AE 101 for VOICE Study
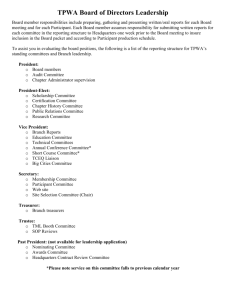
advertisement

MTN-003 Study-Specific Training Participant Safety Monitoring and Reporting Overview of Presentation Participant safety monitoring Adverse event definition Reportable adverse event definition AE terminology AE severity AE relationship to study product AE outcome AE recurrence Serious adverse event definition Expedited adverse event definition and reporting Completion of adverse event case report forms Examples Participant Safety Monitoring Participant safety is of utmost importance Several layers of safety monitoring are in place for MTN-003 Study participants Study site staff team Clinical affairs staff at SCHARP MTN-003 Protocol Safety Review Team (PSRT) NIAID Vaccine and Prevention Data and Safety Monitoring Board (DSMB) Participant Safety Monitoring Study Site Staff Team Primary responsibility for monitoring and safeguarding participants IoR Clinical staff Non-clinical staff Primary responsibility for submitting safety data to SCHARP and DAIDS Safety Office Provides data for other layers of safety review Alert Protocol Team if unexpected concerns arise Participant Safety Monitoring Clinical Affairs Staff at SCHARP Review clinical and laboratory data received at SCHARP Issue clinical data QC notes (queries) for data requiring confirmation, clarification, or further followup by site staff Help prepare safety data reports for review by the PSRT Participant Safety Monitoring MTN-003 PSRT Routinely reviews MTN-003 safety data reports prepared by SCHARP Reviews data that are pooled across study treatment groups Meets via conference call to discuss safety data and any potential safety concerns Must be consulted on some clinical and product use management issues, per protocol Always available to consult on adverse event management, product use management, and other aspects of clinical management PSRT Query Process Site submits query Email to mtn003safetymd@mtnstopshiv.org Response back to site PSPs draft response 72 hours PSPs finalize response PSRT comments PSRT Query Form Instructions: Email completed form to MTN Safety Physicians: mtn003safetymd@mtnstopshiv.org IMPORTANT: Complete all required fields so the PSRT has all information needed to respond to your query. Site: Completed by: Query Date (dd-MMM-yy): Email address: PTID: Participant Age (in years): Participant randomization assignment: Reason for query: vaginal gel or oral tablets Product use consultation: Should use of study product be temporarily discontinued? Should use of study product be permanently discontinued? Should use of study product be resumed? Request for consultation on AE management Request to withdraw participant from the study Other, specify: Is this query a request for the PSRT to consult on an adverse event (AE)? form posted on MTN-003 web page Yes → continue completing this page Emergency Safety Phone +001-412-641-8947 (toll call) Staffed by Protocol Safety Physicians 24/7 Intended for emergency safety situations only Questions that can wait should be addressed through PSRT query process Usual response time 72 hours Urgent queries can be addressed within 1 working day if necessary Contact form will be used to document each call (initiated at site, completed by Safety Physician) Participant Safety Monitoring NIAID Vaccine and Prevention DSMB Composed of independent medical, statistical, and ethical experts Routinely reviews MTN-003 safety data reports prepared by SCHARP (approx every 8 months) Data are presented by study treatment group (unblinded) Participant Safety Monitoring NIAID Vaccine and Prevention DSMB DSMB can recommend changes to study design and operations related to: Study viability Product safety and/or effectiveness Results from other studies Brief report from each review will be distributed to Protocol Team and all study sites Must be submitted to IRBs/ECs MTN-003 Study-Specific Training Questions so far? Definition: Adverse Event Any untoward medical occurrence in a clinical research participant administered an investigational product that does not necessarily have a causal relationship with the investigational product. An AE can therefore be an unfavorable or unintended sign (including an abnormal laboratory finding), symptom, or disease temporally associated with the use of an investigational product, whether or not considered related to the investigational product. ICH E6, Glossary 1.2 Definition: Adverse Event For MTN-003, the ICH definition of adverse event will be applied To all participants in all study groups Beginning at the time of randomization Definition: Pre-Existing Condition Any medical condition, problem, sign, symptom, or finding identified as ongoing in a study participant at the time of enrollment (prior to randomization). Pre-existing conditions are not AEs. However, if a pre-existing condition worsens in severity and/or frequency after randomization, the worsened condition is an AE. Let’s Discuss Adverse Events Suppose a participant reports in her baseline medical history that she has asthma. