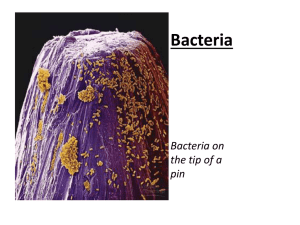
File - Dr.Taghreed Khudhur
advertisement

Dr.Taghreed Khudhur Mohammad Ahmed Dawood Lab. 1 2015 Sterilization التعقيم Sterilization: is a freeing of an article from all living microorganisms including bacteria and their spores, viruses, yeasts, molds (pathogenic and nonpathogenic) .هو خلو االدوات من االحياء المجهرية المتضمنة البكتريا )وسبوراتها والفايروسات والخمائر واالعفان ( الممرضة والغير ممرضة Methods of Sterilization :- طرق التعقيم Physical methods . الفيزياوية Chemical methods . الكيمياوية Mechanical methods الميكانيكية 1 sterilization mechanical physical chemical other filtration pH,osmotic pressure , highly movement speed , sonication ionizing gases formaldehyde antiseptic radiation disinfectant Non ionizing heat Moist heat Dry heat Red heat Temp. above 100 C Flaming` Temp. at 100 C autoclaving incineration Temp below 100 C Hot air oven tyndalization boiling pasteurization 2 Physical methods of sterilization :A -Heat sterilization التعقيم بالحرارة 1) Dry heat sterilization الحرارة اجافة a. Red heat used to sterilize wire loops ,point end of forceps الحرارة الحمراء تستخدم لتعقيم الناقل ونهايات المالقط b. Flaming: used to sterilize mouth of tubes , glass spreaders (which are flamed in ethanol ). األلهاب تستخدم لتعقيم فوهات االنابيب c. Incineration الحرق:used in pathological fuming materials . 3 d. Hot air oven ( 160-180 ) ˚C for 2-4 hr., used to sterilize glass wares ( pipette ماصات زجاجية, syringes سرنجات زجاجية, flask دوارق زجاجية, glass Petri dishes اطباق بتري زجاجية, ….etc ) . فرن الحرارة الساخن ,Conical flask , volumetric flask , Beaker, Graduated cylinder , Petri dish 4 2) Moist heat sterilization الرطبة a. Temperature below 100˚C, pasteurization (63˚C for 30 min ) , to sterilize milk . م لتعقيم الحليب100 حرارة أقل من b. Temperature at 100 ˚C Boiling (5-10 min ) to sterilize rubber tubes , glass syringes ( kills all non-spore forming bacteria ) . Steaming ( tyndillization ) steam 30 min for 3 days ,used to sterilize gelatin media , sugar media . بخار بدرجة م لتعقيم االوساط الجيالتينة واالوساط السكرية100 C .Temperature above 100 ˚C ( autoclave ) the condition used in this instrument (121˚C ,15 min, 15 p/inch2 ),used for sterilization of : surgical tools and clothes االدوات الجراحية ومالبس العلميات culture media and to sterilize inoculated media االوساط الزرعية Swab المسحة D.W. ماء مقطر, Solutions sealed in containers ampuls, vials , Bulk Solutions محاليل بحجوم كبيرة Glassware Instruments Intraoperative sterilization of metallic devices اجهزة معدنية metallic surgical instruments 5 B -Radiation sterilization Non ionizing type, like ultra-violate rays , infra-red rays Ionizing type, like Gamma rays , X ray , Beta rays Ultraviolet Lampe (UV rays) (300 – 400 nanometers) Wavelengths 2500-2600 A° Limited uses that even thin glass or moisture protect from UV rays Used in sterile inoculations cabinets sterile operation rooms Infra-red sterilize Water bath …. 6 C- GASEOUS STERILIZATION التعقيم بالغازات Equipment: Special oven for admission of gas, humidity & hermeticمحكم السد Gases: formaldehyde ethylene oxide Carbon dioxide Ethylene Oxide Kills germs by damaging their DNA-RNA Liquid below 11 C Flammable, explosive, toxic and possibly carcinogenic Advantages: High penetration Compatible with most materials Disadvantage toxic residuals Explosive hazard Not appropriate for solutions Application: plastic syringes(disposable syringes) disposable Petri dish surgical sutures intraocular lens ligament-tendon repair devices إصالح وتر- أجهزة الرباط absorbable bone repair devices heart valves and vascular grafts Thermolabile powder plastic polymers ophthalmic preparation subcutaneous vaginal inserts tubing sets 7 Mechanical methods: Filtration: The material is effect by heat (Heat sensitive solutions ) Ex. (serum , protein , sugar, vaccine,..) are sterilized by filtration . Filters (bacterial filtration) 1. Porcelain filters 1. Siliceous earth filter 2. Sintered glass filters 3. Asbestos filters 4. Membrane filters nitrocellulose different