health applications of bayes techniques
advertisement

Population Health
Perspectives
1
Peter Congdon
Research Professor of Quantitative
Geography & Health Statistics, QMUL
e-mail: p.congdon@qmul.ac.uk
http://www.geog.qmul.ac.uk/staff/congdonp.html
http://webspace.qmul.ac.uk/pcongdon/
2
Major tasks in definition and analysis
3
4
Upstream & downstream determinants of
health (Kaplan, 2004)
5
6
To describe/analyze health variation over
areas or area categories (poverty status, area
socioeconomic classifications, “deprivation
quintiles”)
by area SES scales (deprivation gradients), or
other area characteristics (social
“fragmentation”, social capital)
according to area environmental exposures
(e.g. pollution levels or categories)
7
8
9
To describe health variation over
demographic categories (age, race, gender, family
type)
individual socioeconomic variables (income,
education)
health behaviours (smoker or not, obese or not)
Assess how individual and contextual factors (aka
upstream & downstream factors) interact in their
impacts on health
10
Assess
which potential sources of
variation in health are significant
(or not)
Summarise health variations
parametrically
Provide stable estimates
11
12
Assess how health need (need for
healthcare) is distributed over areas or
social groups
to guide distribution of scarce health
resources and effective targeting of
healthcare interventions
May involve “health need indices”
based on characteristics of areas or
area populations
13
14
A major focus of my talk will be on models for
spatial variations in health, and predictors of
those variations (“ecological studies”)
These models typically use area counts
(deaths, incidence or prevalence totals) from
official registration systems
Statistical models often seek to assess the
implications of area health variation (e.g.
locating areas with excess risk, ranking areas
according to health risk, measuring inequality,
smoothing ragged observed area rates).
15
Relevance of “ecological studies” (despite
“ecological fallacy”) to broader
upstream/downstream debate: what are
contextual effects, what causes them, how
should they be modelled, etc
Crude rates for rare events unreliable
stabilized/robust/smoothed area health
outcome rates essential to accurate
description of population health.
Smoothing may draw on spatial structure of
known or unknown risk factors
16
17
18
19
I will also consider multilevel perspectives
Assess how individual and contextual factors
interact in their impacts on health, e.g. area
variables may act as effect modifiers for individual
risk factors.
Health surveys (e.g. Health Survey for England,
Behavioral Risk Factor Surveillance System) are the
most suitable for analysing the effects on health of
age, ethnicity, and individual SES, and their possible
modification by geographic variables.
But administrative or census data also can be
analyzed profitably by ML methods
20
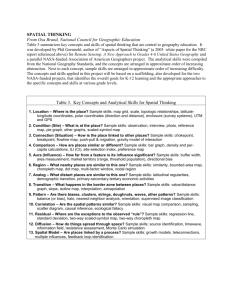
RELEVANT METHODS
Some distinctive aspects of methodologies for
modelling population health
1
2
3
4
5
6
7
APPLICATION THEMES
Assessing varying health risks in areas
Spatially varying predictor effects
Age and area: life table methods
Spatial aspects of health care use
Multilevel modelling
Prevalence Modelling
Common Spatial Factor Models
21
22
General linear models (e.g. with count or
binary response) more frequently used than
linear models
For health survey data often need binary
regression, with logit or log link, and maybe
accounting for differential survey weights
For area counts of health events (e.g. deaths,
prevalence) typically need Poisson or binomial
or over-dispersed versions of these densities
23
Often use random effects to pool strength (or
borrow strength) over areas or other relevant
dimensions (e.g. age)
Essentially refers to adding stability/precision
to estimates by referring to overall population
density
Maybe pool strength over variables too
multivariate random effect and common
factor models
24
In area health applications, both outcomes (e.g.
mortality or prevalence) and ecological risk
factors (e.g. area deprivation, area smoking
rates) are typically spatially structured. Also
applies to “unknown” risk factors
So in statistical models, spatially correlated
random effects often involved (in Bayesian
terminology “spatial priors”)
Modelling aims to account for spatial structure
Inter alia, a good model will ensure regression
residuals are free of spatial correlation
25
In multilevel modelling effects of individual
risk factors may vary according to area
contexts
For example, ethnic relativities in diabetes
prevalence may not be constant over areas
So use random effects (maybe spatially
structured) to model spatial variation in
impacts of individual level risk factors
26
Bayesian approach using MCMC sampling assists in
monitoring “derived parameters” or outputs,
providing full densities, and in testing hypotheses
about derived parameters.