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant reports at her Month 1 visit that she had abdominal menstrual cramping two weeks before the visit. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine What more might you need to know to determine whether this is an adverse event? Let’s Discuss Adverse Events Suppose a participant becomes pregnant while in the study. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose manipulation of the speculum during a pelvic exam causes abrasion of the vaginal tissue. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant has a calculated creatinine clearance rate of 90 mL/min at Screening Part 1. At one of her study follow-up visits, this participant’s calculated creatinine clearance rate is 81 mL/min. The rate of 81 mL/min represents a 10% decrease from baseline. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant reports at her Month 11 visit that she has been feeling very sad lately. Two of her family members passed away in the past month and she and her partner are disagreeing about many household matters. She has been so sad that she has not been able to complete her household duties for the past 4 days; all she wants to do is sleep. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine MTN-003 Study-Specific Training Questions? Definition: Reportable Adverse Event An AE that meets criteria in the study protocol for reporting on adverse event case report forms (for VOICE, on the AE Log form) Reportable Adverse Events There are eight types of AEs that are reportable in VOICE. Can you name them? Reportable AEs All genital, genitourinary, and reproductive system AEs except asymptomatic bacterial vaginosis All fractures All grade 2 or higher dizziness, headache, nausea, vomiting, diarrhea, abdominal pain, rash All grade 3 or higher AEs All serious AEs, as defined by ICH GCP All AEs that result in permanent discontinuation of study product use All lab test abnormalities not otherwise associated with a reported clinical AE AEs that do not meet the above criteria but meet expedited reporting requirements How does the listing of reportable AEs change under Letter of Amendment #01? All genital, genitourinary, and reproductive system AEs except fetal losses Fetal losses (e.g., spontaneous abortions, spontaneous fetal deaths, still births) will not be reported as AEs However, untoward maternal conditions that either result in or result from fetal losses will be reported as reproductive system AEs. Is this AE Reportable? Grade 1 elevated ALT 1. 2. Yes No Is this AE Reportable? Grade 1 vulvovaginal itching 1. 2. Yes No Is this AE Reportable? Grade 1 headache 1. 2. Yes No Is this AE Reportable? Grade 2 musculoskeletal pain 1. 2. Yes No Is this AE Reportable? Grade 2 active hepatitis B infection 1. 2. Yes No Is this AE Reportable? Grade 2 malaria 1. 2. Yes No MTN-003 Study-Specific Training Questions? Adverse Event Terminology A term or description must be assigned to each AE Whenever possible, assign a diagnosis When not possible to assign a single diagnosis to describe a cluster of signs and/or symptoms, each sign and symptom must be documented as an individual AE For genital and reproductive system AEs, assign terms from the DAIDS Female Genital Grading Table If an AE can occur in more than one anatomical location, specify the location See SSP Section 11.2 for tips and guidance Let’s Discuss Adverse Events Suppose a participant reports at her Month 1 visit that she had fever, nasal congestion, cough, sore throat, and sneezing two weeks before the visit. Is this an adverse event and if so, how many? 1. 2. 3. 4. Yes, 5 AEs Yes, 1 AE No AE has occurred Not enough information to determine What term would you use to describe this AE? Let’s Discuss Adverse Events Suppose a participant reports at her Month 1 visit that she had fever, nasal congestion, cough, sore throat, and sneezing two weeks before the visit. On one of the days when she had these symptoms, she also had genital itching. Is this an adverse event and if so, how many? 1. 2. 3. 4. 5. 