pore sizes .45μm used 8 D-Others: pH, Pressure Osmotic pressure Highly movement speed Sonication Quiz4 Q1- Fill in the blanks with suitable answer: The disadvantages of gaseous sterilization are __________ and______________. Q2- Write the types of Wet heat with examples of each type. 9 Chemical methods of sterilization A- Antiseptic :It is chemical substance that kill micro-organisms on living tissues , ex. 70% alcohol , heptane , 10% Dettol to sterilize hand … المادة الكيمياوية المستخدمة لقتل االحياء المجهرية وتستخدم مع االنسجة مثل االنسان وااليدي B- Disinfectant :IT is a chemical substance used to sterilize non -living objects لتعقيم االشياء الغير حية, ex. Phenol , 5% formalin to sterilize refrigerator الثالجة, bench البنجات, floor االرضية The disinfectant may be described either as : Bacteriostatic:- any chemical substance which inhibits the growth and multiplication of bacteria but do not necessarily kill them . Bacteriocidal :- any chemical substance which kills the bacteria and their spores. Disinfection : freeing of an object from some or all living pathogenic microorganism by inhibit growth & multiplication of microorganism . Sepsis : presence of infection (M.O) in living tissue . Asepsis : Absence of infection (M.O) in living tissue . 10 Dr.Taghreed Khudhur Mohammad Ahmad Dawood Salman Lab.2 / 2015 Preparation of Culture media Aims: 1. To Isolate the bacteria عزل البكتريا. 2. To demonstrate the properties of bacteria دراسة صفاتها. 3. To obtain sufficient pure growth for preparation of antigen and for other test . زرع نقي 4. To determine sensitivity to antibiotic. 5. To estimate viable count . العدد الحي 6. To maintain stock culture ( store the microorganisms ffrom months to years). حفظ البكتريا Equipment: 1. Balance 2. Conical flask. 3. Graduated cylinder. 4. 5. 6. 7. 8. Spatula. Source of heat ( Bunsen burner ). Filter paper Autoclave powder of culture media 11 Procedure:1-weight media powder by using a balance. 2-Dissolve powder in D. W 3-use a heat to complete dissolving of powder. 4-put cotton plug on 1 mouth of conical flask. 5-sterilize by using Autoclave . تعقيم االوساط الزرعية باالوتوكليف 6-cool the media to (45-50)C . 7-pour this media a Petri dish about 20 ml for each. 8-let plate for some time to Solidify a media. 9-Put plates in refrigerator upside down until using. حفظ االطباق في الثالجة Basic components of culture media: 1- Energy source : (carbon , amino acid ,..) 2- Carbon source : (glucose ,..) 3- Nitrogen source 4- Minerals and salts ( NaCl) 5- pH 6- Growth factor 7- etc…. 8- Water 12 Quiz Q1-Write the advantages of autoclave? Q2- Why you prepare culture media in your laboratories? 13 Dr.Taghreed Khudhur Mohammad Ahmad Dawood Salman Lab.3 / 2015 Classification of culture media according to components (function) : 1. Simple media 2. Enrichment media 3. Differential media 4. Selective media 5. Special media Nutrient broth , Nutrient agar Blood agar , Chocolate agar MacConkey agar MacConkey agar, S.S agar, Manitol salt agar Brucella agar 14 Nutrient agar 25 g 1 L Distilled water (D.W) Blood agar : (N.agar or blood agar) + Distal water = dissolve by heating &then sterilized with autoclave &then cool to 55c0 &then add 3-4 % blood . Chocolate agar : (nutrient agar or blood agar) + Distal water = dissolve by heating &then sterilized with autoclave &then cool to 80c0 &then add 3-4 % blood (blood is hemolysis release X , V factor). 15 MacConkey Agar Is selective for Gram negative organisms, and helps to differentiate lactose fermenting gram negative rods from Non lactose fermenting gram negative rods. It is primarily used for detection and isolation of members of family enterobacteriaceae and Pseudomonas spp. Composition of MacConeky Agar: 1. Enzymatic Digest of Gelatin, Casein: provides nitrogen, vitamins, minerals and amino acids essential for growth. 2. Lactose: fermentable carbohydrate providing carbon and energy. 3. Bile Salts: selective agents and inhibit Gram positive organisms. 4. Crystal Violet: Gram positive bacteria are generally inhibited . 