Classical estimation typically provides confidence
intervals under assumed asymptotic normality for
model parameters only, with delta method for
derived parameters
Bayesian approach arguably more flexible for
models with multiple or nested random effects, or
where there is partially missing data
27
An example of a
derived model output
that is not the model
response. Model
response (Poisson) are
deaths by area & age.
Derived model output
is life expectancy
EASTERN REGION OF
ENGLAND, MALE LIFE
EXPECTANCY.
Ref:
Congdon ,
2009, International
Statistical Review
28
Many relevant risk or outcome variables for
analysing population health can be regarded
as latent constructs, not directly observed but
proxied by several observed variables
Examples in area studies: area unemployment
or rates of social housing are proxies for area
construct “deprivation”
Examples in survey studies: battery of survey
items on neighbourhood perceptions and
trust are proxies for individual level construct
“social capital”
29
ASSESSING
VARYING HEALTH
RISKS IN AREAS
30
Observed data (e.g. death totals by area i)
are y[i], and E[i] are expected event totals.
Limitations of conventional (fixed effects)
maximum likelihood estimates of relative
risks (or “standard mortality ratios”) y[i]/E[i]
as description of spatial contrasts.
OR data might be y[i] and populations P[i],
MLE (e.g. crude death rate) is y[i]/P[i] (or
such rates feed into “age standardised” rate)
OR data: y[i] (infant deaths) and births B[i].
MLE is y[i]/B[i]
31
Maximum likelihood approach (underlies
conventional demographic techniques)
treats each area (or risk category) as a
separate isolated entity, taking no account
of:
overall average for the event,
the location of the area, or risk category in
relation to other areas (or risk categories)
By neglecting the broader context, MLE
estimates also potentially unstable
32
Under Bayesian random effects, information
on the pattern of disease risk across the
collectivity of areas (or risk categories) is
used to provide an estimate of the underlying
relative risk for each area (or risk category)
Treat each area’s outcome with reference to
the ensemble of areas
The “prior” specifies the chosen overarching
density of relative risk (e.g. normal or
gamma) and whether or not the density
specifies local or global pooling of strength.
33
However, may be unwise to uncritically assume
complete spatial dependence - or homogenous
spatial correlation.
So allow for some unstructured variation or for
spatial outliers
Spatial outliers: areas unlike their neighbours,
e.g. socially dissimilar (example, suburban “social
housing” estates surrounded by owner occupied
housing areas)
Allow extent of spatial dependence to vary across
the map
Congdon, 2008, Statistical Methodology
34
Use of spatial risk modelling for policy inferences
One may assess for example, the posterior
probability that a particular area has an elevated
relative risk (compared to the average)
Assume RR=1 on average. Then simply count the
proportion of MCMC iterations where condition
RR[i]>1 holds
More complicated to do this under frequentist
approaches
e.g. Congdon, Health and Place, 1997, article on
area contrasts in suicide and attempted suicide in
NE London
35
36
EXTENDING
THE SMOOTHING
PRINCIPLE: Spatial
Heterogeneity In Regression
Effects
37
Spatial pooling of strength may be applied not only
to disease risks but to effects of area risk factors.
Example: how are lung cancer incidence relativities
i affected by area smoking rates xi
Conventionally assume constant slope on xi over
all areas
However, risk relationship may vary (smoothly) over
space varying slopes i
e.g. Congdon, Health and Place, 1997, article on
area contrasts in suicide and attempted suicide in
part of NE London (x=deprivation)
38
39
40
EXTENDING
THE SMOOTHING
PRINCIPLE: Smoothing over
areas and ages to derive small
area life tables
41
Modelling mortality data yix (and maybe illness
data hix too) by both area i and age group x
As before, neighbouring areas have similar
rates under prior incorporating spatial
dependency
But also assume neighbouring ages have
similar rates under pooling (random effects)
prior
Technically, often use “state space” or
“random walk” priors for age effects
42
43
Congdon 2006, Demographic Research, A model for
geographical variation in health and total life
expectancy
Spatial Framework, 33 London Boroughs, ca 230k
population on average
Use illness data (long term ill status from 2001 UK
Census) as well as deaths data (bivariate outcome)
With mortality and illness data can model both total
life expectancy and healthy life expectancy difference between expectancies is expected years
lived in disability (“disease burden”)
Correlation between disease burden & area
deprivation
44
45
Calculate life expectancies Eix for areas i and
ages x using usual life table calculations and
“smoothed” age and area specific mortality
rates Mix
Life expectancy at birth Ei0.
