Chronic Obstructive Pulmonary Disease
advertisement

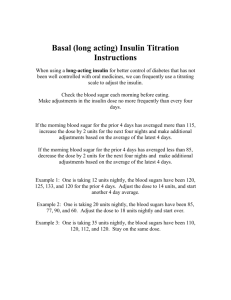
CASE PRESENTATION PATIENT’S PROFILE Name: Mr. X Date of Admission: 26/7/2009 Age: 72 years old Race: Malay Gender: Male Diagnosis: COAD, hypertension Weight: Cannot be assessed Height: Cannot be assessed Allergy: Unknown Chronic Obstructive Pulmonary Disease 1 progressive disease narrowing of the airways, leading to the shortness of breath and difficulty in breathing "Progressive" means the disease gets worse over time. 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition. COPD includes the terms chronic bronchitis (clinical term) and • condition with chronic or recurrent excessive mucus secretion into the bronchial tree with cough 1 emphysema (anatomic pathology) • enlargement of the air spaces distal to the terminal bronchioles, with destruction of their walls 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition. 2. http://www.buzzle.com/articles/pathophysiology-of-copd.html Causes • Cigarette smoking is the primary modifiable risk factor for the development of COPD. • Long-term exposure to other lung irritants, such as air pollution, chemical fumes, or dust, also may contribute to COPD. 5 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Pathophysiology 1 The most important processes causing lung damage are: Oxidative stress produced by the high concentrations of free radicals in tobacco smoke. Cytokine release due to inflammation as the body responds to irritant particles such as tobacco smoke in the airway. Tobacco smoke and free radicals impair the activity of antiprotease enzymes (such as alpha 1-antitrypsin) Protease enzymes damage the cells and tissue of lungs and other supportive tissues, 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Healthy vs COPD Symptoms 1 • • • • • 1. A cough (large amount of mucus) Chest tightness Shortness of breath Wheezing Low energy http://www.buzzle.com/articles/pathophysiology-of-copd.html Hypertension High blood pressure (HBP) or hypertension means high pressure (tension) in the arteries. Arteries are vessels that carry blood from the pumping heart to all the tissues and organs of the body.5 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Blood pressure is the force applied against the walls of the arteries as the heart pumps blood through the body. The pressure is determined by the force and amount of blood pumped and the size and flexibility of the arteries.1 1. http://www.healthline.com/sw/khs-understanding-asthma&usg Classification 1 1. Essential (primary) - no specific medical cause can be found to explain a patient's condition. 90-95% 2. Secondary. Secondary hypertension indicates that the high blood pressure is a result of another condition, such as kidney disease or tumours. 1. http://www.nlm.nih.gov/medlineplus/ency/imagepages/9124.htm Classification of BP for Adults 5 Classification SBP (mm Hg) DBP (mm Hg) Normal <120 And <80 Prehypertension 120-139 Or 80-89 Stage 1 hypertension 140-159 Or 90-99 Stage 2 hypertension ≥160 Or ≥100 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition High Blood - Pressure: The Silent Killer Hypertension may result either from a specific cause (secondary hypertension) or from an underlying pathophysiology mechanism of unknown etiology (primary or essential hypertension).1 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Secondary hypertension may cause by chronic kidney disease, Cushing’s syndrome, hyperthyroidism, hyperparathyroidism, primary alsosteronism, pregnancy, obstructive sleep apnea, and coarctation of the aorta. Some drugs that may increase BP: ~ Corticosteroids ~ Estrogens ~ Nonsteroidal antiinflammatory drugs (NSAIDs) ~ Amphetamines ~ Sibutramine ~ Cyclosporine ~ Tacrolimus ~ Erythropoietin ~ Venlafaxine 1 Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Multiple factors that contribute to the development of primary hypertension, including: Humoral abnormalities involving the reninangiotensin-aldosterone system, natriuretic hormone, or hyperinsulinemia Pathologic disturbance in the CNS, autonomic nerve fibers, adrenergic receptors, or baroreceptors 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Abnormalities in either the renal or tissue autoregulatory processes for sodium excretion, plasma volume, and arteriolar constriction. 1 Deficiency in the local synthesis of vasodilating substances in the vascular endothelium, such as prostacyclin, bradykinin, and nitric oxide, or increase in production of vasoconstricting substances such as angiotensin II and endothelin I. 1 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition High sodium intake and increased circulating natriuretic hormone would inhibit intracellular sodium transport, causing increased vascular reactivity and increased BP. 1 Increased intracellular concentration of calcium, leading to altered vascular smooth muscle function and increased peripheral vascular resistance. 1 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Diabetes mellitus is a group of metabolic disorders of fat, carbohydrate, and protein metabolism that results from the defects in insulin secretion, insulin sensitivity, or both. 1 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition There are two major classifications of diabetes mellitus: i) Type 1 DM ii) Type 2 DM They are differ in clinical presentation, onset, etiology, and progression of disease. 1 DIAGNOSIS OF DIABETES… Based on three criteria : i) Fasting plasma glucose ≥ 126mg/dL ii) A 2-hour value from a 75g oral glucose tolerance test ≥ 200mg/dL iii) Casual plasma glucose level of ≥ 200mg/dL with symptoms of diabetes 5 PATHOPHYSIOLOGY OF DM 1 Type 1 DM Generally develops in childhood or early adulthood and results from immune-mediated destruction of pancreatic β-cells, resulting in absolute deficiency of insulin. 