Tibial Posterior Tendon Dysfunction MD
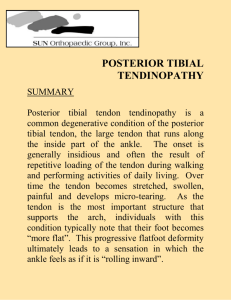
advertisement

Journal of Orthopaedic & Sports Physical Therapy 2OOO;3O (2) :68-77 Posterior Tibial Tendon Dysfunction William M. Geideman, MD )effrey E. )ohnson, MD Posterior tibial tendon dysfunction is the most common cause of acquired flatfoot deformity in adults. Although this term suggests pathology involving only the posterior tibial tendon, the disorder includes a spectrum of pathologic changes involving associated tendon, ligament, and joint structures of the ankle, hindfoot, and midfoot. Early recognition and treatment is the key to prevention of the debilitating, long-term consequences of this disorder. Conservative care is possible in the earliest stages, whereas surgical reconstruction and eventually arthrodeses become necessary in the latter stages. The purpose of this article is to review the symptoms, physical examination, radiological examination, classification, and treatment of posterior tibial tendon dysfunction. / Orthop Sports Phys Ther 2000;30:6877. Key Words: flatfoot, pes planovalgus, posterior tibial tendon dysfunction, tendinitis Holmes and MannI7 found that 60% of patients with rupture of the posterior tibial tendon had 1 or more of the following associated conditions: hypertension, obesity, diabetes mellitus, previous surgery or trauma about the medial aspect of the foot, or exposure to steroids. Local injections of steroids near the posterior tibial tendon have also been reported as a cause of HISTORY osterior tibial tendon dysfunction is the major cause of acquired flatfoot deformity in adults. The later stages of the disorder are characterized by increased heel valgus, plantarflexion of the talus, flattening of the medial longitudinal arch, and abduction of the forefoot at Chopart's joint. Posterior tibial tendon dysfunction includes a broad range of progressive disorders, ranging from tenosynovitis to tendon rupture with or without hindfoot collapse to a fixed, rigid, flatfoot deformity. The causes of posterior tibial tendon dysfunction are varied. They include age-related degeneration or overuse with attenuation, chronic recurrent tenosynovitis, inflammatory arthritides,';"' and, infrequently, An association with seronegative spondyacute traumatic rupture.1J.21.34 loarthropathy (ie, Reiter's syndrome, ankylosing spondylitis, and psoriatic arthritis) was found in one series in 47 of 76 patientsJ2 Most r u p tures are the result of an intrinsic abnormality of the tendon. There is a zone of hypovascularity in the region of the medial malleolus that is the most common site of rupture,'" but this does not explain the reason for rupture proximal to the malleolus or at the navicular insertion. The prevalence of rupture is increased in middle-aged, obese women.ll.lY27.33 It is uncommon to see ruptures in young patients, except for acute tra~maticrupture^.".".^'.^!'^^^ Most patients present with a history of insidious onset of unilateral acquired flatfoot deformity, as only 50% can recall a history of some form of ua~ma.~"ymptoms may be present for months or years. Bilateral posterior tibial tendon dysfunction is rare. Early symptoms include pain and swelling along the medial foot and ankle, pain in the plantar medial arch, and occasionally pain radiating into the medial proximal calf. Patients find standing on their toes painful and difficult. Over time, patients note a gradual worsening of their condition, with progressive collapse of the medial longitudinal arch. With the development of severe hindfoot valgus, they may perceive that they are walking on their medial ankle. Chief resident, Department of Orthopaedic Surgery, Washington University School of Medicine, St They frequently report abnormal Louis, Mo. wear of the sole of their shoe. Chief, Foot and Ankle Service, and Associate professor, Department of Orthopaedic Surgery, - . WashWalking increases the pain, and ington University School of Medicine, St, louis, Mo. Send correspondence to William M. Geideman, 10651 Steppington Drive, Apt 5052, Dallas, TX they note earlier fatigue and a decrease in their e n d ~ r a n c e . ' ~ 75230. E-mail: ifixbone@aol.com FIGURE 1. (A) Stage I posterior tibial tendon dysfunction. Note swelling posterior to the medial malleolus. (B)Single limb heel