B-Cell Modulation in
Multiple Sclerosis
Riley M. Bove, MD
Partners Multiple Sclerosis Center, Brigham and Women’s Hospital,
Harvard Medical School, Boston, Massachusetts
A REPORT FROM THE 29TH CONGRESS OF THE EUROPEAN COMMITTEE FOR
TREATMENT AND RESEARCH IN MULTIPLE SCLEROSIS (ECTRIMS 2013)
© 2014 Direct One Communications, Inc. All rights reserved.
1
The Traditional View:
Immunopathogenesis of Multiple Sclerosis
The initial step in pathogenesis involves the peripheral
activation of CD4+ T helper (Th) type 1 cells in
response to a stimulating antigen.
The assortment of molecules released, including
costimulatory signals and cytokines, influences the
response profile of the activated immune cells.
The stimulating antigen, probably infectious,
subsequently cross-reacts with a CNS antigen.
Subsequently, activated T cells transmigrate across
the blood-brain barrier by adhesion, chemoattraction,
and active infiltration into the CNS.
Chitnis T, Int Rev Neurobiol 2007;79:43
© 2014 Direct One Communications, Inc. All rights reserved.
2
The Traditional View:
Immunopathogenesis of Multiple Sclerosis
Transmigration of activated T cells across the bloodbrain barrier leads to reactivation of infiltrating cells
within the CNS, which contributes to perivascular
inflammation and injury.
Release of additional CNS antigens may result in the
recruitment of T cells with specificities for additional
CNS antigens, called “epitope spreading,” which may
further propagate a chronic immune response.
Further modifications to this model include the
appreciation of other factors, most importantly ThIL-17.
Chitnis T, Int Rev Neurobiol 2007;79:43
© 2014 Direct One Communications, Inc. All rights reserved.
3
Back to the Bench: Further Discoveries
Macrophage-mediated vesicular demyelination was
replicated in New World monkeys, who developed
chronic relapsing-remitting MS and occasionally
progressive disease, with evidence of remyelination.
Autoantibodies that recognize the immunizing
antigen are deposited within the vesiculated myelin
sheaths in this animal model of MS, and similar
antibodies have been found in human MS lesions.
This discovery implied that humoral immunity might
be a key factor in MS pathogenesis.
CD20+ B cells were then identified in MS lesions.
Massaccesi L et al, J Clin Invest 1992;90:399; von Büdingen HC et al, Eur J Immunol 2004;34:2072;
Genain CP et al, Nat Med 1999;5:170; von Büdingen HC et al, Curr Opin Immunol 2011;23:713
© 2014 Direct One Communications, Inc. All rights reserved.
4
A Possible Role for B Cells in MS
Memory B cells, which can cross the blood-brain
barrier, can trigger cellular-dependent and
complement-dependent cytotoxic effects in the CNS.
B cells can influence the priming of effector T cells by
functioning as antigen-presenting cells.
Abnormalities in B-cell cytokine responses have been
reported in MS patients, and production of cytokines
and chemokines by B cells may be involved in the
formation of ectopic lymphoid-like structures.
B cells may be the reservoir for Epstein-Barr virus
(EBV); EBV infection is a known risk factor for MS.
Hauser SL et al, N Engl J Med 2008;358:676; Kappos L et al, Lancet 2011;378:1779
© 2014 Direct One Communications, Inc. All rights reserved.
5
HERMES Trial: Rituximab in RRMS
Phase 2, double-blind, 48-week trial in 104 patients
diagnosed with relapsing-remitting MS (RRMS) who
were randomized to receive rituximab or placebo
Patients receiving rituximab had lower counts of
gadolinium-enhancing lesions at 12, 16, 20, 24, and
48 weeks; fewer new gadolinium-enhancing lesions;
a smaller T2 lesion volume; and fewer relapses at 24
and 48 weeks, compared with placebo.
Patients receiving rituximab initially experienced
more adverse events than did those receiving placebo
(78% vs 40%, respectively) but not afterward, as
treatment continued (20% vs 40%).
