Biochem Chapter 18 [4-20

Biochem Chapter 18: The Molecular Bio of Cancer
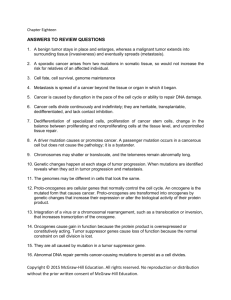
Cancer- term for diseases where cells no longer respond to normal restraints on growth
Normal cells in the body respond to signals, like cell to cell contact (contact inhibition), that tell them to stop proliferating
Cancer cells don’t need growth stimulating signals and are resistant to growth inhibitory signals
Cancer cells also resist apoptosis – programmed cell death to get rid of unwanted or irreparably damaged cells
Cancer cells have an infinite proliferative capacity, and don’t become senescent (they’re immortal)
Cancer cells can also grow independent of structural support, and don’t need anchors like the ECM
Requirement to be cancerous in culture:
Cancer cells don’t need things to trigger them to grow, they can grow on their own o Serum – liquid part of blood
Cancer cells can grow without attachment to a supporting matrix o So no anchorage dependence o Normal cells need to adhere to a substratum (bottom of the disc) when in culture, and won’t grow just suspended in the agar
Cancer cells will form tumors
Cancer is caused by mutation in existing cell genes
A single cell that divides abnormally eventually forms a mass called a tumor
A tumor can be benign and harmless, or malignant o Common warts are benign tumors formed from a slowly expanding mass of cells o Malignant neoplasm (tumors) – proliferation of rapidly growing cells that progressively infiltrate and destroy surrounding tissue o Moles (aka nevi) are tumors of the skin
Formed by melanocytes that have been transformed from single cells, to round oval cells that grow in aggregates or “nests”
Melanocytes form the dark pigment melanin, which protects against sunlight by absorbing UV light
Additional mutations can transform a mole into a malignant melanoma
Tumors develop angiogenic potential, which is the capacity to form new blood vessels and capillaries o So tumors can generate their own blood supply to bring in oxygen and nutrients
Cancer cells can also metastasize- separating from the growing mass of the tumor, and traveling through the blood or lymph to other parts of the body, where they establish new growths of cancer cells
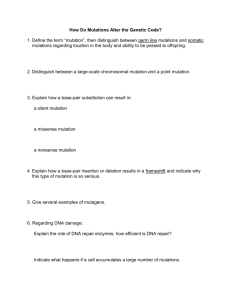
The transformation of a normal cell to a cancer cell begins with damage to DNA , like a base change or break in a strand
Damage can be caused by chemical carcinogens, UV light, viruses, or replication errors
If the damaged DNA is not repaired right, or isn’t repaired before replication happens cancer
A mutation that leads to a transformation can also be inherited
When a cell with one mutation proliferates, this clonal expansion (proliferation of cells arising from a single cell) results in a population of cells having this one mutation
Then another cell from this population can get a 2 nd mutation to control cell growth or death
With each clonal expansion, the probability of another transforming mutation increases
Because mutations happen in genes that control proliferation, subsequent mutations happen even more rapidly until the cells acquire enough of the needed mutations for full transformation
The transforming mutations happen in genes that regulate: o Cell proliferation and differentiation - proto-oncogenes
Proto-oncogenes are genes that regulate cell growth
Mutated forms of a proto-oncogene are called oncogenes o Suppress growth - tumor suppressor genes o Target irreparably damaged cells for apoptosis o Repair damaged DNA
A transforming mutation in a proto-oncogene that increases the activity or amount of the gene product, called a gain-of-function mutation
Tumor suppressor genes and repair enzymes protect against uncontrolled cell proliferation o A transforming mutation in tumor suppressor genes causes loss of their activity, or a decreased amount of the gene product, called a loss of function mutation
So cancer is caused by the accumulation of mutations in the genes involved in normal cell growth and differentiation
These mutations give rise to cancer cells that are capable of unregulated, autonomous, and infinite proliferation
As these cancer cells proliferate, they impinge on normal cell function, leading to symptoms
DNA damage leading to mutations:
A change in chemical structure of DNA, or the sequence of bases in a gene, is a requirement for cancer
The function of DNA depends on polar chemical groups in DNA bases, that can form hydrogen bonds to form a DNA strand o The oxygen and nitrogen atoms in DNA bases are targets for electrophiles (electron seeking chemical groups)
Chemical carcinogens (compounds that can cause transforming mutations) must be activated by body metabolism to react with DNA