6. Yes, 6 AEs Yes, 5 AEs Yes, 2 AEs Yes, 1 AE No AE has occurred Not enough information to determine What terms would you use to describe these AEs? AE Terminology for Abdominal Pain Abdominal pain that is gastrointestinal in nature must be differentiated from abdominal pain that is genitourinary or reproductive in nature If gastrointestinal, report as “abdominal pain” or “lower abdominal pain” If genitourinary or reproductive, ideally localize the pain to a genitourinary or reproductive organ and report as such, e.g., adnexal pain, bladder pain If unable to localize to a specific organ, report with terms that identify a genitourinary or reproductive anatomical location, e.g., pelvic pain, urinary tract pain For pain associated with menstruation, report as dysmenorrhea MTN-003 Study-Specific Training Questions? Adverse Experience Log Form • First form in training packet • Form is “standard” (used in MTN, HPTN, IMPAACT) • Instructions on back • Additional instructions in SSP Section 14.6 • Let’s take a closer look at the form items … AE Log Form: Page Number AE Log Form: Page Number For each participant, assign page numbers starting with “001” for the first AE reported Continue assigning page numbers in sequential ascending order (002, 003, 004, etc) through the participant’s Termination Visit Do not start page numbers over at each visit Once an AE Log page has been faxed, do not change the page number or assign that page number to another AE Log form for that participant AE Log Form: Date Reported to Site AE Log Form: Date Reported to Site Date reported to site = date clinic staff became aware of the AE This could be Date of a clinic visit Date of a phone call in which a new symptom or condition is reported Date clinic staff receive an abnormal lab test result Cannot be before the AE onset date (item 2) Complete date (day, month, and year) is required AE Log Form: Item 1 AE Log Form: Item 1 Report only one AE diagnosis or symptom per page Record a unifying diagnosis whenever possible Record signs and symptoms associated with a diagnosis in comments at bottom of page E.g., “influenza” in item 1 and “with fever, chills, and myalgia” in comments When a unifying diagnosis is not available, record each reportable sign and symptom as a separate AE on a separate AE Log form page AE Log Form: Item 1 Include anatomical location when applicable Pain – location needed Headache – location not needed Record as much detail as possible in the space provided in item 1 E.g., “red, itchy rash on both arms” rather than “arm rash” The AE is coded using text in item 1 only If more details are available, record in comments AE Log Form: Item 1 Pelvic Exam Finding AEs Report any and all new abnormal findings as AEs Specify anatomical location (e.g., vulvar, vaginal, cervical) Use finding term as it appears in FGGT or Follow-up Pelvic Exam CRF, whichever is more specific For example, do not report “genital sore”. Instead, report “vaginal ulcer”. AE Log Form: Item 1 Genital Bleeding AEs Report only unexpected bleeding as AEs If bleeding associated with pelvic exam finding, report finding as the AE If bleeding unexpected and not associated with pelvic finding, use appropriate term in SSP Section 10.6 Menorrhaghia (menstrual) Menometrorrhagia (menstrual) Postcoital bleeding (non-menstrual) Metrorrhagia (non-menstrual) Separate terms for pregnancy-related bleeding AE Log Form: Item 1 Urinary Tract Infections (UTIs) Only use term “Urinary Tract Infection” if participant is symptomatic tests positive for urine LE tests positive for urine nitrites If UTI suspected, but above criteria not met Report each symptom as separate AE on separate AE Log form Do not report positive urine LE and positive nitrite results as AEs AE Log Form: Item 1 Do not report procedures or surgeries as AEs These are treatments, not AEs Treatments are collected in item 7 E.g., c-section - do not record as AE Do report the reason for a procedure and/or untoward conditions resulting from a procedure as an AE E.g., cervical dystocia – report AE as “cephalo-pelvic disproportion” (see SSP Figure 11-8) E.g., decreased hemoglobin post c-section – report as AE Include related diagnosis when available E.g., “edema related to congestive heart failure” AE Log Form: Item 1 Do not use abbreviations Is “BOM” burning on micturition or bilateral otitis media? Is “LAP” lower abdominal pain or laparotomy? Review for correct spelling Variations in spelling can lead to differences in AE coding, which means similar AEs will appear in different places in AE safety reports To QC or Not to QC? Text recorded in item 1 on AE Log form is … candidiasis appendectomy lower abdominal pain UTI tingling in genital area feeling sad assault abnormal white cell count AE Onset and Outcome Dates AE Log Form: Items 2 and 6a Onset and outcome dates can be based on Participant self-report Physical and/or pelvic exam dates For laboratory AEs, onset date = specimen collection date Record a complete date whenever available, at minimum, month and year required MTN-003 Study-Specific Training Questions? Adverse Event Severity The severity of all AEs must be