Monitor “derived outcomes” Ei0 in MCMC
whereas likelihood for deaths uses Mix (“actual
model parameters”)
Problems with conventional calculations for
life expectancies when populations small,
rates Mix unstable apply Bayesian random
effects smoothing
46
Congdon (2007) A model for spatial variations in life
expectancy; mortality in Chinese regions. Int J Health
Geographics
Negative binomial model because of large death
counts/overdispersion but allowing for correlated area
and age effects
47
FEMALE LIFE EXPECTANCY CHINA 2000
48
Similar ideas apply if the second dimension is
time rather than age
Correlation between adjacent times is
expected and should be included in the
model
For example, could have “random walk” in
time parameters
49
Congdon, 2004, J Appl Stat “Modelling Trends
and Inequality in Small Area Mortality” has
three dimensions: area, age, time (years) in an
analysis of area mortality through time
“Derived outputs” monitored by MCMC are
Theil and Gini indices of inequality in life
expectancies Eit between areas i =(1,..,n) at
year t.
If Rit=Eit/Et where Et is average, then Theil
entropy index in year t is
Ht=i [Ritlog(Rit)]/n
50
51
Mortality, prevalence and incidence variations
between areas reflect primarily population
health need (e.g. age/ethnicity/SES
composition), maybe together with area
contextual effects
But health care use in different areas (e.g.
hospitalisation rates) affected not only by
population need but by health supply factors
& efficacy of different health sectors
Same applies to flows f[i,j] from areas i to care
providers j, e.g. of acute (hospital) care
52
For example, emergency hospital use in different
areas i affected (inter alia) by
area deprivation, age structure, etc
efficacy of primary care in handling chronic disease
(and preventing “ambulatory sensitive” emergency
hospital admissions)
access to primary care (e.g. primary care physicians
per head, adequate “out of hours” cover)
referral thresholds
hospital capacity
proximity of area i to hospitals j allowing for
competing/intervening populations in other areas
53
Gravity models for flows f[i,j] from area i to providers j
take account of:
Population sizes in areas i (maybe weighted for need)
and capacity of hospital provider j (e.g. bed mass,
staff)
Efficacy of, and access to, primary care
Distance decay (home to hospital distances)
Relative accessibility R[i,j]: capacity B[j] of providers j
adjusted for distances d[i,j] relative to other providers
Can model situation of new sites, or hospital closures
(via Bayesian “predictions”) using implied changes in
R[i,j]
54
Congdon 2001 Health Care Management Sciences
55
Multilevel models
56
Usual paradigm: want to assess effects on
health of
Compositional variables (individual level
risk factors)
Contextual influences (area variations)
Interplay between composition and context
Example is additive effect: poor people
more likely to smoke, but poor people living
in deprived areas more likely to smoke than
poor living in less deprived areas.
57
For example suppose yij is binary health
status (e.g. whether long term ill) for
individuals i in areas j, and xij is individual
level measure of socioeconomic status (e.g.
years of education).
Then ij=Probability(yij=1)
Logit regression to predict ij,
ij=1/(1+exp(-ij)
Intercept variation only ij=j+xij
Intercept and slope variation ij=j+jxij
58
Are there “place effects”: does inter-area health variation
(intercept variation) remain when individual risk variables
are added into the model
Conversely are effects of individual variables diminished
when area effects added
Explaining “contextual variation” or “place effects” in
substantive terms. Which aspects of areas cause
contextual effects (e.g. “healthy food access”, deprivation
amplification, residential segregation)
How should (known and unknown sources of) contextual
variation be modelled (e.g. spatial prior or not)
Do impacts of individual risk factors vary by area
(interaction between levels). This includes slope variation,
as well as more complex forms for categorical predictors
(e.g. multivariate conditional autoregressive prior)
59
Neighbourhood access to healthy
environments, positive health choices
Access to healthy food outlets (e.g. work by
Neil Wrigley on “Food Deserts” in British
cities). Many GIS studies on access to healthy
food
Access to physical activity facilities also an
influence on child & adolescent obesity
60
Usual paradigm for multilevel model is individual
level observation nested according to higher level
index (e.g. area, school); scheme A
However, to make analysis feasible when there are
many individuals, might turn all individual risk factors
into category form and group observations according
to risk category; scheme B.