rise. Patient with stage 1 disease is able to perform this with normal inversion of the heel on the right. In the final stages, the planovalgus deformity progresses. Pain will shift laterally because of calcaneofib ular or lateral subtalar impingement, and medial pain frequently will d i ~ a p p e a r . ~ ~ PHYSICAL EXAMINATION Early in the development of posterior tibial tendon dysfunction, swelling and fullness in the posteromedial ankle is common. With an established flatfoot deformity, the involved foot will be abducted and will have lost the longitudinal arch. When viewing the standing patient from behind, the examiner will note the increased hindfoot valgus and the appearance of the "too many toes sign." This sign, originally described by Johnson,"' indicates that with advanced forefoot abduction, more toes will be visible on the affected side laterally. The single limb heel rise tesf"' is a sensitive indicator of posterior tibial tendon dysfunction. This is performed by asking patients to stand near a wall, gently balancing themselves with their arms forward and their hands resting on the wall. Patients then flex the knee of one leg, lifting the opposite foot off the ground, and then attempt to rise up onto the ball of the affected foot. With posterior tibial tendon dysfunction, inversion of the heel is weak or absent, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If able to perform this test, the patient may note medial ankle pain. Repetitive heel rises may reveal a subtle weakness of the tendon."4 With the patient seated, the posterior tibial tendon J Orthop Sports Phys Ther-Volume 30. N~unber2. Febnvaly 2000 should be palpated from above the medial malleolus to its insertion onto the navicular to assess its integrity and to assess any pain or swelling from tenosynovitis. Lateral tenderness in the subfibular or sinus tarsi region indicates calcaneofibular abutment or subtalar arthritis. Another useful test for recognizing early posterior tibial tendon dysfunction is the first metatarsal rise sign. This test is performed by externally rotating the shank of the affected foot with 1 hand or passively aligning the heel of the affected foot into a varus position with the patient standing, full weight bearing on both feet. The head of the first metatarsal will rise in the presence of posterior tibial tendon dysfunction and will remain on the floor if posterior tibial tendon function is normal.'"his is caused by the loss of posterior tibial tendon function, resulting in flattening of the medial longitudinal arch and the consequent elongation of the supporting plantar medial ligamentous structures, in particular the caspsuloligamentous complex of the first metatarsalcuneiform joint. This allows the gastrocnemius-soleus complex to act at the level of the first metatarsal head and cause dorsiflexion with weight bearing and external rotation of the shank of the foot or passive heel varus. The strength of the tendon is evaluated by asking the patient to attempt to invert the foot from a plantarflexed and everted position. This position isolates the posterior tibial tendon, neutralizing the synergistic inversion from the anterior tibialis m~scle.'"~The contralateral foot also should be tested in a similar fashion to determine the strength of the patient's nonimpaired ankle and to help identify a partial tear 70 J Orthop Sports Phys Ther .Voh~me30 -Number 2 - February 2000 FIGURE 2. Continued. based on comparative ~eakness.~' It is important to palpate the posterior tibial tendon behind the medial malleolus to feel it actively contract during inversion. An active, palpable contraction in a patient with an acquired flatfoot deformity puts the diagnosis of posterior tibial tendon rupture in doubt; tendonitis or partial rupture of the posterior tibial tendon or r u p ture of the spring or deltoid ligament then may be the cause of flatfoot deformityJJ Motion of the ankle and subtalar joints should also be evaluated. Ankle motion is usually normal, whereas subtalar motion becomes more limited as the dysfunction progresses. The subtalar joint may become fixed in valgus in cases of long-standing deformityaJ4 The amount of passive hindfoot inversion is an important variable in the selection of treatment and therefore should be assessed a c ~ u r a t