5. Sodium Chloride: supplies essential electrolytes for transport and osmotic balance. 6. Neutral Red: pH indicator. which is red in color at pH’s below 6.8. When lactose is fermented, the pH of the medium decreases, changing the color of neutral red to pink 7- Agar : (Solidifying agent ) polysaccharide extract from sea weedy (red algae ) , used for solidification of culture media , its solidify at 42 C0 & melted at 95 C 0 . 16g 1 L D.W 16 Classification of media according to solubility (Form) : 1 – liquid media (broth media) :contain all ingredient except agar (0%). 2 – Semi solid media: contain all ingredient except & 0.2 – 0.4% agar. (Motility test medium). +3 – Solid media: contain all ingredient except & 1.5 – 2% agar. 17 Dr.Taghreed Khudhur Mohammad Ahmad Dawood Salman Lab.4 / 2015 Inoculation on Solid media (Streaking on Solid media) : Aim: The purpose of streaking to get an isolated colony to know the type of Bacteria which is help to diagnose of organism which cause disease. Equipment : 1. 2. 3. 4. 5. Spirit lamp or Bensun Burner Bacteriological loop Solid media ( Blood agar or Nutrient agar or MacConkey agar , etc. ). Sample ( urine , stool, blood , CSF,…..etc. ) or Bacteria. Incubator . Procedure: 1-Put the solid media and clinical sample near Bunsen burner. 2-Sterilize the loop by flaming . 3- Cool it by touching the loop on side of medium. 4-Hold a piece of colony by loop ( or drop of urine or CSF or stool or blood or ear swab or wound swab ) and transfer it to a new media .As in A this area termed inoculum area. 5-Re - sterilize the loop and repeat point 3. 6-make 4 parallel line as in B . 7-Repeat point (2and3) . 8-repeat point 6 as in c 9- repeat point 2.3 . 10- repeat point 6 as in D 11- repeat point 2.3 . 12- from D , Make a zigzag line to the middle of medium to get an isolated colony . 13- Incubate the culture media in incubator at 37C° for (18-24) hr . 14- Isolated colony appears after incubation. 18 مستعمرة مفصولةIsolated colony 19 The method or types of inoculation (culturing) I-SOLID MEDIA A-Plate cultured methods Streak plate method Carpet culture method Pouer plate method B-Tube culture methods Slope (Slant) culture stock Deep culture Stab culture Roll tubes II-Liquid media On SOLID Media 1 -Plate cultured methods (Streak plate method ) : To isolate single colonies ( Obtaining Isolated Colonies ) Colonies can be Identified and Further Evaluated 2-Carpet culture (lawn culture, whole surface, spreading methods). These methods are prepared by flooding the surface of plate with suspension of bacteria it provides uniform surface growth of bacteria; it is useful for bacteria phage typing and antibiotic sensitivity test. And this method of streaking may be used either for culture from solid media or for heavy broth culture and smeared over the whole surface, using a sterile spreader or loop or swabs 20 3-Pouer plate method About 15-20 ml of agar media are melted and left to cool in water bath at 45oC-50 C°. Appropriate dilution of inoculum are added in 1 ml volume to molten agar and mixed well. Contents of tube are poured in Petri dish. They are allowed to set and after incubation colonies will be seen distributed through out of the depth medium. The colonies growing in and on the medium. This method give viable bacteria count in suspension it is recommended method for food microbiology. B- TUBE CULTURE METHOD 1- Slope (Slant) culture stock. Many tests devised to differentiate organisms require solid cultures. It is not always necessary to grow an organism on a whole Petri dish of medium, and slope cultures often suffice. ‘Slops’ or ‘slants’ are tubes or bottles containing a small quantity of medium ,that has been allowed to solidify with the bottles slightly raised at one end. Such slopes are used only for maintenance or biochemical tests once the organism has been isolated in pure culture, they cultured by streaking the surface of slope media 2- Deep culture. Anaerobic organisms require an oxygen-free atmosphere. For cultivation of these organisms ‘shake’ or ‘deep’ cultures are sometimes made. The medium is distributed in 150mm x 20mm tubes to a depth of 6-7cm and allowed to solidify. For use, the medium is melted, cooled at about 45 C o, inoculated with organism, and mixed by rotation between the palms of the hands. When it has solidified, the culture is incubated and the anaerobic organisms grow at the bottom of the tube. These shake, or deep, tubes can also be used for counts of viable organisms. 