BBS vs POMA in Determining Fall Risk in Elderly
advertisement

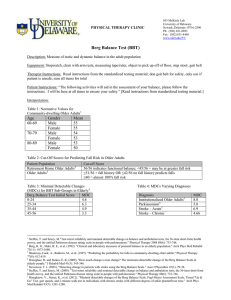
Berg Balance Scale vs Performance-Oriented Assessment of Mobility Problems (aka Tinetti): What the Evidence says about the two most widely used balance tests on elderly individuals in skilled nursing facilities Kelsey Shelton Virginia Commonwealth University - DPT What is a fall? Unintentional dislocation of the body to an inferior level to the initial position, with incapacity for correction in due time Two conditions must be satisfied for a fall to occur: o perturbation of balance o failure of the balance system to compensate and anticipate this perturbation Why are balance tests important? Due to aging processes, diseases, and inactivity, balance is often impaired among the elderly. The impairment can lead to dramatic consequences such as dependency in ADLs, admission to nursing homes, and falls/fractures. It is known that the ageing process provokes alterations in the systems responsible for balance, as well as altering the motor strategies, the reactive and anticipatory postural controll, and the limits of stability. The elderly who present damage in one or more systems responsible for balance develop a larger risk for suffering recurrent falls, making an assessment necessary. Balance impairment imparts a moderate increase on fall risk in community-dwelling older adults. o Impaired balance has been correlated with an increased risk for falls and a resulting increase in the mortality rate of elderly persons. Risk factors for fall include medical conditions (e.g., postural hypotension, anemia), medications, fear of falling, environmental factors (e.g., poor lighting, loose rugs), and problems with balance and mobility. Number of falls and gait impairments increases with advancing severity of dementia A reliable and valid clinical measure for balance abilities increases the physical therapist's ability to predict who is at risk for falls. The goal of screening is to identify people at risk for falling in the imminent future for further in-depth evaluation. Berg Balance Scale The 14-item Berg Balance Scale identifies and evaluates balance impairment in older adults. The items involve balance common to many functional tasks: o Sit to stand, stand to sit, stand and sit unsupported, transfer bed to chair, stand eyes closed, stand feet together, reach forward, pick up object from floor, SLS, tandem stance, look over shoulders, turn 360°, and alternate foot on step Does not examine the performance under altered environmental conditions, and none of the tasks demand reactive postural control The items are graded on a five-point ordinal scale, yielding a total of 56 points. Lower points are given for people in need of supervision or assistance, or if specific time or distance requirement is not met. The Berg needs very little equipment to administer. However, the 15 min needed to administer the test is longer than that needed by the other instruments. What does the evidence say about the Berg? The absolute reliability (MDC) showed that a change of 8 BBS points is required to reveal a genuine change in function among older people who are dependent in ADLs and living in residential care facilities. Intrarater reliability for the BBS was high Strong interrater reliability when raters are provided with written instructions and are allowed to ask questions prior to administering the balance test Relatively low sensitivity to change and limited responsiveness Low sensitivity - demonstrated poor sensitivity for predicting who would fall (53%) High specificity – (86-96%) to identify individuals in the nonfaller category o Improved sensitivity of the instrument is needed, particularly for those older adults scoring closer to the cutoff score of 45. Ceiling Effect – test is not able to distinguish outcomes of respondents above the highest level asked in the survey; large proportion of subjects have maximum scores o Ceiling effects on the BBS are lower than other measures particularly with mildly limited function subjects. o Limited items to challenge people with scores above the 45/56 range o Suggests that the measure may be more appropriate for use in communitydwelling older adults with lower levels of functioning. Cutoff for fall risk o Results support the test developers' use of 45 (out of 56) as a generalized cutoff score Adults who scored higher than the cutoff score on the test were less likely to fall than were those adults who scored below the cutoff score Decreased scores, did not predict increased frequency of falls o Previously recommended cutoff value of 45 was inadequate for identifying the majority of future fallers in community sample the optimal single cutoff value for any fall was 54, for multiple falls was 53, and for injurious falls was 54 o The high cutoff values required to optimize sensitivity indicates that balance impairment alone does not define increased fall risk and that falls are frequent among people with scores above 45 BBS has a better power for verifying falls suffered in the last year compared to the Balance Stability System BBS bas better discriminatory ability for identifying people sustaining recurrent or multiple falls than for identifying those who fall once or sustain an injury among community-dwelling elderly people o Elderly classified with fall risk on the BBS presented 2.5 (95%CI 1.08–5.78) more chance of identifying who had two falls or more over the last year The use of the BBS to identify people at high risk for falling is discouraged because it fails to identify the majority of these people. However, the predictability of this scale for multiple falls is superior to that for other types of falls It is a valid instrument used for evaluation of the effectiveness of interventions and for quantitative descriptions of function in clinical practice and research Tinetti Balance Test of the Performance-Oriented Assessment of Mobility Problems The total POMA scale (POMA-T) consists of a balance scale (POMA-B) and a gait scale (POMA-G). The POMA-B carries the subject through positions and changes in position, reflecting stability tasks that are related to