graded as Grade 1 = Mild Grade 2 = Moderate Grade 3 = Severe Grade 4 = Potentially Life-Threatening Grade 5 = Death Assign grades based on the DAIDS Female Genital Grading Table (FGGT) and DAIDS Table for Grading Adult and Pediatric Adverse Events (Toxicity Table) See SSP Section 11.3 for tips and guidance How does severity grading change under Letter of Amendment #01? Bleeding during pregnancy prior to the onset of labor (regardless of trimester) will be graded per the table below: Severity Grading of Vaginal Candidiasis Normal = absence of symptoms regardless of candida test results Grade 1 = positive wet mount or other laboratory test for yeast, with mild symptoms Grade 2 = positive wet mount or other laboratory test for yeast, with moderate to severe symptoms Grade 3: Not applicable Grade 4: Not applicable AE Log Form: Item 3 MTN-003 Study-Specific Training Questions? Adverse Event Relationship The relationship of all reportable AEs to study product must be assessed as: Definitely related Probably related Possibly related Probably not related Not related Likelihood AE is Related to Study Product 0% 1-49% 50% 51-99% 100% Not Related Probably Not Related Possibly Related Probably Related Definitely Related AE clearly explained by another cause not related to study product Potential relationship cannot be ruled out but AE most likely explained by causes other than study product AE can be explained equally well by causes other than study product AE more likely explained by study product than other causes Direct association can be demonstrated between the AE and study product Factors to Consider Pre-clinical and clinical profile of the study products: protocol, package inserts, investigators brochures, other published information Timing of product use relative to onset, resolution, and/or recurrence of the AE Likelihood of observing the AE in the study population in the absence of product use Presence of other conditions or exposures that could have caused the AE Clinical judgment, including judgment of biologic plausibility Sample Case A 24 year old VOICE participant who had no pre-existing conditions and was randomized to vaginal gel presents for an interim visit, 12 days after her enrollment visit. This participant first started taking oral contraceptive pills (OCPs) at her Screening Part 2 visit, which was five days before her enrollment visit. At her interim visit, she reports that she has been taking her OCPs and inserting her study gel every day. She also reports that she has been experiencing waves of mild nausea off and on since her enrollment visit and that is why she has come to the clinic today. A pregnancy test done at the interim visit is negative. Factors to Consider Pre-clinical and clinical profile of the study products: protocol, package inserts, investigators brochures, other published information What do we know about nausea from the available sources? Factors to Consider Timing of product use relative to onset, resolution, and/or recurrence of the AE What do we know about use of study gel in relation to the participant’s nausea? What can we do to find out more? Factors to Consider Likelihood of observing the AE in the study population in the absence of product use How common is nausea in the population from which the study participants are drawn? If the participant was a patient of yours, outside of the study, how likely is it that she might experience nausea? Factors to Consider Presence of other conditions or exposures that could have caused the AE What do we know about the presence or absence of other possible causes of the participant’s nausea? Consider other medications, concomitant illnesses, infectious diseases, etc … What can we do to find out more? Factors to Consider Clinical judgment What if… Instead the participant was randomized to oral tablets and reports that she has been taking her OCPs and her study tablets every day. The participant was randomized to oral tablets, but the participant first started taking oral contraceptive pills (OCPs) about 9 months before joining the study and she cannot remember experiencing nausea like this since she was a child. MTN-003 Study-Specific Training Questions? Relationship to Study Product AE Log Form: Item 4 If “not related” is marked, the cause of the AE and/or other reason why the AE is not related must be recorded in comments For MTN-003, vaginal product = gel + applicator If an AE is thought to be related to the applicator, report this by assigning one of the “related” categories and record in comments that the presumed relationship is to the applicator Study Product Administration AE Log Form: Item 5 Mark “No change” if the AE does not result in product hold/discontinuation (participant is on product