Cholesterol: The Good, the bad and the ugly
advertisement

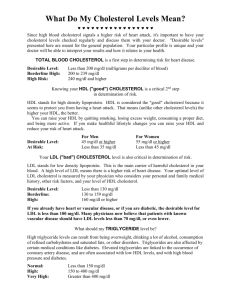
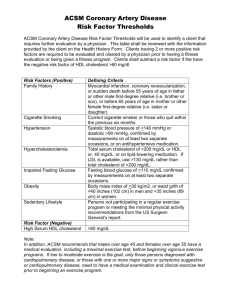
Cholesterol Outline • What is cholesterol? – Synthesis – Functions – Lipoproteins • Drugs to reduce cholesterol – – – – – Statins Bile-Acid Sequestrants Niacin (Nicotinic Acid) Fibric Acid Derivatives Ezetimibe and the Inhibition of Dietary Cholesterol What is cholesterol? • • • • Waxy, fat-like substance Steroid alcohol (sterol) Found in all cells of the body 75% of cholesterol is synthesized – 25% comes from diet Cholesterol synthesis • Synthesized primarily in the liver • Occurs in the cytoplasm and ER • The HMG-CoA Reductase reaction is ratelimiting – Highly regulated – Target of pharmaceutical intervention • Very complex process involving over 30 enzymes Functions of Cholesterol • • • • • Cell membranes Sex hormones Hormones released by the adrenal glands Production of bile acids Vitamin D Dangers of High Cholesterol Levels • Atherosclerosis – Increased coronary heart disease risk – Heart attack – Angina – Stroke Lipoproteins • • • • • Chylomicrons Very low density lipoproteins (VLDL) Intermediate-density lipoproteins (IDL) Low density lipoproteins (LDL) High density lipoproteins (HDL) Class % Protein % Cholesterol % Phospholipid % Triglyceride Chylomicrons <2 8 7 84 VLDL 10 22 18 50 IDL 18 29 22 31 LDL 25 50 21 8 HDL 33 30 29 4 Apolipoproteins • Six major classes – A, B, C, D, E and H Apolipoprotein Site of Synthesis Function(s) ApoA-I Liver, intestine Structural in HDL; reverse cholesterol transport ApoA-V Liver Modulates triglyceride incorporation into hepatic VLDL ApoB-100 Liver Structural protein of VLDL, IDL, LDL ApoB-48 Intestine Structural protein of chylomicrons ApoE Liver, brain, skin, gonads, spleen Structural in HDL; reverse cholesterol transport Chylomicron Triglyceride, LDL and HDL Metabolism Atherosclerosis Risk Factors • Diet • Medical conditions – Diabetes – Hypertension • • • • • Genetics Sex Age Smoking Inactivity & obesity Drugs Therapy of Hyperlipidemia 1. 2. 3. 4. 5. Statins Bile-Acid Sequestrants Niacin (Nicotinic Acid) Fibric Acid Derivatives Ezetimibe and the Inhibition of Dietary Cholesterol Statins • Competitive inhibitors of HMG-CoA reductase – Decreased cholesterol synthesis – Increased expression of the LDL receptor gene • Reduce LDL levels • Documented in reducing fatal and nonfatal CHD events, strokes, and total mortality – Adverse effects were similar in placebo and drug groups Statins Zocor Lipitor Crestor Effects on Triglycerides & Lipoprotein Levels • Decrease triglycerides in hypertriglyceridemic – 35-45% • Increase HDL-C – Normal patients: 5-10% – Low patients: 15-20% • Decrease LDL-C – 20-55% • Non-lipid lowering effects – Endothelial function (Enhances production of nitric oxide) – Anti-inflammatory – Reduce venous thromboembolic events • 43% • Adverse Effects – Hepatotoxicity • Elevated hepatic transaminase values • One case of liver failure per million person-years of use – Myopathy • One death per million prescriptions caused by rhabdomyolysis Bile-Acid Sequestrants • Highly positively charged – Bind negatively charged bile acids • Large size keeps them from being absorbed – Secreted in stool • Hepatic bile-acid synthesis increases – Hepatic cholesterol declines stimulating the production of LDL receptors and lowers LDL levels – Partially offset by the enhanced cholesterol synthesis caused by upregulation of HMG-CoA reductase • Combining these with a statin substantially increases their effect Bile-Acid Sequestrants Effects on Lipoprotein Levels & Adverse Effects • Dose dependent decrease in LDL-C – Normal dose: 12-18% reduction – Maximal dose (2x normal): Up to 25% reduction • GI side effects • HDL-C: Increase 4-5% • Combined with statins or niacin: 40-60% reduction • Adverse Effects – Generally safe – Hyperchloremic acidosis – Are not used in patients with hypertriglyceridemia • May increase triglycerides Niacin (Nicotinic Acid) • Inhibits the lipolysis by hormone-sensitive lipase – Reduces transport of free fatty acids to the liver – Decreases hepatic triglyceride synthesis • May inhibit diacylglycerol acyltransferase-2 – Rate-limiting in triglyceride synthesis – Reducing triglyceride synthesis reduces hepatic VLDL production • Raises HDL levels by decreasing the fractional clearance of apoA-I in HDL Effects on Lipoprotein Levels & Adverse Effects • Increases HDL: 30-40% • Lowers triglycerides by 35-45% • Reduces LDL: 20-30% • Half-life: 60 minutes – Requires 2-3 doses/day • Therapeutic Use – Hypertriglyceridemia and low HDL levels • Adverse Effects – – – – Flushing Dyspepsia Hepatotoxicity Hyperglycemia Fibric Acid Derivatives: PPAR Activators • Mechanism of action still remains unclear – Thought to interact with peroxisome proliferatoractivated receptors (PPARs) • Bind to PPARα – Increase LPL synthesis – Reduce expression of apoC-III – Stimulate apoA-I and apoA-II Fibric Acid Derivatives: PPAR Activators Effects on Lipoprotein Levels & Adverse Effects • Decreases triglycerides • Increases HDL-C • LDL-C can decrease, increase or be unchanged • Should not be used in patients with renal failure or hepatic dysfunction • Therapeutic Use – Type III hyperlipoproteinemia – Hypertriglyceridemia – Chylomicronemia syndrome • Adverse Effects – Rash – Hair loss – Fatigue Ezetimibe and the Inhibition of Dietary Cholesterol Uptake • Inhibits cholesterol absorption by enterocytes in the small intestine – 54% in humans • Inhibits the transport protein NPC1L1 Combination Therapy & Adverse Effects • Reduces LDL by 15-20% alone • Reduces LDL by 60% in combination with simvastatin • Should not be given with bile-acid sequestrants • Adverse Effects – Rare allergic reactions Videos • http://www.youtube.com/watch?v=9Tbo0GfDcg • Cholesterol • Atherosclerosis Mechanism of Action Statins • Inhibit an early and rate limiting step in cholesterol biosynthesis • Inhibiting hepatic cholesterol synthesis results in increased expression of the LDL receptor gene – Decreased free cholesterol causes membrane-bound SREBPs to be cleaved and translocated to the nucleus to bind the sterol responsive element of the LDL receptor gene. This enhancnes transcription and increases the synthesis of LDL receptors • It also reduces the degradation of LDL receptors Adverse Effects • Hepatotoxicity – Elevated hepatic transaminase values – One case of liver failure per million person-years of use • Myopathy – One death per million prescriptions caused by rhabdomyolysis Bile-Acid Sequestrants • One of the oldest hypolipidemic drugs • Safest – Not absorbed from the intestine • Used as a second agent if statins are not sufficient • Maximal dose can reduce LDL-C by up to 25% – Cause bloating and constipation so compliance is low Mechanism of Action • Inhibits the lipolysis by hormone-sensitive lipase – Reduces transport of free fatty acids to the liver – Decreases hepatic triglyceride synthesis • May inhibit diacylglycerol acyltransferase-2 – Rate-limiting in triglyceride synthesis – Reducing triglyceride synthesis reduces hepatic VLDL production • Raises HDL-C levels by decreasing the fractional clearance of apoA-I in HDL Mechanism of Action • Still remain unclear • Thought to interact with peroxisome proliferator-activated receptors (PPARs) – Bind to PPARα and stimulate fatty acid oxidation, increase LPL synthesis and reduce expression of apoC-III to reduce triglycerides – Bind to PPARα to stimulate apoA-I and apoA-II expression to increase HDL-C levels Mechanism of Action • Inhibits the transport protein NPC1L1 • Inhibits absorption by 54% in humans