CQC's Approach to the MCA Compliance
advertisement

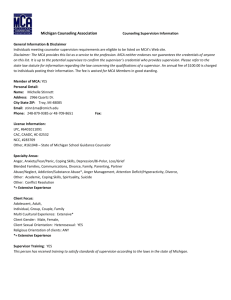
CQC’s approach to Mental Capacity Act compliance Neil Grant Partner, Ridouts LLP 26 February 2014 Care Quality Commission CQC is focussing on Mental Capacity Act compliance Understanding of and compliance with the MCA is patchy CQC also monitors the DOLs system Particular concerns exist around consent issues and best interest decisions This has led to enforcement action which is likely to increase with the planned introduction of the fundamental standards. Compliance with the MCA • Compliance with the MCA is mandatory • The challenge for health and social care professionals is working out what this means in practice • The MCA provides an excellent framework but there is a risk of making assumptions about capacity and best interests • Compliance affords the decision-maker with a degree of legal protection from civil and criminal liability Codes of Practice • Those working professionally with people lacking capacity have a DUTY to have regard to the MCA and the relevant codes. • Two codes: Mental Capacity Code of Practice Deprivation of Liberty Code of Practice Compliance with the MCA Non-compliance might lead to a variety of legal consequences for the provider depending on the circumstances of the case, including: • CQC enforcement • Contractual difficulties • Safeguarding referrals • Neglect findings before a coroner • Claims for damages e.g. negligence or Human Rights Act claims Compliance with the MCA • Registered providers and managers might be subject to CQC enforcement • Professional disciplinary issues e.g. GMC, NMC • Performance management issues involving staff • Criminal liability for trespass and assault • Criminal liability for neglect or ill-treatment Knowledge deficit The problem is that most carers will not have a working knowledge of the MCA (both informal carers and those working in care settings) Even many professionals (particularly GPs) will have a limited awareness of the legislation Even those that do have an awareness of the MCA are at risk of making decisions based on what the courts have described as the “protection imperative” Staff need practical guidance When does a mental capacity assessment need to be undertaken? When do best interests decisions need to be formally taken and who should be involved? What is the test for judging whether someone is being deprived of their liberty? Unhelpful guidance “You should never express an opinion, without first conducting a proper assessment of the person’s capacity to make a decision.” Office of the Public Guardian, making decisions – a guide for people who work in health and social care CQC guidance for providers on capacity “As a service provider, you assess people’s capacity to make decisions as part of their normal assessment and care planning arrangements, whenever this is needed. [my emphasis]” “Assessments of capacity must be made where there may be an ‘impairment of or disturbance in a person’s mind or brain’ affecting their ability to make a particular decision.” CQC the Mental Capacity Act 2005 – Guidance for Providers (Dec 2011) CQC guidance for providers on capacity “Having an illness such as Alzheimer’s disease, mental health difficulties, or a learning disability does not necessarily mean that a person lacks capacity to make all decisions.” “A person may have the capacity to choose what to have for lunch or what to wear, but not whether to take vital medication. Capacity can vary over time, even over the course of a day.” CQC the Mental Capacity Act 2005 – Guidance for Providers (Dec 2011) CQC guidance for providers on capacity “The [MCA] code of practice does not require care services and workers to undertake formal, recorded [capacity] assessments for minor day-to-day decisions about giving routine care.” “You have to use your judgment over whether individual situations are significant enough to need a formal, written assessment of capacity, and who to involve in making an assessment.” CQC the Mental Capacity Act 2005 – Guidance for Providers (Dec 2011) CQC guidance for providers on capacity “As the significance of a decision increases (and significance must be judged for each person individually), the assessment and decision-making process – who is involved and how is it recorded – should become more detailed.” CQC the Mental Capacity Act 2005 – Guidance for Providers (Dec 2011) Capacity - what CQC will be looking for • The service has a copy of the MCA codes of practice • Induction and training for staff includes learning about how the MCA codes of practice affect their work • Staff are aware of the codes of practice and when assessments of capacity are needed • Two-stage assessments of capacity have been made and recorded whenever needed CQC questions about capacity Are your assessment and planning records for care, treatment and support consistent with the MCA’s code of practice guidelines? Do staff giving care, support and treatment know how detailed different assessments of capacity should be? Mental Capacity Mental Capacity – The Task • The ability to make a decision • Is the person able to make the specific decision required, at the time it needs to be made? Capacity – Starting Points • Capacity is presumed • Incapacity must be proven • Standard is balance of probabilities • Assessment of capacity can be carried out by lay persons as well as professionals. Assessing Capacity - Stage 1 1. Does the person have an impairment of the mind or brain, or a disturbance affecting the way their mind or brain works? (it can be temporary, it doesn’t have to be permanent) 2. If so, does that impairment or disturbance mean that the person is unable to make the decision in question at the time it needs to be made? Assessing Capacity – Stage 2 • Does the person have a general understanding of what decision they need to make and why they need