and may continue using it) Mark “N/A” if product was already held or permanently discontinued when the AE occurred If multiple AEs are reported at a visit when product is held, mark “Held” only for those AEs that required product to be held All other AEs reported at the same visit should be marked “N/A” If multiple AEs are reported at a visit when product is permanently discontinued, mark “Permanently Discontinued” only for those AEs that required permanent discontinuation All other AEs reported at the same visit should be marked “N/A” MTN-003 Study-Specific Training Questions? Adverse Event Outcome All AEs – reportable and not reportable – must be followed clinically until the AE resolves or stabilizes Resolution = return to baseline severity grade Stabilization = persistence at a severity grade above baseline for 3 consecutive monthly evaluations Adverse Event Outcome At each visit, an authorized study clinician should review all previously reported ongoing AEs to evaluate their current status Oftentimes the outcome of an AE will not be available when the AE is first documented In such cases, documentation should be updated when the final outcome becomes available Adverse Event Outcome If an AE increases in severity or frequency, the higher grade AE must be documented (and reported) as a new AE If an AE completely resolves and then recurs at a later date, the second occurrence must be documented (and reported) as a new AE Let’s Discuss Adverse Events Suppose a participant has completely normal laboratory test results at Screening Part 1. At Month 1, her hemoglobin level is grade 1. At Month 2 her hemoglobin level is grade 2, and she is asked to return in three days for another test. At that time her hemoglobin level has returned to grade 1. At Month 3, her hemoglobin level is normal. How many AEs have occurred? 1. 2. 3. 4. 1 AE 2 AEs 3 AEs 4 AEs Let’s Discuss Adverse Events Suppose a participant has completely normal laboratory test results at Screening Part 1. At Month 1, her hemoglobin level is grade 1. At Month 2 her hemoglobin level is grade 2, and she is asked to return in three days for another test. At that time her hemoglobin level has returned to grade 1. At Month 3, her hemoglobin level is normal. Suppose this participant’s hemoglobin level is found to be grade 2 at Month 6. Has another adverse event occurred? 1. 2. 3. Yes No Not enough information MTN-003 Study-Specific Training Questions? Status/Outcome and Date AE Log Page: Items 6 and 6a If AE outcome/status is “Continuing” when the AE is first reported, leave item 6a blank Later, after an AE outcome is determined Line through the “Continuing” box Mark the appropriate box for item 6 Record the appropriate outcome date in item 6a Initial, date, and refax When status/outcome = resolved, death or severity/frequency increased, an outcome date must be recorded in item 6a AE Log Page: Items 6 and 6a If a previously-reported AE increases in severity grade: Close out the previously-reported (lower grade) AE by updating item 6 to “severity/frequency increased” and recording in item 6a the date the AE increased in severity. Initial, date, and refax. Complete a new AE Log page for the new (higher grade) AE. Use the same text in item 1 as for the lower grade AE. Record in item 2 (onset date) the date the AE increased in severity. Initial, date, fax. The date the AE increased in severity will be recorded as the outcome date of the lower grade AE and the onset date of the new AE Example of Severity Increase On 03-NOV-09, a participant has a grade 1 decreased hemoglobin value. An AE Log form is completed with status = continuing. At the next visit on 01-DEC-09, the hemoglobin value is still grade 1. Any updates to the AE Log form? At the next visit on 05-JAN-10, the hemoglobin value is grade 2. What do you do? Update AE Log form for grade 1 decreased hemoglobin: outcome = severity/frequency increased, outcome date = 05JAN10. Initial, date, refax. Complete new AE Log form, item 1 = decreased hemoglobin, onset date = 05-JAN-10, severity = grade 2, status = continuing. Initial, date, fax. AE Log Page: Items 6 and 6a Improvements in AE severity – prior to resolution – do not require changes to AE Log forms E.g., Grade 2 rash identified at Month 6 At an interim visit one week after the Month 6 visit, the rash is re-assessed and found to have improved to grade 1 Any updates to the AE form completed at Month 6? Any new AE Log forms completed? At Month 7, the rash has resolved Any updates to the AE form completed at Month 6? Any new AE Log forms completed? AE Log Page: Items 6 and 6a At each participant’s Termination Visit, review all AEs marked as “continuing” For any AEs continuing (ongoing) at the Termination Visit, update item 6 