Many chemotherapeutic agents, which are designed to kill proliferating cells by interacting with
DNA, may also act as carcinogens, and cause new mutations and tumors, while getting rid of the old
Structural changes to DNA also happen through radiation and UV light o Most skin cancers happen in sunlight-exposed areas o The wavelength of UV light most associated with causing cancer is UV-B o With excessive exposure to the sun, the nucleotide excision repair pathway is
overwhelmed, and some damage stays unrepaired
If the DNA damage isn’t repaired, it introduces a mutation into the next generation when the cell proliferates
Proto-oncogenes are converted to oncogenes by DNA gain in function mutations o Things that convert proto-oncogenes oncogenes:
Radiation and chemical carcinogens can do it two ways:
Cause a mutation in the regulatory region of a gene- this increases the rate of making of the proto-oncogene protein
Produce a mutation in the coding part of the oncogene that will result in the making of a protein with a slightly different a.a. make up, that can
transform the cell
The entire proto-oncogene, or a part of it, can be transposed or translocated
(moved from one part of the genome to another)
In its new location, the proto-oncogene may be under the control of a promoter that is regulated differently than the original
This promoter may allow the gene to be expressed in a tissue where it’s normally not expressed, or express it more than usual
If only a part is translocated, it may be expressed as a shortened protein with changed properties, or it can fuse with another gene and make a fusion protein from parts of two separate proteins o The shorter or fusion protein may be hyperactive and cause inappropriate cell growth
The proto-oncogene may be amplified, so that many copies of the gene are made in a single cell
If more genes are active, more proto-oncogene proteins are made, increasing the growth rate of the cells
If a cancerous virus infects a cell, it’s oncogene may combine into the host genome, allowing making of the new abnormal oncogene protein
The cell may be transformed and grow more
The virus can also just insert a promoter into the host genome, that increases or causes expression of a normal proto-oncogene
o Transformations result from abnormalities in the normal regulation of growth, caused by gain-of-function mutations in proto-oncogenes
Loss of function mutations though can happen in tumor suppressor genes, and their combo with the gain of function mutations is usually needed for full transformation to a cancer cell
Mutations in repair enzymes o Repair enzymes are the first line of defense in preventing conversion of damage in DNA to a mutation o DNA repair enzymes are tumor suppressor genes, since errors repaired before replication will not become mutagenic o DNA damage is always happening from sunlight, background radiation, toxins, and replication errors o Without the repair enzymes, mutations to a growth regulatory gene aren’t fixed o Ex: problem with DNA repair genes BRCA1 and BRCA2 means you can’t repair double stranded breaks, increasing the risk for breast cancer
Proto-oncogenes control normal cell growth and division
They encode proteins that are growth factors, growth factor receptors, signal transduction proteins, transcription factors, cell cycle regulators, and regulators of apoptosis
To name these things, the gene is in lower case and italicized, and the protein is capitalized
Cancerous mutations to proto-oncogenes are usually gain-of-function mutations o So more of a protein is made
Micro RNAs (miRNAs) can behave as oncogenes
Oncogenes of signal transduction: o All of the proteins in growth factor signal transduction cascades are proto-oncogenes o Growth factor and growth factor receptors are proto-oncogenes
Growth factors regulate growth by acting as ligands that bind to receptors, triggering a signal transduction pathway in the cell that will activate transcription of certain genes
If too much of a growth factor or growth factor receptor are made, the target cell may respond by proliferating inappropriately
The receptor can also be mutated into something cancerous
This can make the receptor stuck in the “on” position, and keep sending signals even when there is no growth factor bound o Genes for the proteins in the signaling cascade can also be proto-oncogenes
Ex: binding of growth factor leads to activation of Ras
When Ras binds GTP, it is active, but then Ras slowly inactivates itself by
GTPase hydrolyzing its bound GTP GDP + P
I
This controls how long Ras is active
Ras is made oncogenic by mutations that decrease the activity of the
GTPase of Ras, which makes it stay active longer
Active Ras will activate serine-threonine kinase Raf, which activates
MEK, which activates MAP kinase
