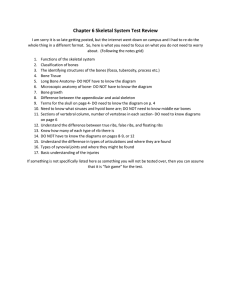
Skeletal System
advertisement

Skeletal System The human hand has 27 bones; your face has 14! You have 206 bones but were born with 300. The longest bone in your body? Your thigh bone, the femur -- it's about 1/4 of your height. The smallest is the stirrup bone in the ear which can measure 1/10 of an inch. Did you know that humans and giraffes have the same number of bones in their necks? Giraffe neck vertebrae are just much, much longer! You have over 230 moveable and semimoveable joints in your body. Skeletal System Functions: Support – hold the body up Protection – protects vital organs from damage – heart, lungs, brain Movement – through the joints Mineral Storage – is a reservoir for calcium Blood cell production – red and white blood cells are produced in the bone marrow Energy Storage – the yellow marrow in adult bones is fat storage Types of Bones Long Bones Needed to support the weight of the trunk & for locomotion Mostly the bones of the limbs Has a main shaft that is cylindrical with two ends The wall of the shaft is made of thick compact bone and only a small amount of spongy bone on the inside At the ends there is more spongy bone with a thin layer of compact bone Examples: femur, tibia, fibula, metatarsals, humerus, radius, ulna, metacarpals, phalanges, clavicles Long Bones Flat Bones: Strong, light, & flat Used for protection Two thin layers of compact bone surrounding spongy bone (amounts of spongy bone vary In adulthood, produces most of the RBC’s Examples: ribs, sternum scapula, cranium, ~pelvis Short Bones: Strength and compaction but not much motion Small bones tied together by ligaments Spongy throughout with a very thin compact layer at the surface Examples: carpals, tarsals (Wrist and ankle bones) Irregular Bones Cannot be groups with any other group Examples: Vertebrae, pubis, Ischium, Patella, Hyoid, Ear bones Epiphyseal Line Articular Cartilage Spongy Bone Epiphysis Medullary cavity ↓ Periosteum ↑ Yellow Marrow Compact Bone Bone Parts Epiphysis – ends of bone (contains spongy bone and early in life makes RBC’s) Epiphyseal Plate – cartilage plate where bones grow Epiphyseal Line – when bone fusion occurs (no more cartilage) and growth is finished Articular Cartilage – covering bone ends Diaphysis – bone shaft Medullary Cavity – center of bone containing some spongy bone and in adulthood is filled with fat (yellow marrow) Periosteum – fibrous connective tissue covering over the bone Parts of the Bone Bone Histology Bone Histology Bone Histology Haversian Canal (central canal) – run longitudinally to bone tissue – carry blood vessels Volkmann Canal – run perpendicular to bone tissue and carry blood vessels Osteocyte – bone cells surrounding Haversian canals in concentric circles Lacunae – spaces in the matrix that the bone cells live in Bone Histology Continued Canaliculi – tiny canals through the matrix connecting each lacunae to the main blood vessels in the Haversian and Volkmann canals Lamellae – concentric circles of matrix formed by the bone cells Osteon – whole bone unit including the Haversian canal, the lamallae and osteocytes that go with that canal Histology Bone Histology Bone Cells Osteoprogenitors – stem cells that create all of the other bone cells. Found in the inner layer of the periosteum. Osteoblasts – the bone cells that are actively creating the matrix – located also on the inner face of the periosteum. Osteocytes – mature bone cells that are fully embedded in matrix and just maintain the matrix. Osteoclasts – specialized white blood cells that live in the bone and chew up the bone matrix and return the protein and calcium to the blood. Matrix – collagen protein hardened with calcium phosphate and calcium carbonate. Bone Remodeling What is it? Constant break down and rebuilding of bone Bone resorption – breaking down bone Caused by action of osteoclasts Bone deposition – building of bone Cause by the action of osteoblasts Bone Turnover Purposes of Bone Remodeling: Turn old bone into new bone Turn spongy bone into compact bone Increase the diameter of the bone (resorbed on inside, built on outside (matrix secreted by osteoblasts on periosteum side) Repair broken bones Regulation of Bone Dynamics Weight bearing exercise (mechanical stress) causes more bone deposition than resorption Availability of aa to form the collagen protein of the matrix Availability of Minerals (lack of minerals, especially calcium, will cause bone to be broken down) Regulation of Turnover Continued Vitamins – lack of vitamins will be negative for bone construction Vitamin C – necessary for collagen synthesis – so needed to make and maintain the matrix Vitamin D – necessary to absorb calcium from blood Hormones – control balance of bone resorption/deposition Estrogen and Testosterone – positive for bone depostion Insulin – needed for bone deposition Calcitonin (Thyroid) – positive for bone depostion when blood calcium is high Parathyroid Hormone – speeds bone resorption when blood calcium is low Osteoclast – multinucleated, modified WBC – “eating bone” Osteoporosis Epidemiology – statistics of a disease – study of a disease in a population Lifetime risk of breaking a hip, radius, or spine is 40% 500,000 hospital stays, 83,000 nursing home stays / year $5-10 billion/yr cost in US ½ with hip breaks never walk again, ¼ stay in rest homes until death Osteoporosis is increasing because we have a large aging population Bone Turnover - Causes of Osteoporosis Loss of bone mass after menopause or low peak bone mass or both Imbalance of bone resorption and formation Negative calcium balance – not enough calcium intake, not enough vitamin D, calcium leeching Loss of hormone - inhibits osteoclasts and may signal osteoblasts (takes 100-150 osteoblasts to form bone destroyed by 1 osteoclast) Lack of exercise Low peak bone mass Higher PTH – activates osteoclasts Risk Factors – make a person more likely to get a condition Being female – men have 30-50% greater bone mass Asian Thin Late menarchy Early menopause (doubles the risk of heart disease and osteoporosis) Heavy drinking and smoking Inactivity Peak Bone Mass Determined By: Genetics collagen gene mutation (makes up 80% of bone) causes bone fragility Vitamin D receptor – polymorphic Estrogen Receptor Bone geometry Gender Ethnic origin African Americans have best bone density > Caucasians > Asians Peak Bone Mass Determined By: Nutrition Calcium intake Vitamin D intake Protein intake Hormones Estrogen Testosterone PTH Peak Bone Mass Determined By: Weight bearing exercise Other environmental factors Tobacco use Alcohol use Hormone Replacement Therapy Pros Increased bone density Increase in collagen – younger skin Decrease menopausal symptoms like hot flashes and vaginal dryness May improve mood Cons Increase risk of heart attack Increased risk of breast, ovarian, and uterine cancer May increase risk of blood clots in legs and lungs Effects are temporary Can’t be taken if have blood clots, migraines, fibroids, endometriosis Side effects – bloating, headaches, mood swings