to “continuing at end of study participation” and initial, date, and refax Treatment AE Log Form: Item 7 Record treatments that are clinically-indicated for the AE, *regardless* of actual use E.g., participant has an STI requiring treatment, but she refuses the medication. Mark item 7 as “Medications” In comments, record that the participant refused the indicated treatment. Do not record the medication on the Concomitant Medications Log (only document medications actually taken/used by participant on the Con Meds Log) Mark “Medications” if participant self-treated with medications obtained on her own MTN-003 Study-Specific Training Questions? Definition: Serious Adverse Event Any untoward medical occurrence that at any dose: Results in death Is life-threatening Requires inpatient hospitalization or prolongation of existing hospitalization Results in persistent or significant disability/ incapacity Is a congenital anomaly/birth defect Important medical events that may not be immediately life-threatening or result in death or hospitalization, but may jeopardize the participant or may require intervention to prevent one of the above-listed outcomes, also may be considered serious. Seriousness of Adverse Events Seriousness ≠ severity SAEs are a subset of all AEs All SAEs are reportable on AE Log forms All AEs must be assessed by authorized study staff to determine whether they meet the definition of serious source document and record on AE Log form AE Log Form: Item 8 Definition: Expedited Adverse Event AE that meets criteria in the study protocol for additional reporting for rapid review and assessment by DAIDS VOICE protocol specifies “standard” reporting per the Manual for Expedited Reporting of Adverse Events to DAIDS Expedited Adverse Events EAE ≠ SAE SAEs and EAEs are two different subsets of AEs Some EAEs will be serious, some will not All EAEs are reportable on AE Log forms All AEs must be assessed by authorized study staff to determine whether they meet criteria for expedited reporting source document and record on AE Log form AE Log Form: Item 9 EAE Reporting Type of Adverse Event Standard EAE Reporting Results in death Is a congenital anomaly or birth defect or fetal loss Report as EAE regardless of relationship Results in persistent or significant disabilities or incapacities Requires or prolongs hospitalization or requires intervention to prevent significant/permanent disability or death Is life-threatening (includes all grade 4 AEs) Other grade 1, grade 2, and grade 3 AEs Report as EAE if: Definitely related Probably related Possibly related Probably not related Do not report as EAE More EAE Reporting AEs that may be related to study product (definitely, probably, possibly, or probably not related) that the IoR believes are of sufficient concern to be reported on an expedited basis to DAIDS; includes AEs that, based upon appropriate medical judgment, may jeopardize the participant and may require medical or surgical intervention to prevent an SAE SAEs that are not related to study product but could be associated with study participation or procedures Unexpected SAEs that may be related to study product (definitely, probably, possibly, or probably not related) and occur after the protocol-defined expedited reporting period How does EAE reporting change under Letter of Amendment #01? Type of Adverse Event Standard EAE Reporting Results in death Is a congenital anomaly or birth defect or fetal loss Report as EAE regardless of relationship Results in persistent or significant disabilities or incapacities Requires or prolongs hospitalization or Report as EAE if: requires intervention to prevent Definitely related significant/permanent disability or Probably related death Possibly related Is life-threatening Probably not related (includes all grade 4 AEs) Other grade 1, grade 2, and grade 3 AEs Do not report as EAE EAE Reporting Report within 3 business days of site awareness Check for consistency with AE Log case report form Submit incomplete report if needed to meet timeframe Follow up as quickly as possible Use DAIDS Adverse Experience Reporting System (DAERS) and DAERS Reference Guide for Site Reporters and Study Physicians Or submit paper EAE form if internet not available Print and file all submitted EAE reports/forms, all confirmations of receipt, any correspondence Respond in a timely manner to any requests for more information MTN-003 Study-Specific Training Questions? Let’s Discuss Adverse Events Suppose a participant is killed in a car accident after completing her Month 7 study visit but before her Month 8 visit. It takes some effort to find out exactly what happened, but you are able to obtain a verbal report from the participant’s mother three weeks after the Month 7 visit and you obtain hospital records related to her injuries one week after that. Is this AE serious? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant reports at her Month 7 visit that she has fever, nasal congestion, cough, sore throat, and sneezing. The Month 7 visit is completed per the protocol, including documentation of upper respiratory tract infection as a grade 2 AE. Several days later, a friend of the participant, who is also in the study, presents for a study visit and reports that the participant has been hospitalized. You contact the hospital, talk to the participant, and receive verbal confirmation from the hospital physician that the participant has been diagnosed with pneumonia. How many AEs have occurred? 1. 2. 3. One Two None Let’s Discuss Adverse Events Suppose a participant reports at her Month 7 visit that she has fever, nasal congestion, cough, sore throat, and sneezing. The Month 7 visit is completed per the protocol, including documentation of upper respiratory tract infection as a grade 2 AE. Several days later, a friend of the participant, who is also in the study, presents for a study visit and reports that the participant has been hospitalized. You contact the hospital, talk to the participant, and receive verbal confirmation from the hospital physician that the participant has been diagnosed with pneumonia. How many are serious? 1. 2. 3. One Two None Let’s Discuss Adverse Events Suppose a participant reports at her Month 7 visit that she has fever, nasal congestion, cough, sore throat, and sneezing. The Month 7 visit is completed per the protocol, including documentation of upper respiratory tract infection as a grade 2 AE. Several days later, a friend of the participant, who is also in the study, presents for a study visit and reports that the participant has been hospitalized. You contact the hospital, talk to the participant, and receive verbal confirmation from the hospital physician that the participant has been diagnosed with pneumonia. How many are EAEs? 1. 2. 3. One Two Not enough information Let’s Discuss Adverse Events Suppose a participant has a grade 4 decreased absolute neutrophil count at her Month 9 visit. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant has a grade 4 decreased absolute neutrophil count at her Month 9 visit. 82% Is this AE serious? 1. 2. 3. Yes No Not enough information to determine 9% 1 2 9% 3 Let’s Discuss Adverse Events Suppose a participant has a grade 4 decreased absolute neutrophil count at her Month 9 visit. Does the AE need to be reported as an EAE? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant has a positive pregnancy test at her Month 13 visit. At her Month 14 visit, her pregnancy test is negative. She reports having no symptoms between visits and is surprised that she is no longer pregnant. Is this an adverse event? 1. 2. 3. Yes No Not enough information to determine Let’s Discuss Adverse Events Suppose a participant has an argument with her partner related to her participation in the study. She was late meeting him because a study visit took longer than expected. He thinks the study is taking up too much of her time and he does not want to hear any more from her about safe sex and using condoms. The argument escalates and he pushes her to the floor, resulting in a laceration on her forehead and a broken collarbone. She is treated in the emergency department and then admitted to the hospital for observation related to her head injury. How many AEs have occurred? 1. 2. 3. One Two None Let’s Discuss Adverse Events Suppose a participant has an argument with her partner related to her participation in the study. She was late meeting him because a study visit took longer than expected. He thinks the study is taking up too much of her time and he does not want to hear any more from her about safe sex and using condoms. The argument escalates and he pushes her to the floor, resulting in a laceration on her forehead and a broken collarbone. She is treated in the emergency department and then admitted to the hospital for observation related to her head injury. How many AEs are EAEs? 1. 2. 