Human Genome Project
advertisement

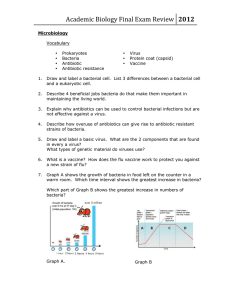
Bacterial Drug Resistance • Discovery of penicillin 1929. – Sir Alexander Fleming. – Accidental mold contamination. • Chinese, Egyptians, Europeans used moldy food to treat infections. Bacterial Resistance • Many bacterial have developed antibiotic resistance. – 80% of Staphylococcus resistant to penicillin. – “Superbugs” resistant to all antibiotics. – Multi-drug resistant tuberculosis. • Misuse of antibiotics accelerates rates of resistance. Sources of Antibiotics Antibiotic Mechanisms Antibiotic Examples • b-Lactam antibiotics (e.g., Penicillin): – Transpeptidase crosslinks the peptidoglycan net in the cell wall of Grampositive bacteria. – The b-lactam ring mimics a component of the cell wall to which transpeptidase binds, inhibiting the binding of transpeptidase. – Bacterium lyse (rupture) because the cell wall is weakened. • Disrupters of nucleic acid synthesis prevent bacterial cell division. – The antibiotic rifampin interferes with prokaryotic RNA polymerase. – Fluoroquinolones inhibit DNA gyrase. • Disrupters of protein synthesis: – Aminoglycosides inhibit nucleic acid or protein synthesis in bacteria. – L-shaped molecules that fit into pockets of bacterial ribosomal RNA. – When they insert themselves into rRNA, they disrupt ribosomal structure. – L-shaped pocket is specific to bacteria. Antibiotic Mechanisms Mechanisms of Resistance • Bacteria either have preexisting resistance to drugs, or they develop resistance. • Often resistance to a certain drug from a particular class leads to resistance to all other drugs in that class. Inherent Resistance • Darwinian evolution: – Bacteria that resist an antibiotic's effects are better suited to survive in an environment that contains the antibiotic. – Genes that confer resistance are transferred to the bacterial progeny. • Bacteria naturally resistant (e.g., Gramnegative bacteria resistant to penicillins). • Bacteria may be resistant because – They have no mechanism to transport the drug into the cell. – they do not contain or rely on the antibiotic’s target process or protein. Acquired Resistance • Bacteria that don’t begin life resistant to a certain antibiotic can acquire that resistance. • Horizontal evolution: – Resistance genes pass from a resistant strain to a nonresistant strain, conferring resistance on the latter. – Presence of a antibiotic is a selective pressure. • Gene transfer mechanisms: – Conjugation. – Transduction. – Transformation. Conjugation • Transmission of resistance genes via plasmid exchange. • Resistance spreads much faster than simple mutation and vertical evolution would permit. Transduction and Transformation • Transduction: Virus transfers gene. • Transformation: DNA released from a bacterium is picked up by a new cell. Examples of Resistance Mechanisms of Resistance • Enzyme-based resistance–break down or modify antibiotic. • Ribosomal modifications–methylation of ribosome interferes with antibiotic binding. • Protein modifications–mutations leave target protein unrecognizable to antibiotic yet still functional. • Metabolic resistance–overcome competitive inhibition by producing excess of metabolite. • Effluxing the toxin–pump it out. Enzyme-Based Resistance: b-Lactamase • Enzymes can destroy or disable antibiotics. • For example, b-lactamase hydrolyzes b-lactam ring of penicillins. • Without a b-lactam ring, penicillins ineffective. Enzyme-Based Resistance: Aminoglycoside Disruption • A bacterial enzyme adds a bulky substituent to the aminoglycoside (such as chloramphenicol). • Antibiotic now does not fit into the rRNA pocket, rendering it harmless. Conclusion • We overuse antibiotics and often neglect to complete a full course of antibiotics once it has been prescribed, leading to the spread of antibiotic resistance. • Resistance can disappear if there is no selective pressure to maintain resistance.