MAP kinase phosphorylates proteins to increase the transcription of transcription factors for proto-oncogenes myc and fos
Any mutations along the way can cause uncontrolled cell proliferation o Many transcription factors, like Myc and Fos, are proto-oncoproteins, which are the products of proto-oncogenes
MAP kinase can also phosphorylate and activate activator protein-1 (AP-1) transcription factor
AP-1 is made from the fos and jun proto-oncogenes
AP-1 targets genes for cell proliferation and progression through the cell cycle
Myc transcription factor has the same targets
Transcription factor C-myc is only made during the S phase of the cell cycle
Many tumors cause loss of regulation of this, and so c-myc is inappropriately expressed or overexpressed throughout the cell cycle, driving cells to continuously proliferate
Mutations to transcription factors increase the making of proteins that carry out processes for proliferation
Oncogenes of the cell cycle o The growth of human cells is activated by growth factors and hormones o These activators work through cyclins and cyclin-dependent kinases (CDKs), that control progression from one phase of the cell cycle to another o Page 317 – cell cycle o For quiescent (inactive) cells to proliferate, they must leave G
0
and enter G1 of the cell cycle o If the proper sequence of events happen in G1, the cell enters the S phase, and are committed to DNA replication and cell division o In G2, cells make commitments to mitotic division o CDKs are made constantly throughout the cell cycle, but need bound to a specific cyclin to be active
Different cyclins made at different times int eh cell cycle control each transition
(G1/S, S/G2, G2/M) o The activity of the cyclin-CDK complex is further regulated through phosphorylation, and through inhibitory proteins called cyclin-dependent kinase inhibitors (CKIs)
CKIs slow cell cycle progression by binding and inhibiting the cyclin-CDK complexes o CDKs are also activated by cyclin-activating kinases (CAKs), and inhibited by hyperphosphorylation kinases (adding a methyl silences) o The G1/S checkpoint- page 318
Since a cell commits to DNA replication and division once it enters the S phase, many regulatory proteins are involved in determining whether the cell is ready to pass this checkpoint
Regulator proteins include: o cdk4 and cdk6 – made throughout the cell cycle o cyclin D – made only after growth factor stimulation o retinoblastoma gene product (Rb) o E2 transcription factors (E2F)
In quiescent cells, Rb is complexed with E2F, which inhibits both of them
Upon growth factor stimulation, the cyclin Ds are induced, and bind to cdk4 and cdk6, converting them to active kinases
One of the targets of cyclin/CDK phosphorylation is the Rb protein
Phosphorylation releases Rb from E2F, and E2F is then free to activate transcription of genes required for entry into S
Rb is a tumor suppressor gene
Proteins induced by E2F include cyclin E and A, cdc25a (an activating phosphatase), and proteins that help initiate DNA synthesis
The making of cyclin E allows it to complex cdk2, forming another
active cyclin complex that retains activity into the S phase
One of the major jobs of the cyclin E1-cdk2 complex is hyperphosphorylation of the Rb protein, which keeps it inactive
Cyclin A also complexes with cdk2, and it inactivates E2F o This ensures that the signals are not present for too long
So each phase of the cell cycle activates the next through cyclin synthesis
The cyclins get removed by proteolysis o Progression through the cell cycle is opposed by CKIs
Two CKIs regulate cyclin/CDK in the G1 phase: Cip/Kip and INK4
Cip/Kip inhibit all cyclin-CDK complexes
INK4 specifically inhibits the cyclin D-cdk4/6 family
The regulation of making of different CKIs can be induced by DNA damage to the cell, and stop cell cycle progression until the damage can be repaired
If damage can’t be repaired, apoptosis happens
Like oncogenes, tumor suppressor genes also encode things involved in regulating cell proliferation
The normal job of tumor suppressor proteins is to inhibit proliferation, in response to certain signals, such as DNA damage
The signal is removed when the cell is completely ready to proliferate o So when you remove tumor suppressor genes, you take the “brakes” off of cell growth
Products of tumor suppressor genes often regulate pathways that are activated by protooncogenes
When both copies of the tumor suppressor gene are inactivated, it allows for cancer to develop
o Requires 2 mutations for cancer to happen o Different from proto-oncogenes, which only need one allele mutated oncogene
miRNA can also be a tumor suppressor
Tumor suppressor genes that directly regulate the cell cycle: o The retinoblastoma (rb) gene