e l y . ~ ~ Long-standing hindfoot valgus is often associated with an Achilles tendon c o n t r a ~ t u r eThis . ~ is assessed by dorsiflexing the ankle while holding the hindfoot in subtalar neutral position and the knee in extension. The relationship of the forefoot to the hindfoot should be assessed because as the hindfoot valgus worsens, the forefoot and midfoot assume a compensatory supinated position that may become fixed. This forefoot supination is evident as a forefoot varus posture. This, too, will affect selection of treatment, as well as the design of any foot o r t h o s i ~ . ~ ~ . ~ ~ PATHOLOGIC ANATOMY With attenuation or rupture of the posterior tibial tendon, the medial longitudinal arch of the foot coll a p s e ~and , ~ there is a relative internal rotation of the tibia and talus. The subtalar joint everts, causing the heel to assume a valgus position and the foot to abduct at the talonavicular joint. A compensatory forefoot varus deformity ensues. As the heel assumes an increased valgus alignment, the Achilles tendon becomes positioned lateral to the axis of rotation of the subtalar joint. Over time, the shortened position of the hindfoot results in an Achilles tendon contracture. As the deformity progresses, the fibula abuts against the lateral wall of the calcaneus, causing pain in the lateral hindfoot. CLASSIFICATION Johnson and Strom"' described the clinical stages of posterior tibial tendon dysfunction. In stage I (Figure I ) , the length of the tendon is normal, although mild degeneration is present. There is medial foot and ankle pain, swelling, and mild weakness, but no deformity. The single limb heel rise is painful, but normal. A flexible planovalgus foot characterizes stage I1 (Figures 2 and 3). The tendon is ruptured o r functionally incompetent and shows more advanced degeneration. The "too many toes sign" is FIGURE 2. (A) Stage I1 posterior tibial tendon dysfunction. Note the "too many toes sign" on the left foot with more toes seen laterally when viewing the patient from behind. Also, note the hindfoot valgus, which is more pronounced on the left side than the right. (B)Lateral radiograph of the same patient. Note the plantarflexedposition of the talar head. (C)Postoperative photograph of the same patient after a calcaneal osteotomy with medialization. Note the correction of the hindfoot valgus. (D) Postoperative radiograph showing 2-screw fixation of the calcaneal osteotomy and the improved pitch of the talus. J Orthop Sports Phys TheroVohme SO Number 29 Febn~aly2000 71 FIGURE 3. (A) Stage II posterior tibia1 tendon dysfunction. Again, note the hindfoot valgus and the "too many toes sign." (B) and (CI Patient treated with a short articulated AFO with correction of the hindfoot valgus. 72 1 Orthop Sport5 Phys Ther .Volume 30. Number 2. Febnran 2000 FIGURE 4. (A) Stage Ill posterior tibia1 tendon dysfunction. Note the medial hindfoot fullness and iixed valgus position. (BIPreoperative lateral radiograph showing severe transverse tarsal joint collapse and osteoarthritis of the subtalar and talonavicular joints. (C) Postoperative lateral radiograph aiter triple arthrodesis showing much improved midfoot and hindioot alignment. present, indicating secondary deformity of the midf~ot.~"he patient will be unable to perform a single limb heel rise, but the hindfoot remains flexible. In stage 111 (Figure 4), all the signs of stage I1 are present except that some component of the hindfoot deformity is fixed. In advanced disease, there may be lateral abutment pain at the calcaneal-fibular articulation. Stage IV (Figure 5 ) . alluded to by Johnson and Strom's article and later added to their classification by Myerson,J4 involves valgus tilt of the talus in the ankle mortise leading to lateral tibiotalar degeneration.Zl.J4 RADIOGRAPHIC EVALUATION Anteroposterior and lateral weight bearing radiographs of both feet, as well as radiographs of the ankle with the patient weight bearing should be o b tained. Early in the disease, radiographs may reveal normal findings or show minimal changes of angular deformity. As the clinical deformity progresses, charJ Orthop Sports Phys Ther*Voliime 30 Number 2. February 2000 acteristic radiographic changes occur. With increasing deformity, the anteroposterior view of the foot will show lateral subluxation of the talonavicular joint as the navicular rotates laterally on the talus, uncovering the talar head."','".:'!' There is an increase in the talo-first metatarsal angle, as well as an increase in the divergence of the talus and calcaneus.'