to make it? • Does the person have a general understanding of the likely consequences of making, or not making, this decision? Assessing Capacity – Stage 2 • P is unable to make a decision if unable: • (a) to understand the information relevant to the decision, • (b) to retain that information, • (c) to use or weigh that information as part of the process of making the decision, or • (d) to communicate his decision (whether by talking, using sign language or any other means). Mental Capacity in the Care Setting Service users with capacity have the right to make decisions about their lives. This includes: • Whether to take or refuse medication; • When to get up and to sleep; • What to wear; • Where to spend their days Assessing capacity • Capacity assessments should be undertaken in the context of developing (and keeping under review) excellent care plans. • NYC v PC and PC (Court of Protection): sometimes the decision might be generic e.g. can the person make any decision about their care owing to their degree of dementia? However, other decisions may be specific in nature e.g. a particular type of treatment. • The specific circumstances may be relevant e.g. fluctuating capacity. • Also do not need to understand all the details – salient factors sufficient. Best interests Best interests • Best interests are at the heart of the MCA and the MCA determines how to make decisions for those who lack capacity. • See Chapter 5 of Code of Practice. • The person who has to make the decision is known as the ‘decision maker’ and for day to day care that is the person making care arrangements i.e. carer or manager. Best interests – section 4 checklist • Best interests should not be made on assumptions about age, appearance, condition or behaviour. • All relevant circumstances should be taken into account e.g. risks and benefits. • Every effort should be made to encourage and enable the person who lacks capacity to take part in making the decision. • It may be possible to delay the decision until the person regains capacity. Best interests – section 4 checklist • Past and present wishes and feelings, beliefs and values should be taken into account. • Views of people close to the person should be considered, as well as the views of an attorney or deputy. • NB – special considerations apply to life-sustaining treatment, though this is likely to be a matter for medical professionals rather than carers. • Practice point – record best interests decisions and consult widely. Protection for carers A person (D) who takes reasonable steps to establish whether P lacks capacity in relation to the matter in question, and (b) when doing the act, D reasonably believes— (i) that P lacks capacity in relation to the matter, and (ii) that it will be in P's best interests for the act to be done. does not incur any liability for doing that act that he would not have incurred had the person had capacity and consented. Section 5 (paraphrased) Section 5 in practice • For care homes, main application is for decisions around personal care. • E.g. helping with washing, dressing, personal hygiene etc. • Also applies to lifestyle choices e.g. helping service users to participate in social and educational activities • More substantial life changing choices may require further steps, e.g. Independent Mental Capacity Advocates (IMCAs) for residence changes or safeguarding. Section 5 in practice • See Chapter 6 of Code of Practice. • The care plan should include a capacity assessment when necessary. Where the conclusion is that the resident lacks capacity, agreement as to what actions are in the resident’s best interests. • Consideration of whether decisions can be postponed until capacity is regained. • Consideration of least restrictive options. • Careful documentation of decisions, including regular reviews of capacity and best interests. Section 5 and Restraint • Additional considerations apply. • Is restraint necessary to prevent harm to the person who lacks capacity? and • Is restraint a proportionate response to the likelihood of the person suffering harm and to the seriousness of that harm? • NB –the provisions do not allow deprivation of liberty. That requires authorisation under DoLS. Restraint • Very broadly defined • Can cover restricting someone’s movements in a service • Not just physical restraint • Important to ensure the legal requirements are met to avoid potential criminal liability for trespass or assault. Advance Decisions to Refuse Treatment • • • • • • • • Made when person still has capacity. See Code of Practice Chapter 9. Binding if valid and applicable. Valid if not withdrawn or overridden by LPA, or person has acted in a way which is clearly inconsistent with the advance decision. Applicable if clearly relates to the treatment in question. Covers treatment not care. Special rules applies to life sustaining treatment. More applicable in health setting. Seek legal advice if appropriate. Advance Decisions to Refuse Treatment • The Department of Health has stressed the importance of GPs and district nurses working with care providers in dealing with advance decisions around end of life care • If valid, they need to be respected. • We come across situations where locum GPs and ambulance crews have not respected advance decisions. Lasting Powers of Attorney • People who have capacity can appoint attorneys under a LPA. • 2 types of LPA Personal welfare LPA – check to see if there are any restrictions. Property and affairs LPA. An attorney only has power to give or withhold consent to the carrying out or continuation of life sustaining treatment if the LPA expressly so provides. So always check the LPA!! Court of Protection Deputies • Appointed by the Court of Protection to make decisions for a person lacking capacity. • Can be e.g. family, directors of social services, professionals • Deputies can also deal with personal welfare