Communicating with Patients Families and Coworkers
advertisement

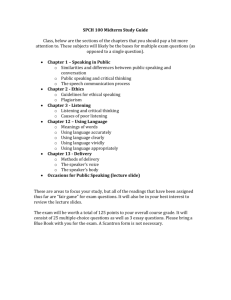
PowerPoint® to accompany Medical Assisting Chapter 4 Second Edition Ramutkowski Booth Pugh Thompson Whicker Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 1 Communication with Patients, Families, and Coworkers Objectives 4-1 Identify elements of the communication circle. 4-2 Give examples of positive and negative communication. 4-3 List ways to improve listening and interpersonal skills. 4-4 Explain the difference between assertiveness and aggressiveness. 4-5 Give examples of effective communication strategies with patients in special circumstances. 2 Communication with Patients, Families, and Coworkers Objectives (cont.) 4-6 Discuss ways to establish positive communication with coworkers and superiors. 4-7 Explain how stress relates to communication and identify strategies to reduce stress. 4-8 Describe how the office policy and procedures manual are used as a communication tool in the medical office. 3 Introduction You are the key communicator between the physician and patient. Your interaction sets the tone for the office visit. Developing strong communication skills are just as important as mastering administrative and clinical skills Communication will influence how comfortable the patient feels in your practice. 4 Examples of Customer Service Telephone techniques Writing or responding to telephone messages Explaining procedures to patients Assisting with billing issues Creating a warm and reassuring environment 5 The Communication Circle MESSAGE Source NOISE Receiver FEEDBACK The communication cycle involves an exchange of messages through verbal and nonverbal means. 6 Maslow’s Hierarchy Self-Actualization Esteem Needs Love Needs Safety Needs Physiological Needs Deficiency Needs 7 Positive Communication Communication promotes patient’s comfort and wellbeing Set the stage for positive communication Encourage patients to ask questions Speak slowly and clearly 8 Negative Communication Look for and ask for feedback to help You curb negative communication habits. • • • • • • • • Mumbling Speaking brusquely Avoiding eye contact Interrupting patients as they speak Rushing explanations Forgetting common courtesies Showing boredom Treating patient impersonally 9 Body Language Facial Expression Eye Contact Posture Open Closed Touch Personal space In many instances, people’s body language conveys their true feelings, even when their words may say otherwise. 10 Improving Communication Skills Listening skills Passive listening Active listening Interpersonal Skills Warmth Empathy Respect Genuineness Openness Consideration and sensitivity 11 Assertiveness Skills Assertive – people who are firm and stand by your principles while still showing respect for others Aggressive – people who try to impose their position on others or try to manipulate them. 12 Therapeutic Communication Involves: Silence Accepting Giving recognition Offering self Giving a broad opening Offering general leads Making observation Involves: Encouraging communication Mirroring Reflecting Focusing Exploring Clarification Summarizing 13 Ineffective Therapeutic Communication Roadblocks: Reassuring Giving approval Disapproving Agreeing/ disagreeing Advising Roadblocks: Probing Defending Requesting an Explanation Minimizing feelings Making stereotyped comments 14 Defense Mechanisms Patients may display: Compensation Denial Displacement Dissociation Identification Introjection Projection 15 Communication in Special Circumstances Anxious Patient Watch for tense appearance, increased blood pressure and breathing, irritability and agitation. Angry Patient Help them express their anger constructively Don’t take it personally Help them refocus toward solving the problem Remain calm 16 Patients with Other Cultures Different views and perceptions Treat all patients of all cultures and ethnic groups with equal respect. Maintain open mind Language barrier Speak through an interpreter to gather and convey information or to discuss sensitive issues with a patient 17 Patients with Visual Impairment Use large-print materials Use adequate lighting in all areas Use a normal speaking voice Talk directly and honestly Do not talk down to the patient Preserve the patient’s dignity 18 Patients with Hearing Impairment Find a quiet area to talk Minimize background noise Position yourself close to and facing the patient Speak slowly Remember that elderly patients lose the ability to hear high-pitched sounds first 19 Apply Your Knowledge -Answer What can you do to promote communication with someone who is visually impaired? Use large-print materials, adequate lighting in all areas, and a normal speaking voice. Talk directly and honestly, but not down to the patient; preserve the patient’s dignity. 20 Mentally or Emotionally Disturbed Determine what level of communication the patient can understand It is important to remain calm if the patient becomes agitated or confused. 21 The Elderly Patient Denial or confusion Act as if you expect the patient to understand Use simple questions and terms Ask the patient to relax Speak slowly Explain points slowly and clearly 22 The Young Patient Recognize and accept their fear and anxiety Explain any procedures Use praise Do not tell children that a procedure will not hurt if it will, or you will lose their trust 23 Patient with AIDS/HIV • You need accurate information about the disease and the risks involved. • You will need to answer as many questions as you can. 24 Terminally Ill Patients Kubler-Ross’ Stages of Dying Denial Anger Bargaining Depression Acceptance 25 Communication with Coworkers Develop rapport Use proper channels. Have a proper attitude. Plan an appropriate time for communication. 26 Communicating with Superiors Keep superiors informed Ask questions Minimize interruptions Show initiative 27 Dealing with Conflict Do not “feed into” others negative attitudes. Be personable and supportive. Refrain from passing judgments. Do not gossip. Do not jump to conclusions. 28 Managing Stress Stress can motivate you Stress can be overwhelming and affect you physically. Learn to manage stress. Be realistic about how much you can handle at work and in your life 29 Burnout End result of prolonged periods of stress without relief. Type A personality Highly driven, perfectionist-type person More susceptible to burnout Type B personality More relaxed, calm, “laid back” Less prone to burnout. 30 Stages to Burnout Honeymoon Awakening Brownout Full-scale burnout Phoenix phenomenon 31 Policy and Procedures Manual Key written communication tool Policies Dictate the day-to-day workings of an office Describes chain of command Procedures Detailed instructions for specific procedures 32 Policies Office purposes Rules and regulations Job descriptions Office hours Dress code Insurance Vacation and sick leave Maintenance of equipment Mailings Bookkeeping Scheduling appointments OSHA 33 Procedures Purpose of test Specimen required and collection method Reagents, standards, controls, and media used Instrumentation Step-by-step directions Calculations Expected values Procedures Limitations of methods References 34 Development of Manual Plan format and organization Create an outline Develop and update material Contact National Committee for Clinical Laboratory Standards (NCCLS) for help 35 Summary Medical Assistant You are the key between the office and patient Communication Skills: People with Special Needs: Listening, interpersonal, and assertiveness Anxious, angry, elderly, hearing and visual impaired Develop working relationships and help office run smoothly. 36 Apply Your Knowledge Developing communication skills for the medical office is as important as mastering administrative or clinical tasks. True or False Good communication requires patient feedback at every step. True or False 37 Apply Your Knowledge -Answer Developing communication skills for the medical office is as important as mastering administrative or clinical tasks. True Good communication requires patient feedback at every step. True 38 End of Chapter 39