Hauser SL et al, N Engl J Med 2008;358:676
© 2014 Direct One Communications, Inc. All rights reserved.
6
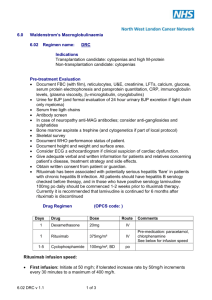
HERMES Trial: Rituximab in RRMS
Number of gadolinium-enhancing lesions in patients receiving rituximab or placebo, from baseline to
week 48. (A) Mean total number of gadolinium-enhancing lesions by week. (B) Mean number of new
gadolinium-enhancing lesions by week. Missing values were imputed by averaging the available data.
Baseline magnetic resonance imaging information was obtained 4 weeks before baseline.
Hauser SL et al, N Engl J Med 2008;358:676
© 2014 Direct One Communications, Inc. All rights reserved.
7
HERMES Trial: Rituximab in RRMS
The incidence of infection (eg, nasopharyngitis,
upper respiratory tract infections, urinary tract
infections, and sinusitis) was similar among the
rituximab and placebo groups (70% vs 71%).
More patients in the placebo group than in the
rituximab-treated cohort discontinued therapy
before week 48 (40% vs 16%).
Rituximab treatment may lead to lysis of memory B
cells in the peripheral blood and lymphoid tissues, as
well as interfere with antigen presentation by B cells
and activation of T cells or macrophages by proinflammatory B-cell cytokines.
Hauser SL et al, N Engl J Med 2008;358:676
© 2014 Direct One Communications, Inc. All rights reserved.
8
OLYMPUS Trial: Rituximab in PPMS
Double-blind, randomized clinical trial in which a
total of 439 patients with primary progressive MS
(PPMS) received rituximab or placebo every 24
weeks over a period of 96 weeks (four courses)
There was no significant difference between
rituximab and placebo in time to clinically definite
progression, defined as an increase in EDSS score
sustained over 12 weeks.
Patients given rituximab had less of a decrease in T2
lesion volume, but total brain volume was similar in
both patient groups.
Hawker K et al, Ann Neurol. 2009;66:460
© 2014 Direct One Communications, Inc. All rights reserved.
9
OLYMPUS Trial: Rituximab in PPMS
Rituximab therapy of PPMS was associated with
delayed time to clinically definite progression in:
» Patients under 51 years of age
» Patients with gadolinium-enhancing lesions on MRI
These subpopulation analyses suggest that:
» Some PPMS patients have evidence of inflammation early in
the disease course, which influences the rate of progression.
» Early, aggressive treatment of inflammation in PPMS may
be beneficial.
» Age-related neurobiologic changes (eg, immunosenescence)
occur in MS and have implications for therapeutic decisions.
Hawker K et al, Ann Neurol. 2009;66:460
© 2014 Direct One Communications, Inc. All rights reserved.
10
On the Horizon: Ocrelizumab
Ocrelizumab, a recombinant humanized monoclonal
antibody that selectively targets CD20+ B cells, might
offer similar therapeutic benefits to rituximab in
patients with MS with less risk of immunogenicity
and infusion-site reactions.
Ocrelizumab is biosimilar but not bioidentical to
rituximab.
In vitro, ocrelizumab demonstrates more antibodydependent, cell-mediated cytotoxicity than rituximab
and less complement-dependent cytotoxicity.
Kappos L et al, Lancet 2011;378:1779; ocrelizumab [data on file], Genentech, 2003
© 2014 Direct One Communications, Inc. All rights reserved.
11
On the Horizon: Ocrelizumab
Kappos et al conducted a phase 2, placebo-controlled
trial involving 220 patients with RRMS who were
randomly assigned to receive 600 or 2,000 mg of
ocrelizumab, interferon beta-1a, or placebo.
At 24 weeks, when compared with the placebo group,
patients given 600 or 2,000 mg of ocrelizumab had
89% or 96% fewer gadolinium-enhancing lesions on
MRI; both doses of ocrelizumab were superior to
interferon beta-1a in reducing the number of lesions.