decisions e.g. accommodation, complaints, day to day care. • A deputy cannot refuse consent to life sustaining treatment. Best interests decisions and CQC “The checklist applies equally to routine, day-to-day decision-making and will need to be taken into account when setting and reviewing care plans.” CQC the Mental Capacity Act 2005 – Guidance for Providers (Dec 2011) Best interests - what CQC will look for • Written records of assessments and decisions (including why, when and how decisions were made and who was involved) • Whether staff are aware of the decision-maker’s section 4 checklist • Whether people and their supporters confirm that the person’s past and/or present wishes have been taken into account CQC change in the law – summer 2012 Since 18 June 2012, CQC has been able to enforce the section 4 MCA checklist via Regulation 18 of the Regulated Activities Regulations: “Section 4 of the MCA 2005 (best interests) applies for the purposes of this regulation as it applies for the purposes of that Act.” So CQC can take enforcement action in respect of non-compliance with the MCA. Typically this has been via the service of warning notices. Recent Supreme Court case Aintree University Hospitals NHS Foundation Trust v James [2013] UKSC 67 Mr James was a seriously ill man aged 68 who had been in intensive care for 7 months. The hospital trust sought a declaration from the Court of Protection for declarations as to the lawfulness of withholding further invasive treatment and CPR. First instance judge refused to make absolute declarations but the Court of Appeal decided that the declarations were in his best interests. The Aintree University Hospitals case Sadly Mr James died but the Supreme Court granted permission to appeal. Some key points: • Court of Protection has no greater powers than the patient would if he had full capacity. Patients cannot demand that doctors administer treatment which the doctor considers is not appropriate. • The question for the court is whether it is lawful to give treatment not whether it is lawful to withhold treatment. The Aintree University Hospitals case Continued: • The patient’s wishes are of central importance in best interests. It is a subjective test, not an objective one. • The Supreme Court considered what was meant by “futility” and “no prospect of recovery” and “overly burdensome” in the Code of Practice to the MCA 2005. • Futility is to be considered as treatment which is “ineffective” or “of no benefit to the patient”. The Aintree University Hospitals case Significantly the Court said that “A treatment may bring some benefit to the patient even though it has no effect upon the underlying disease or disability.” As far as prospect of recovery is concerned, “recovery” meant the resumption of a quality of life which the patient would regard as worthwhile, not one that others (including doctors) would regard as worthwhile. The Aintree University Hospitals case The Supreme Court stated that best interests does not merely encompass medical issues. Assessment of the medical effects of a treatment is only one part of the equation. The court should be cautious “about making declarations in circumstances which were not fully predictable or fluctuating.” So the court did not simply follow the wishes of the clinicians. DNAR decision-making DNAR decision-making Do not attempt resuscitation (DNAR) decisions are an important element of care. Where possible, the individual’s preference should be elicited through advance discussions with them and their relatives and carers. Decisions with Significant Consequences CQC’s guidance talks of a need to involve health or social care practitioners and/or other relevant professionals and experts when an assessment and/or decision has significant consequences, including: • There are disagreements with the person, their family or others about the service user’s capacity to make a decision; • Where a decision not to resuscitate someone is being considered; • Considering whether the person should move to new accommodation or receive care, treatment and support at home So this will include, typically, GPs and in some cases, psychiatrists. DNAR • Only applies to cardio-pulmonary resuscitation (CPR) • Presumption of CPR if no DNAR Order in place. • Regarded as ‘indefinite’ unless cancelled or a definite review is specified • Can be controversial – ethical and legal dilemmas Cardio-Pulmonary Resuscitation • • • • In response to cardiac or respiratory arrest Risk of significant adverse effects Can be traumatic and lead to death DNAR Orders – used when CPR will not work or patient expressed wish not to have CPR • Risk that staff interpret DNAR Orders wrongly. • If in doubt, call an ambulance When is DNAR applicable? • Made by most senior clinician involved in patient care • Usually made during end of life care. • Identifiable risk of cardiac or respiratory arrest. • Must be tailored to the individual circumstances of the patient. Discussing DNAR • No requirement to discuss DNAR if no clear presenting circumstances • Best practice to try to engage early on in the event that something may happen in future • Confront respectfully and sensitively • If don’t want to discuss at the time, try again later on • Document all conversations & outcomes DNAR Forms • No ‘universal’ form used nationwide • ‘Red Form’ (produced by Resuscitation Council) is used in many counties and is usually accepted in the event of a transfer of a patient to another county • It would be useful if Resuscitation Council or others could issue a form that is considered universal to avoid confusion. Legal standing of relatives • If no legal authority, relatives cannot be final decision makers • Relatives help inform the decision making process • The decision should always be taken from the patient’s perspective Issues surrounding DNAR orders Documentation - CQC increased scrutiny