Also, sometimes lower level units may be small areas
(“neighbourhoods”), and higher level units might be
larger policy areas; scheme C
61
Binary birth events y at level 1 (e.g.
stillbirth) as well as maternal characteristics
x (mothers age, whether lone mother, etc).
Individual events nested within J=25
districts, in turn nested within K=7 health
authorities (HA’s)
Form risk groups by cross-classifying (a)
maternal age (<20, 20-34,> 35), (b) parity
(null,1-2, 3+), (c) previous still-birth (y/n)
(d) lone mother (y/n).
62
Maximum combinations based on these
factors is 900=(3 x 3 x 2 x 2 x 25), of
which 549 are non-empty.
Can look at contextual effects for both
districts and HA’s in n=549 “collapsed” data
points.
In particular (policy implications): do HA
rankings (monitored by MCMC) change
before and after controlling for risk factors
at both individual and district level
63
64
Reduction of intra-district health gradients (over
small areas) often forms focus of public health
targets. But raises methodological issues…
Study of long term illness (LTI) rates in i=1,..,1332
wards (small areas) within j=1,.,53 districts (London
& Eastern England).
Slope variations: within district slopes j relating LTI
to small area deprivation (binomial data)
Negative intercept-slope covariation, cov(j, j):
stronger deprivation effects occur in districts with
lower LTI rates. Slopes in low LTI districts enhanced
by very low illness rates in some wards.
65
Relates to broader themes of potential
relative deprivation impacts on health:
districts with lower average illness may be
more internally heterogeneous in terms of
small area SES
Not only absolute deprivation or income that
matters for health, but income or deprivation
relative to the average of reference group.
66
GEOGRAPHIC
PREVALENCE
ESTIMATION (based usually
on multilevel modelling)
67
Rising US diabetes levels (Mokdad et al, 2001)
Information regarding small area prevalence
important for effective targeting of diabetes
prevention and resources
Prevalence estimates should incorporate
spatial clustering
ethnic relativities
interactions across levels, e.g. between
demography & area
68
Spatial variation & Clustering
Crude diabetes prevalence rate among adults (source; Behavioural Risk
Factor Surveillance System)
69
In 2007 age standardised rate of diagnosed
diabetes was highest among Native Americans
and Alaska Natives (16.5%), followed by blacks
(11.8%) and Hispanics (10.4%), with whites at
6.6 % (CDC, 2008).
Age gradient for diabetes prevalence varies by
race
Barnett et al (2001) & Casper et al (2000) also
report that ethnic disparities vary by area of
residence (their work is on CHD mortality)
70
Survey regression model based on BRFSS
survey data. Binary multilevel model for
doctor diagnosed diabetes. State of
residence for survey subjects is at level 2
Seek diabetes prevalence estimates for
30,000 Zip Code Tabulation Areas in US
(http://www.census.gov/geo/ZCTA/zcta.html)
ZCTA is not provided as a survey variable.
Instead use survey regression parameters in
conjunction with ZCTA census data (and the
ZCTA’s geographic location) to derive ZCTA
prevalence estimates
71
BRFSS survey model includes age, race, sex, and
education effects together with contextual modifiers
Inclusion of individual risk factors (e.g. age, race) in
survey regression model presumes that such factors
also available in census tabulations for ZCTA
populations.