The product, Rb, works in G1/S and regulates activation of E2F
If a person inherits a mutated rb allele, that person WILL develop retinoblastoma
This is because the probability is very high that the second rb allele will gain a mutation
This is called familial retinoblastoma
People who don’t inherit mutations in rb, but still get retinoblastoma, are said to have sporadic retinoblastoma, and acquire a mutation in each rb allele at some point in life o p53 – called the “guardian of the genome”
p53 – is a transcription factor that regulates the cell cycle and apoptosis
Loss of both p53 alleles happens in over half of tumors
p53 stops replication in cells that have DNA damage, and targets unrepaired cells for apoptosis
p53 levels will rise in response to mutagens, radiation, or UV light
p53 can act as a transcription factor to stimulate transcription of p21, a Cip/Kip
CKI
the p21 gene product inhibits cyclin-CDK complexes, and therefore
prevents inactivation of Rb and release of E2F proteins
So the cell is prevented from entering the S phase
p53 also stimulates transcription of DNA repair enzymes, like GADD45
if the DNA is successfully repaired, p53 will induce its own downregulation, by activating the mdm2 gene
if DNA repair is not successful, p53 activates genes for apoptosis, like Bax and
IGF-BP3
IGF-BP3 binds the receptor for IGF, which is thought to causes apoptosis by blocking antiapoptotic signals
Inheritance of a mutation in p53 causes Li-Fraumeni syndrome, which causes tumors
If p53 is mutated, the rate of mutations in cells will increase, cause there’s no p53 to check for DNA damage, initiate repair, or trigger apoptosis
So damaged DNA is replicated, and the likelihood of more mutations in that cell increases
Tumor suppressor genes that affect receptors and signal transduction:
o Tumor suppressor genes can encode receptors, parts of the signaling pathway, or transcription factors o Regulators of Ras
Ras proteins are involved in signal transduction for many hormones and growth factors, making Ras oncogenic
GTPase activating proteins (GAPs) interrupt Ras pathways
Neurofibromin- nervous system GAP made from tumor suppressor gene NF-1
Regulates Ras in neurons
So a signal to grow is transmitted in the cell, as long as Ras binds GTP
GAPs work by binding Ras and activating its GTPase, triggering GTP GDP, which inactivates Ras
No GAPs means Ras is always active and sending growth signals
Inherited mutation in NF-1 can cause neurofibromatosis, which causes many benign, but painful, tumors in the nervous system o Coreceptors patched and smoothened
Example of oncogenes and tumor suppressor genes working together
Smoothened is the proto-oncogene , and patched is the tumor suppressor gene
They control growth during embryogenesis
Patched receptor (tumor suppressor) inhibits smoothened receptor
Binding of a hedgehog ligand to patched will stop inhibition to smoothened, which can then transmit an activating signal to the nucleus to trigger gene transcription
If patched loses its function, smoothened can signal the cell to proliferate, even without any hedgehog signal
If smoothened has a gain-of-function mutation, it can signal without any hedgehog signal, even in the presence of patched
Inherited mutations to either smoothened or patched will lead to basal cell carcinoma
Tumor suppressor genes that affect cell adhesion: o Cadherin glycoproteins mediate calcium-dependent cell to cell adhesion o Cadherins form intercellular complexes that bind cells together o They’re anchored intracellularly to the cytoskeleton, by catenins , which bind actin o Loss of E-cadherin can allow cancer cells to detach and migrate in metastasis o People who inherit a mutation in E-cadherin have a good chance of developing gastric cancer
This mutation is called CDH1 o Catenins have two jobs: anchoring cadherins to the cytoskeleton, and being transcription factors
β-catenins can also bind APC, which causes degradation of β-catenin
When the appropriate signal inactivates APC, β-catenin levels increase, and it travels to the nucleus where it activates myc and cyclin D1 transcription, leading to cell proliferation
APC is a tumor suprressor gene, and if it’s inactivated, it can’t bind β-catenin to inhibit β-catenin and cell proliferation
Mutations in APC are found in most sporadic colon cancers
Inherited APC mutation leads to familial adenomatous polyposis (FAP), which is the most common hereditary colon cancer
Apoptosis is a pathway of programmed cell death to get rid of extra or unwanted cells
The cell self destructs
In apoptosis, the cell shrinks, the chromatin condenses, and the nucleus fragments o The cell membrane blebs, and the cell breaks up into membrane-enclosed vesicles called apoptotic bodies o Phosphatidlyserine is on the surface of the apoptic bodies, to be recognized by macrophage for phagocytosis