daily activities. In the POMA-G, several qualitative aspects of locomotion pattern are examined. o Examples of balance components include standing and sitting balance, sit to stand, stand to sit, turn 360°, and nudge on sternum. Each item is scored on a 2- or 3-point scale, resulting in a maximum score of 28 on the POMA-T and maximum scores of 16 and 12 on the POMA-B and the POMA-G o Ordinal scale as either normal, adaptive, or abnormal o Gait portion rates seven gait characteristics as normal or abnormal The primary difference between the BBS and POMA-B items is the rating scale used. Also, the POMA-B assesses response to an external nudge while standing and the gait component primarily consists of observational gait analysis. Originally, the POMA-T was developed to predict falls in an institutionalized population. Later, the scale was used in various clinical contexts as a measure of mobility impairment and to study the effects of interventions. o Provides reimbursors with an objective picture of patients’ functional mobility and balance status Assesses many different aspects of balance and is simple and quick to administer After a few practice sessions, the observer can complete the assessment in less than 15 minutes Despite limited clinical experience, the students learned to perform the assessment with good reliability What does the evidence say? MDC – 5 points for it to be interpreted as a reliable change Interrater reliability is high but POMA-G tends to be lower Sensitivity was 70-85% and the specificity was 51-65% o Sensitivity and specificity: 95.5% for frequent fallers versus nonfallers o Supports the use of this test to screen elderly at risk of falling in order to include them in a preventive intervention The predictive validity was acceptable - for the POMA-B, the best predictive value was a score of ≤ 11 points with 70% sensitivity and 51% specificity. Ceiling Effect – More likely to reach than BBS o POMA has a lower threshold to attain the maximum score on each item and has a smaller number of items than BBS. o POMA-T showed a significantly lower ceiling effect than the POMA-B. Cut off for fall risk o A score of 36 or less identified 7 of 10 fallers with 70% sensitivity and 52% specificity. With this cut-off score, 53% of the individuals were screened positive and presented a two-fold risk of falling. o Individuals still fell with high scores on the Tinetti balance scale (37–40 out of 40). Demonstrated that the usefulness of the POMA scales for predicting future falls was severely limited o Good relative reliability and concurrent/discriminate validity o The POMA-G performed less well with regard to these properties. o POMA-T and the POMA-B should be preferred. o Responsiveness could only be assessed for POMA-T. The POMA-T is useful for demonstrating intervention effects. The POMA-T and its subscale POMA-B have adequate reliability and validity for assessing mobility in older adults. The POMA and Dementia o Application of the POMA in populations with moderate to severe dementia is hampered by feasibility problems. Contains dual tasks o Its implementation in clinical practice is not recommended. Conclusion Falls are primarily multifactorial in nature. A complete assessment of risk of falling also must examine the environment in which a person functions, not just a score achieved on any balance assessment. o Risk of falling may be substantially improved by examining their environment and how well they complete their ADLs Training of static and dynamic balance control is an important factor in rehabilitation for older people. There is a need for valid and reliable instruments for evaluating the effects of treatment. References 1. Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I., & Gayton, D. (1989). Measuring balance in the elderly: Preliminary development of an instrument. Physiotherapy Canada, 41, 304—311. 2. Cipriany-Dacko, L., Innerst, D., Jahannsen J., & Rude V. (1997). Interrater Reliability of the Tinetti Balance Scores in Novice and Experienced Physical Therapy Clinicians. Arch Phys Med Rehabil, 78, 1160-4. 3. Faber, M., Bosscher, R., & Wieringen, P. (2006). Clinimetric Properties of the PerformanceOriented Mobility Assessment. Phys Ther, 86(7), 944-954. 4. Littbrand, H., Malmqvist, L., Gustafson, Y., Conradsson, M., Lundin-Olsson, L., Lindelof, N., & Rosendahl, E. (2007). Berg Balance Scale: Intrarater Test-Retest Reliability Among Older People Dependent in Activities of Daily Living and Living in Residential Care Facilities. Phys Ther, 87,1155-1163. 5. Muir, S., Berg, K., Chesworth, B., & Speechley, M. (2008). Use of the Berg Balance Scale for Predicting Multiple Falls in Community-Dwelling Elderly People: A Prospective Study. Phys Ther, 88(4), 449-459. 6. Muir, S., Berg, K., Chesworth, B., Klar, N., & Speechley, M. (2010). Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: a systematic review and meta-analysis. 7. Journal of Clinical Epidemiology, 63, 389-405. 8. Pardasaney, P., Latham, N., Jette, A., Wagenaar, R., Ni, P., Slavin, M., & Bean, J. (2012). Sensitivity to Change and Responsiveness of Four Balance Measures for Community-Dwelling Older Adults. Phys Ther, 92(3), 388-397. 9. Pereira, V., Maia, R., & Silva, S. (2013). The functional assessment Berg Balance Scale is better capable of estimating fall risk in the elderly than the posturographic Balance Stability System. Arq Neuropsiquiatr, 71(1), 5-10. 10. Raîche, M., Hébert, R., Prince, F., & Corriveau, H. (2000). Screening older adults at risk of falling with the Tinetti balance scale. The Lancet, 356, 1001-2. 11. Sterke, C., Huisman, S., Beeck E., Looman, C., & Cammen, T. (2010). Is the Tinetti Performance Oriented Mobility Assessment (POMA) a feasible and valid predictor of short-term fall risk in nursing home residents with dementia? International Psychogeriatrics, 22(2), 254–263. 12. Tinetti, M. E. (1986). Performance oriented assessment of mobility problems in elderly patients. Journal of the American Geriatric Society, 34, 119-126. 13. Whitney, S., Poole, J., & Cass S. (1998). A review of balance instruments for older adults. The American Journal of Occupational Therapy, 52, 666-671.