!' The lateral view reveals a plantarflexion deformity of the talus, a decrease in the lateral talocalcaneal angle, the collapse of the longitudinal arch, a variable increase in the talo-first metatarsal angle, and sag at the talonavicular, naviculocuneiform, or metatarsalcuneiform joints.2" decrease in the distance from the medial cuneiform to the floor compared with the contralatera1 foot also has been de~cribed.~:' With advanced deformity, narrowing of the talonavicular and subtalar joints may be seen."' Anteriorposterior radiographs of the ankles with the patient standing may reveal tibiotalar arthritis, talar tilt, and calcaneofibular impingement in severe deformities. Magnetic resonance (MR) imaging is the method cally demonstrated on short-tau inversion recovery (STIR) images.% Ultrasound evaluation of the posterior tibial tendon is currently under investigation. Diagnostic ultrasound can detect changes in tendon size, the presence of fluid, and any intratendinous echogenic changes, thereby differentiating intratendinous and peritendinous structural changes. In addition, it is cheaper and faster than MR imaging, although significant skill and experience by the ultrasonographer is required to obtain the maximum amount of information from this t e ~ h n i q u e . ~ . ~ DIFFERENTIAL DIAGNOSIS FIGURE 5. Anteroposterior ankle radiograph of stage IV disease dernonstrating severe hindfoot valgus with osteoarthrosis and valgus tilt of the tibio-talar joint. of choice to evaluate pathologic conditions of the posterior tibial however, some controversy exists over the exact role of MR imaging in the treatment plan of patients with posterior tibial tendon dysfunction. '7344.JJ Conti et alqeveloped a classification scheme of tears of the posterior tibial tendon based on MR imaging. The classification takes into account structural features and abnormal signals within the substance of the tendon. In a type I tear, the MR image shows 1 or 2 fine, longitudinal splits in the tendon, often on the undersurface, without patterns of degeneration. T1 weighted images reveal a homogeneous black signal throughout the tendon. Type I1 tears are characterized by wider longitudinal tendon splits and intramural degeneration. These are seen as gray areas within the normally uniform black tendon. The tendon also may show variable diameter on selected cuts where a bulbous section may be distal to an attenuated portion. Type I11 tears are notable for more diffuse swelling and uniform degeneration of the tendon. A few tendon strands may remain, or the tendon may be replaced entirely with scar tissue. Complete ruptures with tendon gap are most graphi- The majority of adult acquired flatfoot deformities are the result of posterior tibial tendon dysfunction, but several conditions have a similar clinical presentati~n.'~:'~ Attenuation or rupture of the calcaneonavicular (spring) ligament complex including the talonavicular capsule will have a similar clinical presentation as posterior tibial tendon dysfunction. A strong voluntary contraction of the posterior tibial tendon on manual testing supports the diagnosis of spring ligament pathology. Degenerative arthritis of the ankle joint with valgus talar tilt places the hindfoot in marked valgus with midfoot pronation and leads to a flatfoot def~rmity.'~ Standing anterior-posterior radiographs of the ankle will rule out degenerative arthritis as a cause of adult acquired flat foot deformity. Arthritis of the talonavicular joint, spontaneous or after trauma, causes forefoot abduction deformity, collapse of the midfoot, and prominent callus formation on the plantar-medial aspect of the foot.'J Posttraumatic tarsometatarsal (Lisfranc) joint arthritis can present as an acquired flatfoot deformity. Usually the first, second, and third tarsometatarsal articulations are involved, and patients have painful osteophyte formation on the dorsal midfoot and progressive abduction and dorsiflexion of the forefoot on presentati~n.'