniform across Medicaid and private-pay patients within nursing homes. – We use a range of process and outcome based measures of quality – We exploit both within-home and within-person variation in payer type and quality – We exploit Medicaid-private pay rate differentials across states Data • Minimum Data Set (MDS) surveys from KS, ME, MS, ND, OH, SD & WA – MDS collected at least quarterly for all patients, 1998 (4th qtr) thru 2002 – Data combines existing patients with new admissions – Eliminate short-stay Medicare patients – Total sample: 1,626,628 assessments for 359,768 patients from 1,537 facilities. • Facility information from OSCAR system • Rates collected from state Medicaid cost reports Quality Measures • • • • • • Pain Pressure ulcers Physical restraints Incontinence Catheters Bedfast • • • • • • Anti-psychotics Feeding Tubes Urinary tract infection Wound infection Falls Depression Methods (cont.) NH fixed effects model Yint = α + β1MEDICAIDint + β2OTHERint + δXint + γZnt + αt + λn + εint Patient fixed effects models Yint = α + β1MEDICAIDint + β2OTHERint + δXint + γZnt + αt + μi + εint Timing of the Medicaid Effect Yint = α + Σ-k<j<m θj MEDICAIDjint + β1OTHERint + δXint + γZnt + αt + μi + εint • Replace Medicaid dummy with three lead (or greater) and three (or greater) lag transition terms in the patient-level fixed effects model. • Restrict model to only those individuals observed 7+ periods and excludes Medicaid transitions with fewer than 3 assessments pre- and post-transition Outcome Facility FEs Patient FEs Dep Var Mean Pain 0.008 (11.76) -0.009 (7.64) 0.13 Pressure ulcers -0.007 (12.38) -0.011 (11.10) 0.08 Restraints -0.002 (4.75) 0.006 (7.21) 0.09 Incontinence 0.018 (24.25) 0.013 (11.86) 0.54 Catheters -0.010 (20.24) -0.014 (23.11) 0.08 Bedfast -0.002 (4.24) -0.007 (11.60) 0.06 Anti-psychotics 0.009 (8.67) 0.005 (3.68) 0.19 Feeding tubes -0.002 (3.99) -0.008 (19.83) 0.07 Urinary infection -0.004 (6.62) -0.013 (11.49) 0.09 Wound infection -0.003 (13.58) -0.004 (9.92) 0.02 Falls -0.022 (31.82) -0.019 (14.07) 0.16 Depression 0.034 (36.79) 0.023 (23.25) 0.43 Transition Results: Total Sample Period T-3+ T-2 T-1 Transition T+1 T+2 T+3+ Incontinence -0.006 (0.99) -0.00004 (0.01) 0.003 (0.51) 0.004 (0.54) 0.001 (1.65) 0.014 (2.15) 0.014 (2.23) Depression -0.008 (1.48) 0.0003 (0.05) 0.004 (0.74) 0.009 (1.56) 0.015 (2.50) 0.017 (2.84) 0.014 (2.52) Transition Results: New Admits Only Period T-3+ T-2 T-1 Transition T+1 T+2 T+3+ Incontinence 0.006 (0.63) 0.010 (1.05) 0.008 (0.84) 0.007 (0.76) 0.015 (1.58) 0.017 (1.75) 0.017 (1.84) Depression -0.006 (0.75) 0.011 (1.25) 0.013 (1.49) 0.019 (2.27) 0.025 (2.94) 0.025 (2.98) 0.021 (2.52) Alternate Specification • Another potentially exogenous source of variation is the difference between the private-pay price and Medicaid • Larger rate differential should entail worse Medicaid quality • Thus, we examine a model that interacts the ratio of rates (Medicaid/private-pay) with payer source • Results do not support differential quality Conclusions • The results support the uniform quality assumption used in most economic studies of the NH sector – Little evidence of a Medicaid causal effect • There is the potential for “free ridership” on the part of state Medicaid programs • Segregation by payer type – “Driven to tiers”