Apoptosis can protect from cancer, by destroying cells with irreparably damaged DNA, before they proliferate o Failure of apoptosis lets damaged cells survive
Apoptosis is divided into three phases: intiation, signal integration, and execution o It’s initiated by external signals that work through death receptors, like TNF, or lack of growth hormones o Apoptosis can also be initiated by intracellular events that effect mitochondrial integrity o In signal integration, the proapoptotic signals are balanced against antiapoptotic survival signals by pathways like Bcl-2 o The execution phase is carried out by caspases
Caspases- cysteine proteases that cleave peptide bonds next to an aspartate (C asp…) o They start as procaspases, which are inactive zymogen enzymes that need cleaved to be activated o Two types of caspases:
Initiator caspases – cleave other procaspases to activate them
Execution caspases – cleave proteins involved in maintaining cell integrity o Initiator caspases get activated through two major signaling pathways: the death receptor pathway and the mitochondrial integrity pathway o The initiator caspases activate the executioner caspases o Executioner caspases cleave protein kinases of cell adhesion, lamins of the nuclear membrane, actin, DNA repair enzymes, and inhibitor protein CAD
Cleaving CAD endonucelase (caspase-activated DNase) activates it to trigger breakdown of DNA
Destruction of the nuclear envelope then activates more endonucleases o The death receptor pathway of apoptosis (external signal):
Death receptors are a type of TNF-1 receptor
Includes Fas/CD95, TNF-receptor 1 (TNF-R1) and death receptor 3 (DR3)
They together form a trimer that binds TNF-1 or another death ligand
The activated TNF-receptor complex binds to procaspase 8 (or procaspase 10), which cleave each other to form active caspase 8 (or 10)
Caspases 8 and 10 are inititator caspases that activate execution caspases 3, 6, and 7
Caspase 3 cleaves a Bcl-2 protein called Bid, to cause it to activate the mitochondrial integrity pathway to apoptosis o Mitochondrial integrity pathway to apoptosis (internal signal):
Intracellular signals can also trigger apoptosis
Examples of signals are lack of growth factors, cell injury, release of some steroids, and increased intracellular Ca 2+
The signals lead to release of cytochrome c from the mitochondria
Cytochrome c is part of the electron transport chain just outside the inner mitochondrial membrane
Release of cytochrome c triggers apoptosis
In the cytoplasm, cytochrome c binds Apaf, and the complex binds initiator caspase 9, to form an apoptosome
The apoptosome activates execution caspases 3, 6, and 7 through cleavage o Bcl-2 proteins are decision makers that integrate pro-death and pro-life signals, to determine whether the cell should do apoptosis
Bcl-2’s can be either pro or anti-apoptosis
Bcl-2’s have 4 homologous regions called BH domains (BH1-BH4)
Antiapoptotic Bcl-2’s have all four BH domains
Proapoptotic channel forming Bcl-2’s have BH1-BH3, while BH3-only proapoptotic proteins have just BH3
Antioapoptotic Bcl-2’s inhibit apoptosis either by binding the outer mitochondrial membrane to inhibit channel forming proteins and inhibit cytochrome c release, or bind Apaf to prevent making of the apoptosome
Includes Bcl-2, Bcl-L, and Bcl-w
Channel forming proteins only differ from the antiapoptotic in that they lose the domain to bind Apaf
When they dimerize with BH3-only proteins in the outer mitochondrial membrane, they form an ion channel that promotes cytochrome c release
Ex: Bax is a channel forming protein
BH3-only proteins only have the domain to bind the channel forming proteins
When channel-forming proteins bind them, it activates the channel forming protein, and inhibits antiapoptotic Bcl-2’s
Ex: Bim, bid, and Bad are BH3 only’s
So when a BH3 protein like Bim is activated by a signal the cell got from something pro-death, it activates Bax to cause release of cytochrome c
At the same time Bid activates Bax, Bid also binds Bcl-2, preventing the
Bcl-2 from binding and inhibiting Apaf, allowing Apaf to bind cytochrome c to for the apoptosome
When Bcl-2 is mutated and oncogenic, it is overexpressed, which tips the
balance towards antiapoptosis, so cells with damaged DNA can’t undergo apoptosis
Bcl-2 also gets antitumor agents and drugs out of the tumor
Apoptosis should be triggered by things like withdrawal of growth factors, increased p53, repair enzymes, or release of TNF
Mutations to oncogenes can cause apoptosis-resistant cells o One way to do this is to activate growth factor dependent pathways to inhibit apoptosis
Ex: PDGF/Akt/Bad pathway