21 3- Roll tubes. The ‘roll rube’ method is also useful for counting viable organisms. The medium is distributed in to 6 x (5/8) in tubes, 1-2 ml per tube, and stored. For use, the medium is melted, cooled to approximately 50 Co, and a known dilution of the test sample is added. The tube is then titled and rolled between finger and thumb, allowing the medium to run all rounds the sides of the tube just bellow the half way mark. This rolling is carried out under cold tap water. A thin film of agar solidifies around the sides of the tube, which is inverted for incubation. 3- Stab culture. It is prepared by puncturing charged long straight wire (4.5-5 cm). Stab culture are employed mainly for demonstration of gelatin liquefication and motility test and for maintaining stock culture II-Liquid culture Media prepared in tubes or bottles or flasks and inoculated by touching with a charged loop. Liquid culture is preferred when large and quick yield is required. The major disadvantage of Liquid culture is that it does not provide pure culture from mixed inocula. . This method constitutes a simple technique and used for liquid culture largely but it may also be used for culture from solid media. Quiz / 1 . Numerate & explain briefly types of culturing. 22 Cultural characteristic Bacteria grown artificially (in vitro) on agar plates are described as colonies vary in size, shape, pigment production and hemolysis on blood agar, depending on the type of media. A. Description of colonies on solid culture 1- Shape: circular, irregular, radiating or rhizoid. 2- Surface: Bacterial colonies are frequently shiny and smooth in appearance. Other surface descriptions might be: veined, rough, dull, wrinkled (or shriveled), glistening. 3- Color – It is important to describe the color or pigment of the colony. Also include descriptive terms for any other relevant optical characteristics such as: opaque, cloudy, translucent, iridescent. 4- Size: Surface colonies are measured in millimeter, they are 2-3 mm in diameter. Smaller ones may be less than (about 0.5-1 mm). 5- Elevation: may be raised, low convex, implicated or dome shape 23 6- Edges: mostly edges are entire, sometimes crenate, fimbrated or effuse. 7- Color (pigmentation): some organism may produce pigmented colonies (Staphylococcus,Pseudomonas) Pseudomonas Staphylococcus on blood agar 8- Opacity: colonies on nutrient agar may be transparent, translucent or opaque. 24 9- Consistency: Mostly soft and butyrous and may be hard, firm, mucoid, tenacious, dry, adherent to medium, friable and membranous. Klebsiella on blood agar and MacConkey agar 10- Contiguity: may be discrete or swarming. Proteus on blood agar 11- Changes in the medium: colonial growth may bring about color changes in the media themselves produce soluble pigment that diffuse in to the medium and some organism haemolysis the blood of medium around the colony. 25 12Emulsifiability: Growth of some bacteria is easily emulsifiable (like E. coli, salmonella) where as growth of N. catarrhalis is not emulsifiable and form granules. 13- Odor Description of growth in liquid culture Growth in liquid medium is described as: 1. Turbidity: Clear or turbid 2. Deposit : Growth of Streptococcus pyogenous is characterized by deposit at the bottom of the tube 3. Surface growth: Surface growth is related to aerobic nature of organism. 4. Color changes: Some organisms produce water soluble, pigment which after diffusion change the color of medium e.g. Pseudomonas pyocyneous. Quiz / 2 How can you describe colonies . 