Two phase 3 pivotal trials in RRMS patients and the
first phase 2 pivotal trial in PPMS patients (the
ORCHESTRA trial) are ongoing
Kappos L et al, Lancet 2011;378:1779
© 2014 Direct One Communications, Inc. All rights reserved.
12
On the Horizon: Ocrelizumab
Number of gadolinium-enhancing lesions by week in patients receiving ocrelizumab, interferon
beta-1a, or placebo. Vertical bars = 95% confidence interval.
Kappos L et al, Lancet 2011;378:1779
© 2014 Direct One Communications, Inc. All rights reserved.
13
Recovery After B-Cell Depletion
The prolonged benefits of B-cell depletion after
exposure to rituximab suggest that protection may
extend beyond the period of B-cell depletion.
Immunologic changes in peripheral circulation:
» Naïve and immature B cells predominate
» Increase in the numbers of interleukin 10-secreting B
regulatory cells and CD25+FoxP3+ T regulatory cells
» Reduction in Th1 and Th17 proinflammatory responses
Immunologic changes in cerebrospinal fluid:
» Decrease in the number of T and B cells
» Resting CD19+ bright B cells predominate
© 2014 Direct One Communications, Inc. All rights reserved.
14
Emerging Studies: MOG Antigen
There may be a repertoire of B-cell-dependent
antigens that might help to elucidate the underlying
triggers in MS.
Myelin oligodendrocyte glycoprotein (MOG), for
example, may be involved in either completion or
maintenance of the myelin sheath; it has emerged as a
potential antigen involved in the pathogenesis of MS.
Studies in B-cell MHC II-deficient mice suggest that a
simple substitution may induce a conformational
change resulting in human MOG antigen becoming
completely B-cell dependent; this protection could not
be restored by injecting MOG antibody.
Weber MS et al, Ann Neurol. 2010; 68:369
© 2014 Direct One Communications, Inc. All rights reserved.
15
Emerging Studies: Oligoclonal Bands
Studies of IgG sequences reveal that oligoclonal B
cells in CSF may be “fingerprints” for MS.
Multiple different oligoclonal bands belong to the
same clone and may respond to a smaller number of
antigenic determinants than the bands would suggest.
Members of these oligoclonal bands were identified in
the CSF and peripheral blood mononuclear cells.
Some B cells found only in the peripheral blood were
associated with oligoclonal bands found only in the
CSF, suggesting some exchange of B cells across the
blood-brain barrier.
von Büdingen HC et al, J Clin Invest. 2012;122:4533
© 2014 Direct One Communications, Inc. All rights reserved.
16
Emerging Studies: Oligoclonal Bands
Lineage trees of multiple sclerosis IgG-VH sequences suggest ongoing B-cell exchange across the blood-brain barrier.
IgG-VH lineages suggestive of ongoing B-cell exchange across the blood-brain barrier for patient MS-1 (A and C), MS-5
(B), and MS-6 (D). These lineages could also reflect affinity maturation occurring in both compartments in parallel. Blue
nodes represents cerebrospinal fluid-derived IgG-VH sequences, red nodes represent PB-derived IgG-VH sequences,
and green nodes represent identical sequences found in both compartments.
von Büdingen HC et al, J Clin Invest. 2012;122:4533
© 2014 Direct One Communications, Inc. All rights reserved.
17
Summary
Anti-CD20 trials have revealed that B cells are central
players in the pathogenesis of focal lesions in MS.
The mechanism of action likely involves blocking the
activation of pathogenic T cells by B cells through a
function of antigen-presenting cells, but it cannot
exclude bystander cytokine effects or autoantibodies.
Not all approaches based on B-cell manipulation are
likely to be effective in MS; some may potentially
worsen the disease.
Targeting resident B cells may soon be feasible.
A properly designed clinical trial could elucidate the
role of B cells in progressive MS.
© 2014 Direct One Communications, Inc. All rights reserved.
18