~ Inflammatory arthritis of the hindfoot, usually secondary to rheumatoid disease, can cause valgus tilt at the ankle or subtalar joint instability. Lacerations of the posterior tibial tendon, although uncommon, have caused an acquired Neuroarthropathy, such as diabetes, as well as other peripheral neuropathies, may cause an acquired flatfoot deformity.'" TREATMENT Treatment is based on an accurate staging of the disease with both nonsurgical and surgical treatments designed to correct the abnormalities particular to that stage of disease and to prevent progression to the next stage. J Orthop Sports P h y Ther-Volume SOeNumber 29Febnlary 2000 FIGURE 6. A University of California, Berkeley Laboratories (UCBL) orthosis with medial posting. The goals of nonoperative treatment include the elimination of clinical symptoms, improvement of hindfoot alignment, and the prevention of progressive foot deformity. For stage I disease, nonsurgical treatment should be tried for at least 3 to 4 months. A short walking cast or removable cast boot immobilization is indicated for patients with acute tenosynov i t i ~ . ~ ~ If . Jsymptoms '.~~ are improved after immobilization, then a custom orthotic or ankle foot orthosis (AFO) may be fitted to the patient. The orthotic should be a full-length, semirigid, totalcontact insert with medial posting. The primary function of the orthotic is to provide arch support and correct the flexible component of the deformity. Physical therapy for Achilles tendon stretching and posterior tibia1 tendon strengthening is also b e n e f i ~ i a l . " Nonste~~~ roidal antiinflammatory medicine may decrease pain and associated swelling. Surgical treatment should be undertaken only after failure of nonsurgical measures. Surgically, a synovectomy will remove any hypertrophic tenosynovium. If a necrotic portion of the tendon is encountered, as evidenced by discoloration, attenuation, and longitudinal rents, this area may be excised and the remaining tendon repaired in an end-toend fashi ~ n . ~ " na study by Teasdall and Johnson4%th an J Orthop Sports Phys Ther-Volume SOeNumber 2.Febnla1-y 2000 average 30-month follow-up, 16 of 19 patients reported feeling "much better" after this procedure and 74% had complete relief of pain. This repair may be reenforced by means of a side-tu-side tenodesis to the adjacent flexor digitorum longus tendon.'JR+' In stage I1 disease, nonsurgical treatment involves an initial period of cast or removable cast boot immobilization or, in subacute cases, an AFO. Longterm nonsurgical treatment requires more rigid s u p port of the foot and ankle. This may be accomplished with an AFO, corrective total contact insert, o r a University of California, Berkeley Laboratories orthosis (UCBL) (Figure 6) .3 The UCBL functions to place the hindfoot in neutral and limit the motion of the subtalar joint. Many designs of AFO have been described for treatment of the flexible flatfoot deformity including a 1-piece molded polypropylene AFO, a short articulated AFO (Figure 3), a short lace-up leather (Figure 7), and a plastic AFO, as well as the traditional double upright AFO with T-strap. These all function to limit subtalar motion. In addition, shoe modifications such a medial flare, wedge, or stabilizer may be Surgical treatment of patients with stage I1 disease is controversial. There are many described procedures, each with only short-term follow-up and all . ~ ~ options for placement may be a p p r ~ p r i a t eOther treatment include a lateral column lengthening to recreate the medial longitudinal arch performed through the calcaneal neck, as described by Evans, or through the calcaneocuboid joint with subsequent f u s i ~ n . ~ Lengthening ."~~ through the calcaneal neck in adults has led to calcaneocuboid joint overload and early arthro~is.