26 Clinical samples : The samples may be:Blood Fasces (Stool) Gastric contents Hair Pus Saliva Sputum Urine C.S.F (cerebrospinal fluid) Effusions like:-Pleural fluid Peritoneal fluid Seminal fluid and others Swabs like: - Throat Swabs Pharyngeal Swabs Laryngeal Swabs Mouth Swabs Nasal Swabs Abacuses Swabs Ear Swabs Eye Swabs Wounds Swabs Rectal Swabs Genitourinary swabs: (High-vaginal Swabs, Urethral discharge Swabs) 27 Examination of specimens BACTERIOLOGICAL EXAMINATION OF SPECIMENS A general plan for examination specimens is as fellows. 1-MACROSCOPIC EXAMINATION:- Note the following: 1. Color, opacity, consistency. 2. Presence of blood, mucus or pus. 3. Presence of macroscopic bodies, such as parasites. 2-MICROSCOPIC EXAMINATION A- Unstained film or wet preparation When looking for cells or casts in urine deposit and protozoa parasites in stool or looking for motile bacteria… ect. B- Stained film by (a) simple stain (b) Gram stain (c) Acid-fast bacilli stain. (d) Special stains. (e) Negative staining 3-CULTURE: inoculated accurate media according the suggested microorganisms found in the sample, then incubated aerobically and anaerobically, mostly using Blood agar. MacConkey agar. Special media. b-Biochemical test:-oxidase, catalase, coagulase , IMVIC tests, motility,TSI... c-Serology test and serotyping. agglutination test with specific anti sera d-Phage typing. e-Genetic tests. f- Toxin production. g-Animal inoculation : is carried out only if necessary. h- SENSITIVITY TEST Antimicrobial Susceptibility Testing 28 (susceptibility test) Susceptibility Testing sensitivity of organisms to antibacterial substances, e.g. antibiotics(penicillin,streptomycin,tetracycline,chlorimphenicol,fusidin, kanamycin,gentamycin,ampicillin,neomycin,furadantin,polymaxins…ec t.) is an important factor in the treatment of patients. There are two main methods of sensitivity testing, namely: incorporation methods like discs Susceptible Not susceptible Growth No growth Antibiotic disk method and diffusion methods. Each of these may be carried out by a variety of techniques. Quiz1 Fill in the blanks with suitable answer :There are two main methods for sensitivity test __________ and______________. 29 5- THE REPORT For the final report, however, it is only necessary to report the organism or organisms seen in smear and isolated on culture together with the sensitivity pattern. 30 Microscopic examination of bacteria: The morphology of bacteria can be studied by the microscopic examination A- Unstained preparations used to studied both shape and motility of bacteria suspended in a fluid using: a -the hanging drop method b- wet smear B- Staining technique must be used to render للتعررthe structure of cells visible. These will only differentiate relatively gross individual structures C- Electron microscopy complex techniques are needed to reveal those not shown by staining. Staining will help to identify organisms and place them in their own particular group by their individual reactions to certain stains. An example is the gram stain. 31 Preparing of bacterial smears A-Making of wet preparations: Principle: drop of liquid containing microorganisms on a slide covered with a coverslip Advantages: can observe live organisms Disadvantages: dries out quickly Procedure: 1. Make a smear on a clean and dry microscope slide : a-From culture grow in liquid media by putting 1-3 drops of liquid cultures on the slide using the loop or Pasteur pipette b-From culture grow on solid media by emulsify the colony in a small drop of saline c-Emulsify the specimens such as feces in a small drop of saline, iodine, or the required stain. 2-Carefully place a cover slip on to the suspension taking care that no fluid extrudes beyond the edges of the cover slip. 32 3- Examine microscopically as for hanging drop under power 10X or 40X. Hanging drop technique drop of liquid containing microorganisms on a slide covered with a cover slip & suspended over a depression slide Advantages of the hanging drop: *Easy to prepare *Bacteria are live so we can see bacterial motility: B-Making of dry smears: 1. Use clean slides free from grease. 