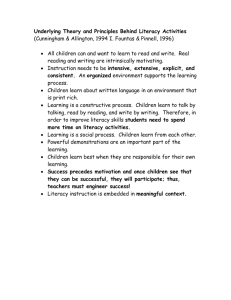
Training Objectives

October is Health
Literacy Month
1) What’s Happening at
UNMH?
2) What Can You Do to
Move UNMH Forward?
Audrey Riffenburgh
Senior Health Literacy Specialist
Office of Diversity, Equity, & Inclusion
Rising to the Challenge
National Action Plan to Improve Health Literacy
(US DHHS, ODPHP)
Promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services.
Groups at Greatest Risk of
Low Health Literacy Skills
Seniors
People living in poverty
People from ethnic minority groups —
Hispanic, Black, American Indian
People with physical, mental or other health problems
People with chronic or long term health problems
Look familiar?
Sources: National Adult Literacy Survey (1993) and
Health Literacy of America’s Adults (2003).
How Much Does the “Person on the Street” Understand?
Health and the City
What is UNMH Doing to Improve
Communication with Patients?
3 Classes in 2012: “Creating Reader-friendly Print and
Web Materials”—
57 people completed
Patient-Friendly Document Committee (and PFEC)
Assisting Health Literacy Specialist in designing system changes to improve patient/family documents, forms, and more
Health Literacy Task Force
Assisting with raising awareness, Health Literacy Month, and educating clinicians about health literacy
Resources Online
Diversity, Equity and Inclusion website
Health Literacy Month
Activities
Health Literacy Fair — October 2-3, 2012
Combined forces to celebrate national Quality, Library, and
Pharmacy Week or Month
Showcased “before” and “after” documents, PDSAs, quality initiatives, “teach back” for checking patient comprehension
Bulletin boards at main
Packets to offsite clinics for staff education
This presentation
Health Literacy Month
Activities (continued)
Coming soon: extensive plain language thesaurus on intranet
HSLIC Health Literacy LibGuide: http://libguides.health.unm.edu/ and click on
Health Literacy
Check it Out!
Here is a recently revised document from
UNM Hospitals
See if you can spot the changes!
Original Parent Discharge
Checklist (NBICU & ICN)
Final Parent Discharge
Checklist (NBICU & ICN)
Key Changes
Checklist format for easier usability
New heading and more instructions re: P-G
Survey to draw attention
Phrased to speak to reader, not about reader — e.g., “your hospital stay” instead of “Mother’s
Hospital stay”
More conversational language — e.g., “taking your baby home” instead of “discharge”
Coming Attractions at UNMH for
Improving Communication with Patients
“Document clinics”/work sessions (for those who have taken the class)
Style guides/sample layouts for standardizing and improving patient documents
Intro/awareness sessions on health literacy offered for your staff meetings
More classes in 2013
In 2013, more focus on verbal communication
So, you’ve heard about the exciting work on patient communication.
What can you take back to your worksite that will make a difference?
Working Effectively with Patients
Challenged by Health Literacy and Limited English Proficiency
Bronwyn Wilson MD
Department of Internal Medicine
Sr. Associate Dean for Academic Affairs
How Patient-Friendly Is my Unit?
Imagine you are a new patient with limited health literacy who comes to your unit.
What happens now? Where do you go?
Whom do you ask for help?
What if you are embarrassed by what you don’t understand and don’t ask many questions?
Now imagine that you don’t speak English very well either…..
Behaviors that May Indicate
Low Health Literacy
1.
Trouble navigating the healthcare system
2.
Patient registration forms incomplete or inaccurately completed
3.
Frequently missed appointments
4.
Anger or frustration with staff/providers
5.
Unable to name medications or explain timing/purpose
6.
Lack of follow-through with lab tests, imaging, referrals
Patient-Friendly Procedures
1.
Exhibit general attitude of helpfulness – notice when a patient is confused and suspect lower health literacy
2.
Create a shame free environment
3.
Use clear and easy-to-follow signs
4.
Insure forms are at 7 th - 8 th grade level
5.
Provide assistance with completing forms
6.
Review instructions for tests, procedures using
“teach back” method
Patient Interview Techniques
1.
Slow down
2.
Use plain, non-medical language and references to everyday life (“your heart is like a pump”)
3.
Ask simple questions, one at a time
4.
Show diagrams, pictures and models
(Google images are very helpful)
5.
Limit amount of information – focus on 2-3 key points
6.
Use the “Teach Back” method to check for understanding
“Teach Back” Method
You do not want your patients to feel this is a test. Place the responsibility on yourself :
" I want to make sure I have been clear…
Can you tell me how you will explain this to your family when you get home?”
Can you please explain back to me what this medicine does?”
Please tell me what you think the next steps are from what I’ve told you?”
Remember, we want our patients to feel comfortable and satisfied with their care
The majority of our patients have limited health literacy, especially if they are worried about their health or don’t speak English well.
Most of our patients do not understand how to fill out complex forms, nor the patient satisfaction surveys that we send them.
We can help them by working together at all levels to improve their experience and enhance their health outcomes.
To Learn More, Share Ideas,
Request a Talk, or Get Help...
Contact:
Audrey Riffenburgh, MA
Senior Health Literacy Specialist
Office of Diversity, Equity, and Inclusion
272-5101
Bronwyn Wilson, MD
Office of Academic Affairs
272-8268