Any interaction between risk factors in regression
model (e.g. age gradients differing by race) similarly
requires matching census cross-tabulation
However, survey model can include geographic context
variables (e.g. state or county level random and fixed
effects). These are applied according to ZCTA
geographic location
72
Differential risks for race (whites, black, hispanic, other
races) and for education (four categories) (fixed effects)
Fixed regression effects of state level predictors,
(poverty rate & percent rural)
Random differential risks specific to age-race group
(multivariate CAR, dimension 4 by 12)
Race specific spatially correlated effects for continental
states (use multivariate CAR), {sjr, j=1,..,49,r=1,..,4}
Race specific spatially unstructured effects for all states,
(multivariate normal) {ujr, j=1,..,53,r=1,..,4} (includes
Hawaii, PR, Alaska, VI)
73
Census provides education and poverty
breakdown for ZCTAs
However, poverty status not in BRFSS
So education gradient in prevalence from
BRFSS survey model used to adjust ZCTA
prevalence estimates for small area education
mix (“compositional” adjustment)
BRFSS model does shows clear education
gradient in prevalence (steeper for females)
Adjustment ensures ZCTAs with more college
graduates have lower prevalence
74
75
Estimates for a particular ZCTA include
relevant random state effects, s[j,r] and u[j,r]
(applied in prevalence estimates according to
state j the particular ZCTA is located in).
ZCTA estimates also adjust for relevant state
poverty/urbanity effect
Can apply same principle to counties (i.e.
3141 US counties at level 2) but then can’t
easily model random area by race
interactions. Also survey data sparse for
many counties.
76
Use European standard population weights
or US 2000 Census weights to combine over
age/race categories
Provides age standardised prevalence
estimate for all persons
Apply same survey model to different years
77
78
79
80
Congdon (Int J Env Res Pub Hea 2010) uses
random county effect in prevalence model for
joint conditions
Joint response over six diabetes- weight
categories: diabetes (y/n) &
obesity/overweight/normal weight
Using BRFSS again
In fact county random effect is form of
common spatial factor over different
categories of the joint response
81
Application Area 7
82
Most commonly applied when there are many
indicators (e.g. different types of cancer
incidence) and just one common factor
But will give an example of multiple
underlying dimensions
In spatial health applications, the common
factor is usually spatially structured (value for
particular area depends on those of its
neighbours)
Can have “multiple causes” of spatial common
factors as well as “multiple indicators”
83
Pool over diverse outcomes (these are
indicators of the underlying common factor)
as a way of pooling strength to assess
underlying morbidity levels
Some indicators may be infrequent, some
may be subject to partially missing values
(e.g. lung cancer county incidence data not
comprehensive across all US states)
So the common factor pools information of
health relativities over different observed
indicators (and imputes/predicts values where
they are missing)
84
Can use common factor models to develop
univariate indices of “health need” (need for
healthcare based on demographic/social
composition of population & also maybe
taking account of relativities in healthcare
usage) e.g. Congdon, J Geo Syst, 2008
Conventional methods for needs indices (e.g.
Mental Illness Needs Index) are aspatial and
usually based on regressing health activity on
bundle of socioeconomic indices. Need index
then derived from significant coefficients.
85
86
Develop multivariate factor models of
different aspects of area social structure with
relevance to health outcomes
Example: area deprivation, area social
fragmentation, and rurality all relevant to
suicide contrasts
Explanatory ecological model for US suicide
contrasts (male & female suicide 2002-2006)
87
88
89
90
91
92
Education application. Multiple tests are
indicators of underlying ability
But investigator might also want to know
what causes variations in ability.
Potential causes might include gender, parent
SES, type of school, etc
93
Variations in avoidable (“ambulatory
sensitive”) hospital admissions. Usually
unplanned emergencies.
Such admissions typically for chronic
conditions, and in many cases could be
avoided with suitable primary/community
care
94
Possible “multiple indicators” of underlying
“quality of care” factor for GP practices:
Emergency admission rate by practice
Ambulatory sensitive admission rate
Attendance rate (unplanned attendances at
“emergency room” or “Accident and
Emergency Unit” that usually don’t result in
hospital admission)
Possible “multiple causes”
GP practice deprivation
Average proximity of patients (affiliated to
each GP Practice) to hospital
95
Similarly Congdon 2010 (J Stat Comp Sim)
uses mortality and hospitalisation data (as
“indicators”) for CHD need index
Spatially structured need index for 625
London wards (small areas)
But ward income and unemployment act as
“causes”
Adjust spatial prior (Besag et al CAR or
Leroux et al 1999 model) to allow for
predictors
96
97
US prevalence model application based on
BRFSS with bivariate outcome
“Multiple indicators” are six categories
defined by diabetic status and weight band:
diabetic and obese (y=1)
diabetic and overweight (y=2)
diabetic and normal weight (y=3)
non-diabetic and obese (y=4)
non-diabetic and overweight (y=5)
non-diabetic and normal weight (y=6).
98
99
10
0