Nonphosphorylated BAD (BH3 only) acts like Bid to promote apoptosis
When PDGF binds its receptor, it activates PI-3 kinase, which phosphorylates and activates serine-threonine kinase Akt (protein kinase B)
Activated Akt causes phosphorylation of BH3-only Bad, inactivating it o A feature of cancerous transformation is the loss of dependence on growth factor for survival o The MAP kinase pathway also works in apoptosis and sends cell survival signals
MAP kinase activates a protein kinase called RSK, which also inhibits Bad o So Bad is where the PI-3 kinase/Akt , and MAP kinase pathways converge to signal survival o Gain-of-function mutations to genes that control these pathways, like ras (ras MAP kinase), create apoptosis-resistant cells
Several miRNAs regulate apoptotic factors o Ex: Bcl-2 is regulated by miRNA-15 and 16
Expression of them controls Bcl-2 levels in the cell
So a mutation to them will either increase Bcl-2, which promotes growth, or decrease Bcl-2, which promotes apoptosis
Loss of both is seen in leukemias, and increases Bcl-2 to cause growth o miRNA-21 regulates PDCD4, which blocks translation to cause apotosis
loss of miRNA21 causes apoptosis, and overexpression of miRNA21 inhibits apoptosis o increased miRNA-17 decreases PTEN levels to promote proliferation & inhibit apoptosis
Cancer takes a long time to develop because many genetic changes are needed to transform normal cells into malignant cells
A single change in one oncogene or tumor suppressor gene isn’t enough for transformation
Cells accumulate multiple mutations through clonal expansion
o When DNA damage happens in a proliferative cell, a population of cells with the mutation is produced, and expansion of this population increases the chances of a second mutation in a cell containing the first mutation o At this point, there may be enough mutations to increase the growth rate when there’s growth signals, followed by more mutations to cause autonomous growth independent of normal controls o Increased growth increases the chances of mutation
Since many different mutations can cause the same kind of cancer, it makes it hard to treat
Three RNA retroviruses can cause cancer to develop: HTLV-1, HIV, and hepatitis C
HTLV-1 causes adult T cell-leukemia o Uses Tax transcription factor to activate proto-oncogenes c-sis and c-fos
HIV causes immunosuppression, so decreased immune tumor regulation o HIV codes Tat transcription factor, which activates transcription of Il-6 and Il-10 growth
factor genes in infected T cells, causing non-Hodgkin lymphoma
Herediatary nonpolyposis colorectal cancer (HNPCC) and hereditary breast cancer, both result from inherited mutations with DNA repair
HNPCC is a mutation to DNA mismatch repair enzymes, allowing a mutation to survive
Familial breast cancer is a mutation to either BRCA1 or BRCA2, and makes up half of hereditary breast cancers o BRCA1 is activated by DNA damage to fix double-stranded breaks of DNA
Once BRCA1 is activated, it stops the cell cycle to allow time to repair DNA o BRCA2 is a tumor suppressor to fix DNA double strand breaks and recombo of chromatids in meiosis and mitosis
Needs to be active for cancer to develop
Chronic myelogenous leukemia (CML) – myeloid cells in bone marrow proliferate abnormally, causing a lot of nonlymphoid WBCs
Will have an abnormal Philadelphia chromosome, which increases the proliferation o Can check if chromosomes are abnormal with a karyotype, which arrests cells in metaphase of mitosis o Philadelphia mutation activates ABL proto-oncogene by binding it to the BCR, causing growth
Can show bleeding, signs like bruises and petechiae, from lack of platelets o The increased WBC proliferation crowds the megakaryocytes, so less platelets develop
Treat with a tyrosine kinase inhibitor
Burkitt lymphoma- general name for several B cell cancers, where proto-oncogene transcription factor c-myc is translocated to an area with a promoter for the Ig heavy chain, causing overexpression of cmyc
Gene for human epidermal growth factor receptor(ERBB2/HER2/NUE) is overexpressed in up to 1/5 of breast cancers
When HER2 is overexpressed, prognosis is bad because it increases risk for metastasis and resists therapy
TNM system is used to classify tumors:
T is stage of the tumor – higher the #, the worse the prognosis
N stands for # of lymph nodes that are affected by the tumor –↑the #, the worse the prognosis
M is metastasis – 0 means nope, and 1 means metastasis
Mutations that cause malignant melenomas include ras, p53, Cdk4, p16, and cadherin/β-catenin
Carcinoma– epithelial cell tumor (includes intestine lining, skin cells, airway lining)
Adenocarcinoma – if it grows in a glandlike pattern
Melanoma – carcinoma of the melanocytes o Most alarming sign of mole melanoma is color change