~' Lateral column lengthening may be performed alone or with a medial displace ment calcaneal osteotomy, thereby addressing both the pes planus deformity and the valgus deforming force of the Achilles t e n d ~ n . ~ ' Stage I11 disease (fixed deformity) is not passively correctable, and therefore, any nonoperative treatment will need to accommodate the deformity. Custom foot orthotics, shoes, and AFOs, may help alleviate pain and slow progression. Because the deformity is not passively correctable, tendon reconstruction alone is not helpful, and to correct the deformity, a subtalar or triple arthrodesis usually is performed. In stage IV, the tibiotalar joint is involved. Treatment thus involves a tibiotalocalcaneal, pantalar fusion, or hindfoot arthrodesis combined with bracing. CONCLUSION FIGURE 7. Short leather lace up ankle-ioot orthosis (AFO)with copolymer reinforcement medial and lateral for added support. Accurate diagnosis requires a high index of suspicion and an understanding of the physical signs, symptoms, and natural history of the acquired flatfoot deformity. Physicians must accurately stage the extent of the disease, as treatment depends on the stage and the response to nonsurgical therapy. with nearly equivalent outcomes. It is not within the scope of this article to discuss each of these treatREFERENCES ments thoroughly; instead, each will be presented 1. Alexander IJ,Johnson KA, Berquist TH. Magnetic resowith relevant articles referenced for further review. If nance imaging in the diagnosis of disruption of the posa large gap is present in the posterior tibial tendon, terior tibial tendon. Foot Ankle. 1987;8:144-147. the nonviable ends are resected, and a side-to-side 2. Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruptenodesis to the flexor digitorum longus tendon is tion of muscles and tendons: an analysis of 1,104 cases. perf~rrned.~~.~!'~:':~~.~~ If the tendon is torn off its inSurgery. 1959;45:406-414. 3. Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonopsertion into the navicular tuberosity, then nonviable erative management of posterior tibial tendon dysfunctissue is resected, and the tendon is advanced and tion. Foot Ankle Int. 1996;17:736-741. reinserted into the navicular by means of an anchor4. Clain MR, Baxter DE. Simultaneous calcaneocuboid and ing suture or by passing the tendon through a drill talonavicular fusion: long-term follow-up study. ) Bone hole and suturing it to itself. Transfer of the flexor joint Surg BE 1994;76B:133-136. 5. Conti S, Michelson J, Jahss M. Clinical significance of digitorum longus tendon through a drill hole in the magnetic resonance imaging in preoperative planning for navicular may also be required if the tendon is torn reconstruction of posterior tibial tendon ruptures. Foot off its insertion.'42i-:':' Some studies recommend that Ankle. 1992;13:208-214. at the time of tendon reconstruction, an evaluation 6. Conti SF. Posterior tibial tendon problems in athletes. Orof the spring ligament be performed and repair perthop Clin North Am. 1994;25:109-1 2 1. formed if there are signs of i n j ~ r y . ~Severe .~' defor7. Cracchiolo A. Evaluation of spring ligament pathology in patients with posterior tibial tendon rupture, tendon transmity with hindfoot subluxation or arthritis may refer, and ligament repair. Foot Ankle Clin. 1997;2:297quire isolated arthrodesis of the subtalar j~int,".~".:'~ 307. talonavicular joint,'.' or a double4 or triple arthrode 8. Deland JT, Otis JC, Lee KT, Kenneally SM. Lateral column ~ i s , :either '~ alone or in combination with tendon relengthening with calcaneocuboid fusion: range of motion pair. For severe hindfoot valgus with lateral impingein the triple joint complex. Foot Ankle Int. 1995;16:729733. ment, osteotomy of the calcaneus with medial disJ Orthop Sports Phys Ther.Volrme 30 Number 2 Febnraly 2000 9. Evans D. Calcaneovalgus deformity. J Bone Joint Surg Br. 1975;57B:270-278. 10. Frey C, Shereff M, Greenridge N. Vascularity of the posterior tibial tendon. J Bone Joint Surg. 1990;72A:884888. 11. Funk DA, Cass JR, Johnson KA. Acquired adult flat foot secondary to posterior tibial tendon pathology. J Bone Joint Surg. 1986;68A:95-102. 12. Gazdag A, Cracchiolo A. Posterior tibial tendon rupture: evaluation of spring ligament pathology and clinical assessment of tendon transfer and ligament repair. J Bone Joint Surg. 1997;79:675-681. 13. Goldner JL, Keats PK, Bassett FH Ill, Clippinger FW. Progressive talipes equinovalgus due to trauma or degeneration of the posterior tibial tendon and medial plantar ligaments. Orthop Clin North Am. 1974;5:39-51. 14. Harper MC, Tisdel CL. Talonavicular arthrodesis for the painful adult acquired flatfoot. Foot Ankle Int. 1996;17: 658-661. 15. Henceroth W D 11, Deyerle WM. The acquired unilateral flatfoot in the adult: some causative factors. Foot Ankle. 