2. Mark the slide with a glass writing diamond - grease pencil is easily rubbed away. 3. From liquid cultures make fairly heavy smears. 4. From cultures on solid media, make thin smears. 5. Do not used water taken form rubber tubing attached to taps for making smears, as organisms may be transferred from the rubber. 6. When blotting slides, use a fresh portion of paper for each slide, to prevent 33 transference of material. Bacterial smear Equipment: Bacteriological Loop. Slide (clean and dry). Drop of water (If the culture medium is solid) Bunsen burner Specimens [growth of microorganisms in Liquid media Solid media Pathological samples ( liquid or solid) Swab (pus, ear, wound, vaginal ,urethral) Sputum C.S.F. (Cerebrospinal fluid) Urine (after centrifugation) 34 stool,tissue A//Making of dry smears from liquid media: Procedure: 1. Sterilize loop in Bunsen flame. 2. Using aseptic precautions االحتياطرات, with draw one loop full of culture. 3. Transfer this to a clean slide 4. spread it with the loop to form a thick film of liquid. 35 5. Sterilize the loop. 4-Allow the film to dry without heating 5-pass the slide 3 times through the Bunsen film flame. This fixes bacteria to the slide. 6-Allow the slide to cool, and then stain the film by the requisite method. B//Making of dry smears from solid media: Aseptic precautions must be observed during the manipulation of culture tubes or plates. 1. Place one drop of distilled water on a clean slide by sterilized loop 36 2. Sterilized loop. 3. With the loop transfer to the slide a small portion of the growth to be examined and Emulsify it in the drop of water until a thin homogenous film is produced. 4. Sterilize loop in Bunsen flame 5. Allow the smear to dry ( air ) 6. Fix by rapidly pass the slide 3 times through the Bunsen film flame. Fixation preservation of morphology but NOT internal structures -Cellular enzymes are inactivated 37 -Cell structures are hardened kills organisms(Organism dies) [usually results in the death of the attached microorganisms] adheres specimen strongly to the glass slide promotes stain ability of specimen Types of fixation: A//Heat fixing: 1-flame heating bacterial film Pass slide through flame quickly 3-4 times Heat fix too little and organisms may wash off slide Heat fix too much and organisms may be distorted B//Chemical fixation: 38 *chemical fixatives penetrate cells *Preserves fine substructures and morphology *Fixative chemicals penetrate cells and react with proteins and lipids; (preserves intracellular components) make them inactive, insoluble and immobile. 1. e.g.:-Acetone, Ethanol, Acetic acid, Mercuric chloride, Formaldehyde, Glutaraldehyde Quiz1 Fill in the blanks with suitable answer :1. The advantage of preparing wet smears is to observe_________. 2. Preparing dry smears is to observe__________. 3. There are two types of fixing bacterial smear ___________and_________. Note - Check your answers in key answer page. 39 Staining of smears: Kinds of bacterial stains 1. Simple stain 2. Compound stain 3. Negative stain Negative stain Simple stain 1-Staning around the cell 1-only one dye, one step 2-to know the morphology of cells(shape and aggregation) 2-one dye or more eg:1. Methylene blue (blue) 2. Methyl violet (blue) 3. crystal violet (blue) 4. Natural red (red) 5. Safranin (red) 6. carbol fuchsin (red) b--- Special stain 40 a---Differential stain Differential stain Special stains 1-more than one dye Mo more than one dye 2-to stain special part of cells eg:- 2-tt to differentiate between two groups 1. Acid fast stain (Z-N stain) of bacteria 2. Albert's stain 3. spore stain eg:-Gram's stain: 4. capsule stain 1. Acid fast stain (Z-N stain) , 5. flagella stain Ziehl Nelsen stain (tuberculosis). 