3. One Two None MTN-003 Study-Specific Training Questions? AE Log Form: Item 10 The visit code in item 10 should match the “Date Reported to Site” recorded in the upper right corner of the AE Log form AE Log Form: Item 11 Review the participant’s Pre-existing Conditions form (and other documentation as needed) to determine if the AE is a worsening of a preexisting condition Adverse Event Documentation Regardless of reporting on AE Log forms, study staff must identify and document all AEs For each AE, source documentation should include AE term/diagnosis, severity grade, onset date, outcome, outcome date, treatment For reportable AEs, source documentation also must include date reported to site, relationship to study product, action taken with study product, whether the AE is serious, whether the AE meets criteria for expedited reporting (EAE) Adverse Event Documentation Site SOPs for source documentation should reflect limited AE reporting: Because some AEs will not be reported on an AE Log form, this form cannot be designated as source for all data elements Identify in SOPs what documents will be source Use AE tracking tools to ensure all AEs are properly documented and all reportable AEs are reported on the AE Log case report form Adverse Event Reporting Site delegation of duties documentation should specify which study staff are authorized to complete AE source documentation, AE Log forms, and EAE report forms All forms should be reviewed for completeness, accuracy, and consistency of reporting by a clinician listed on the FDA Form 1572 discuss review finding as a team for ongoing training and QA Re: consistency, ensure text in item 1 is not contradicted by text in comments MTN-003 Study-Specific Training Questions? For AEs Reported as EAEs Review AE Log forms and EAE reports for consistency: Protocol and PTID AE term Onset date Severity Relationship to study product Discrepancies will result in a clinical query If a previously-reported EAE is updated, update the matching AE Log form when applicable Fax the AE Log form to SCHARP at the same time as submitting the EAE report to the DAIDS Safety Office Storage of AE Log Forms Recommendation = store all AE Log forms for a participant within one section of her study notebook Consider methods to identify AE Log pages that have “continuing” AEs to help ensure these are reviewed and updated as needed at each visit until an AE has an outcome or the participant terminates from the study SCHARP will provide an “Unresolved AE” listing that lists AEs that have been continuing for several months How to Mark AE Log Forms as Deleted If you need to delete an AE (if, for example, an AE was reported in error), draw a diagonal line across the AE Log form page, write “delete due to _____” and initial, date, and refax Keep the AE Log form page in the participant’s study notebook Do not re-number the remaining AE Log pages for the participant and do not “reassign” the page number of the deleted AE The deleted AE remains in DataFax but will not be included in any reports or data analyses References Protocol Section 8 and SSP Section 11 DAIDS Toxicity Table and FGGT Package Insert Viread Package Insert for Truvada Investigators Brochure for Tenofovir Gel Manual for Expedited Reporting of Adverse Events to DAIDS DAERS Reference Guide for Site Reporters and Study Physicians MTN-003 Study-Specific Training Questions? AE Log Form Data QC Examples Do not use abbreviations Report genital bleeding using appropriate term per SSP section 10.6.4 Use term “urinary tract infection” only if symptoms present AND urine dipstick is positive for BOTH LE and nitrites. Otherwise, report each symptom as a separate AE. Refer to SSP section 11.3, Data CQE #1 reminder #2, and Data CQE #3 clarification #10. Report each genital symptom on a separate AE Log form. Specify anatomical location (e.g., vulvar, vaginal, cervical) Line through “Continuing” box, mark “Resolved” and initial/date. Specify anatomical location and type of finding. Use appropriate term in FGGT or on Pelvic Exam CRF, whichever is more specific. Wetness due to study gel is not an AE. It could cause a genital AE though, such as erythema, which would be a reportable AE. Treatment was given (dietary advice) and documented correctly as “Other” in item 7, with description in Comments. AE term should be “hypophosphatemia” since treatment was given. See Data CQE #1 reminder #3. Delete “Vaginal Discharge” text and document discharge in Comments, if part of the “symptomatic bacterial vaginosis” diagnosis, or as its own separate AE. Do not use abbreviations. Per protocol section 8.2, Grade 1 nausea is not a reportable AE. This AE Log form should be marked for deletion. Only Unexpected Genital Bleeding is an AE. If the bleeding is expected, this AE Log form should be marked for deletion. Use more specific term(s) to describe what is meant by “difficulty”. This will help with MedDRA coding. Do not use symbols or abbreviations. Specify anatomical location. Per protocol Clarification Memo #02, cervical bleeding associated with speculum insertion and/or cervical specimen collection judged to be within the range of normal is considered expected nonmenstrual bleeding (and is not an AE). Item 10 Visit Code is not valid. Item 4 is marked “Not related”, but no alternate etiology is provided in the Comments section.