1982;2:304-308. 16. Hintermann B, Gachter A. The first metatarsal rise sign: a simple sensitive sign of tibialis posterior tendon dysfunction. Foot Ankle Int. 1996;17:236-241. 17. Holmes GB Jr, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992;13:70-79. 18. Jahss MH. Spontaneous rupture of the tibialis posterior tendon: clinical findings, tenographic studies, and a new technique of repair. Foot Ankle. 1982;3:158-166. 19. Johnson KA. Tibialis posterior tendon rupture. Clin Orthop. 1983; 177: 140-147. 20. Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop. 1989;239:196-206. 21. Kettelkamp DB, Alexander HH. Spontaneous rupture of the posterior tibial tendon. J Bone Joint Surg. 1969;SlA: 759-764. 22. Kitaoka HB, Patzer GL. Subtalar arthrodesis for posterior tibial tendon dysfunction and pes planus. Clin Orthop. 1997;345:187-194. 23. Mann RA. Acquired flatfoot in adults. Clin Orthop. 1983; 181:46-51. 24. Mann RA. Rupture of the tibialis posterior tendon. Instructional Course Lectures. 1984;33:302-309. 25. Mann RA. Flatfoot in adults. In: Mann RA, Coughlin MJ, eds. Surgery of the Foot and Ankle. Vol 1. 6th ed. St Louis, Mo: The CV Mosby Co; 1993:757-784. 26. Mann RA, Beaman DN, Horton GA. Isolated subtalar arthrodesis. Foot Ankle Int. l998;l9:5ll-5l9. 27. Mann RA, Thompson FM. Rupture of the posterior tibial tendon causing flat foot. Surgical treatment. J Bone Joint Surg. 1985;67A:556-56. 28. Michelson J, Easley M, Wigley FM, Hellman D. Posterior tibial tendon dysfunction in rheumatoid arthritis. FootAnkle Int. 1995;16:156-161. J Orthop Sports Phys Ther.\'olr~me 30. Nr~nlber2 February 2000 29. Miller SD, Van Holsbeeck M, Boruta PM, Wu KK, Katcherian DA. Ultrasound in the diagnosis of posterior tibial tendon pathology. Foot Ankle Int. 1996;17:555-558. 30. Mink JH. Tendons. In: Deutsch AL, Mink JH, Kerr R, eds. MRI of the Foot and Ankle. New York: Raven Press; 1992: 135-1 72. 31. Monto RR, Moorman CT Ill, Mallon WJ, Nunley JA Ill. Rupture of the posterior tibial tendon associated with closed ankle fracture. Foot Ankle. 1991;11:400-403. 32. Myerson M, Solomon G, Shereff M. Posterior tibial tendon dysfunction: its association with seronegative inflammatory disease. Foot Ankle. 1989;9:219-225. 33. Myerson MS. Posterior tibial tendon insufficiency. In: Myerson MS, ed. Current Therapy in Foot and Ankle Surgery. St Louis, Mo: The CV Mosby Co; l993:123-135. 34. Myenon MS. Adult acquired flatfoot deformity. J Bone Joint Surg. 1996;78A:780-792. 35. Myenon MS, Corrigan J, Thompson F, Schon LC. Tendon transfer combined with calcaneal osteotomy for treatment of posterior tibial tendon insufficiency: a radiological investigation. Foot Ankle Int. 1995;16:712-718. 36. Nazarian LN, Rawool NM, Martin CE, Schweitzer ME. Synovial fluid in the hindfoot and ankle: detection of amount and distribution with US. Radiology. 1995;197: 275-278. 37. Noto AM, Cheung Y, Rosenberg ZS, Norman A, Leeds NE. MR imaging of the ankle: normal variants. Radiology. 1989;170:121-124. 38. O'Malley MJ, Deland JT, Lee KT. Selective hindfoot arthrodesis for the treatment of adult acquired flatfoot deformity: an in vitro study. Foot Ankle Int. 1995;16:41141 7. 39. Pedowitz WJ, Kovatis P. Flatfoot in the adult. 1 Am Acad Orthop Surg. 1995;3:293-302. 40. Phillips GE. A review of elongation of the os calcis for flat feet. J Bone Joint Surg Br. 1983;65B:15-18. 41. Pomeroy GP, Manoli A 11. A new operative approach for flatfoot secondary to tibialis posterior tendon insufficiency: a preliminary report. Foot Ankle Int. 1997;18:206212. 42. Rosenberg ZS, Cheung Y, Jahss MH, Noto AM, Norman A, Leeds NE. Rupture of the posterior tibial tendon: CT and MR imaging with surgical correlation. Radiology. 1988;169:229-235. 43. Sangeorzan BJ, Mosca V, Hansen ST Jr. Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14:136-141. 44. Shereff MJ. Treatment of ruptured posterior tibial tendon with direct repair and FDL tenodesis. Foot Ankle Clin. 1997;2:281-296. 45. Teasdall RD, Johnson KA. Surgical treatment of stage I posterior tibial tendon dysfunction. Foot Ankle Int. 1994; 15:646-648. 46. Williams R. Chronic non-specific tenovaginitis of tibialis posterior. J Bone Joint Surg Br. 1963;45B:542-545. 47. Woods L, Leach RE. Posterior tibial tendon rupture in athletic people. Am J Sports Med. 1991;19:495-498.