2. Albert's stain (Corynebacterium) Simple stain diphtheria o One reagent o Usually involves basic dyes Crystal violet Methylene blue Carbol fuchsin Most microbes bind basic stains (+ charged dye) because surfaces have lots of negative charges Typical examples are crystal violet and methylene blue) Used to stain outer surface, so used to look at morphology, size and cell arrangement equipment :- Staining rack. loop Slide. Source of heat. bacterial growth simple stain (Crystal violet or diluted Carbol fuchsin) filter paper 41 distil water 70%alcohol procedure :1- clean and dry slide with 70%70%alcohol 2-prepare bacterial smear 3-fixation the smear 4-put the slide on staining rack. 5- Stain the smear using any simple stain folded the smear by few drops of stain, let it for 1-2 min. 6-pour the stain from the slide 7-wash the slide by tab water upside. 8-Let it to dry in air or with filter paper. 9-exzmin the stained smear under Microscope by oil (100X) Differential stain Gram's stain: In 1884, Gram described this method which is the most important stain in routine bacteriology. It divides bacteria into two categories depending on whether they can be decolorized with acetone, alcohol, or aniline oil after staining with one of the rosaniline dyes such as crystal violet, methyl violet, or gentian violet, and treating with iodine. Those that resist decolorization remain blue or violet in color and are designated gram positive, those that are decolorized and take up the red counterstain such as natural red, safranin or dilute carbol-fuchsin are termed gram negative. 42 Although many investigators have tried to uncover the mechanism of the gram reaction, no universal answer has yet been found and it is possible that more than one mechanism exists. Reagents of gram staim Solution 1: (primary stain) Methyl violet 6B (CI No. 42555)………..0.5 g Distilled water ………………………………………100 ml Dissolve the methyl violet in distilled water and filter. Record date and label. Solution 2 (mordant): Logols iodine iodine……………..…………10 g potassium iodide….………….20 g distilled water………..……….1000 ml Dissolve the potassium iodide in about 50 ml of water, add the iodine, dissolve by shaking and make up to the final volume. Record date, label and store in a tightly stopper bottle. Solution 3:(Decolorizor) Absolute ethyl alcohol 95%or Acetone Solution 4 (Counter stain) Natural red OR Safranin OR dilute carbol fuchsin Procedure: prepare a smear, allow to dry and fix with gentle heat. 43 1. Stain with solution 1 crystal violet (primary stain). for 1-2 min 2. Treat with Iodine (solution 2) solution (mordant) for 1-2 min. to increase interaction between cell and dye. 3. rinse with Decolorizer 95% ethanol (solution 3) and continue application until no more color appears to flow from the preparation.30sec. 4. 5. wash with water. Apply Counter stain ( solution 4 ) safranin, for 1 min. (If dilute fuchsin is sued, stain for 30 sec.). 6. Rinse with water. Blot carefully and dry with filter paper. 7. examine the stained smear under Microscope by oil (100X) 44 Gram-positive bacteria remain dark purple 45 Gram-negative bacteria pink to red Table: reaction of some organisms to gram's stain Gram positive Gram negative Staphylococcus Coliforms Streptococcus Neisseria Pneumococci Vibrios Corynebacteria Spirochetes Mycobacteria Salmonella Bacillus group Shigella Hemophylus group Quiz 3 1. What are the main types of staining with examples? Steps of stain Primary stain Crystal violet G-ve Blue G+ve Blue fixation Lugals Iodine Blue Blue decolonization Ethanol alcohol Blue Colorless counter Stain Safranin Blue Red 2. What is the procedure of Gram's stain? 46 Primary stain Mordant decolorization 47 5/ Post test:- Circle the correct answer:1. Hanging drop is used for :a- visualizing live bacteria. c-a & b b- Dry smear c- none 2. Differential stain:a- is used to differentiate between 2 groups of bacteria is used more tan one dye cThe result will be either G+ve or d- all 3. Negative stain : a- stains around the cell c- none b- used one dye or more d- a & b 4. Heat fixation used to : a- kill & fix c-fix only b- kill the bacteria only d- none 5. The fixative in Gram's stain is : a-iodin b-safranin c- ethanol d- decolorizer 48 bG-ve 49