Residential care homes without nursing - staff generally don’t have the necessary skills to administer or make informed decision about CPR - No clear guidance, need effective arrangements Recording and communicating decisions • Clear record of decisions • Readily accessible to all healthcare professionals • Communicated upon transfer between services • Person who makes the decision is responsible for ensuring it is communicated effectively What do providers need to do? • Providers have an obligation to make sure appropriate decisions are taken on behalf of their service users. It is not enough to say you simply followed a doctor’s orders. • Ensure DNAR Orders are filled out correctly with the appropriate information and consent included • Advance discussions about end of life care are vital • It is not a ‘one size fits all’ approach • Seek advice When things go wrong Ill-treatment or neglect • Section 44 MCA • An offence for a person (D) who has care of a person (P) to ill-treat or wilfully neglect P when P lacks capacity or D reasonably believes P lacks capacity • Care not defined – Lord Denning from 1954: “the homely art of making people comfortable and providing for their well being so far as their condition allows.” Ill treatment and neglect Capacity in this context: Will be the service user’s lack of capacity to make decisions concerning his or her own care. This emphasises the importance of having proper capacity assessments in place, particularly if a service user refuses care. Ligaya Nursing and R Ms Nursing was prosecuted under section 44 of the MCA for wilful neglect – she was a trained mental health nurse who ran a care home Patient elderly lady with significant learning disabilities (functioned around the level of a 7 year old child) Able to make simple choices but without assistance she would neglect herself Alleged lack of care to patient’s personal hygiene and failing to maintain her room in a clean condition and replace dirty bedding. Ligaya Nursing and R Ms Nursing said that would try and help the patient who would sometimes refuse to accept her help and in circumstances like these she felt it was wrong to override her wishes e.g. the patient expressed a strong dislike for having her toe nails cut until the point they became painful. The Court of Appeal noted that the MCA promotes the autonomy of the individual and that “actions or omissions, or a combination of both, which reflect or are believed to reflect the protected autonomy of the individual needing care do not constitute wilful neglect.” Important to reflect this in care plans/records. R v Patel Nurse convicted for wilful neglect. Appealed to the Court of Protection. Failure to carry out CPR on a patient in a nursing home. Patient had been suffering from pneumonia. This had caused respiratory arrest which in turn caused cardiac arrest. CPR probably would not have saved his life. But test does not include causation leading to suffering or injury to health (which is the test for children). No DNR order in the man’s room or over his bed. Proper medical practice required CPR to be given in those circumstances. Nursing home standard practice was to administer CPR in those circumstances and the policy of the home provided “if in doubt resuscitate”. R v Patel Emphasises the importance of having up-to-date end of life care documentation in place One other case involved a nursing home that had blanket DNAR orders in place (the opposite problem) but these were not patient specific – just signed by a GP and put on the file! Staff misunderstood the remit of the order and decided not to actively support a patient who died. It went to an inquest and a neglect verdict was entered. It is also important to ensure best interests decisions are properly recorded where the patient lacks capacity (as well as a clear record of the decision relating to capacity) Coroner’s case A patient in a care home deteriorated over several days and a doctor was not called. The patient died. Minimal nursing observations were made in the days prior to death. The coroner concluded that an Advanced Care Plan document had influenced the decision not to seek medical attention – this recorded a preference of the family that their loved one should not be admitted to hospital and not resuscitated. Coroner’s case The sister was aware of the ACP but did not understand it to be a direction to staff not to admit her brother to hospital in any circumstances. It was simply recording a preference for him to be cared for in the care home. The coroner was concerned about a lack of understanding on the part of the nursing staff about the MCA. The coroner concluded there had been a gross failure of basic nursing care. Some challenges Embedding the MCA framework across all settings – role for CQC but also local authorities and Clinical Commissioning Groups; Training for GPs and doctors in acute hospitals about the MCA; End of life care – ensuring that providers act lawfully particular difficulties arise in the context of DNAR decisionmaking and End of life care ; and More broadly, entitlement to treatment for the elderly CQC Fundamental Standards Due to be introduced from October 2014 Out for consultation at the moment until 4 April (available on the Department of Health website) Most of these will be directly prosecutable including those linked to MCA compliance – person-centred care and need for consent This means CQC will not have to serve a warning notice first Proposal for unlimited fines (not £50,000 per offence) Selected Resources • • • • • • Internal Policies and Procedures MCA Codes of Practice Office of the Public Guardian booklets Social Care Institute for Excellence resources National Council for Palliative Care booklets CQC guidance Contacts - Ridouts LLP Neil Grant – Partner 020 7317 0347 neil@ridout-law.com Paul Ridout – Partner 020 7317 0341 paul@ridout-law.com www.ridout-law.com