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Type 2 DM 1 Characterized by the presence of both insulin resistance and relative insulin deficiency. Insulin resistance is manifested by increased lipolysis and free fatty acid production, increased hepatic glucose production and decreased skeletal muscle uptake of glucose. 1. Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, and Cecily V. Diporo, Pharmacotherapy Handbook, seventh edition Treatment of lower respiratory tract infections, skeletal infections, surgical prophylaxis and staphylococcal infections. Beta lactams antibiotic – Act by inhibiting the formation of peptidoglycan cross-links in the bacterial cell wall. Precaution: - hypersensitivity to b-lactam antibiotic - Renal impairment Adverse effect: - Neutropenia - Agranulocytosis - GI upsets - rash [1] Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. Interaction: A. Drug – Drug interaction - Co-admin of probenecid or disulfiram may result in higher cloxacillin concentration. - Chloramphenicol and tetracycline antagonise bactericidal effect of cloxacillin. B. Drug – Food interaction - delayed absorption in the presence of foods. Pharmacological Category: -Proton Pump Inhibitor Uses: -Treatment and maintenance of healing erosive esophagitis associated with GERD Precaution: -Relief of symptoms does not preclude the presence of a gastric malignancy. -Long term medication will caused biopsy-proven atrophic gastritis(especially caused by the bacterium Helicobacter pylori) [1] Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. Side Effect: -Chest pain, Headache(9%), Rash(2%), Diarrhea (6%), N/V/C (2%), back pain and Others. Storage: -Store the tablet at controlled room temperature of 20˚C to 25˚C. Mechanism of Action: -Suppresses gastric acid secretion by inhibiting the parietal cell H⁺ / K⁺ ATP pump. Dosage: -40 mg once daily for up 8 weeks (this is for who have erosive esophagitis associated with GERD. -20 mg once daily have been used in mild GERD treatment and maintenance therapy Administration (Oral): -Should be swallowed whole and do not crush or chew. -may be taken with or without food but the best if taken before breakfast (coz of PPI) Pharmacological Category: -Antilipemic agent -HMG-CoA Reductase Inhibitor Uses: -Treatment of dyslipidemias (to reduce elevations in total cholesterol, LDL-C and triglycerides -Primary prevention of cardiovascular disease. Precaution: -Secondary causes of hyperlipidemia should be ruled out prior to therapy. -Liver function must be monitored by periodic laboratory assessment if not may cause hepatic dysfunction. [1] Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. Side Effect: -Chest pain, Headache(17%), Rash(4%), Diarrhea (4%), N/C (3%), Insomnia and dizziness. Mechanism of Action: -Inhibitor of 3-hydroxy-3-methylgluryl coenzyme A (HMG-CoA) reductase . -Increase in the expression of LDL receptors on hepatocyte membranes and a stimulation of LDL catabolism. Dosage: -Initial: 10 to 20 mg once daily (for who have hypercholesterolemia) -then 40 mg once daily for patient >45% reduction in LDL-C Administration (Oral): -Should be swallowed whole and do not crush or chew. -may be taken with food -take the medicine on night Monitoring Parameters: -Lipid level after 2-4 weeks Uses: - constipation Precaution: -Do not take immediately before going to bed. -Avoid prolonged use. -Not be used for who has abdominal pain, nausea and vomiting. [2] British National Formulary Side Effect: -Rash, Abdominal pain, Nausea and Vomiting. Mechanism of Action: - Liquid Paraffin acts by softening and lubricating the faeces. The faeces can then move more easily through the bowel. By doing this it relieves constipation and reduces the pain of some conditions such as piles Dosage: -Take 15 ml for 3 times a day. Combivent nebulizer 8 hourly Combivent- Salbutamol and ipratropium Salbutamol- Act on β2 receptors β2 receptors stimulation activate adenyl cyclase increase in intracellular cyclic adenosine monophosphate (cAMP) relax bronchial smooth muscle Ipratropium- competitively inhibit cholinergic receptor in bronchial smooth muscle block acetylcholine reduce cyclic guanosine monophosphate (cGMP) relax brochial smooth muscle Precaution: immediate hypersensitivity reactions may occur after administration, as demonstrated by rare cases of urticaria, angioedema, rash, bronchospasm. Drug-drug interaction: # Ipratropium-increase toxicity with anticholinergic or drug with anticholinergic effects (eg: atropine, TCA, antipsychotic drug). # Salbutamol- refer to MDI salbutamol Adverse drug reaction: (Ipratropium) # Glaucoma # Hypersensitivity reaction # Urinary retention # Blurred vision Metered dose inhaler salbutamol 2 puff + prn Bronchodilator Short acting selective β2 - adrenergic agonist Act on β2 receptors β2 receptors stimulation activate adenyl cyclase increase in intracellular cyclic adenosine monophosphate (cAMP) bronchial smooth muscle relaxation Precaution: # hypertension # cardiac disorders (eg: arrhythmia, CHF) # diabetes # elderly patients. Drug-drug interaction: # salbutamol + nonpotassium sparing diuretics (eg: furosemide) hypokalemia # α- blocker, β-blocker decrease effect of sulbutamol Drug-food interaction: # Avoid or limit caffeine- may cause CNS stimulation Adverse drug reaction: # CNS stimulation # Arrhythmia # Seizure # Hyperglycemia # Hypokalemia Step For Using Metered Dose Inhaler Take off the cap and shake the inhaler. Breathe out all the way to empty the lungs as much as possible. Hold the inhaler 1 - 2 inches in front of your mouth (about the width of 2 fingers). Start breathing in slowly through your mouth, and then press down on the inhaler one time. (If you use a spacer, first press down on the inhaler. Within 5 seconds, begin to breathe in slowly.) Keep breathing in slowly, as deeply as you can. Hold your breath as you count to 10 slowly, if you can. This lets the medicine reach deep into your lungs. Wait about 1 minute between puffs for inhaled quick-relief medicine (beta-agonists). There is no need to wait between puffs for other medicines. Rinse your mouth - help reduce unwanted side effects. Tablet prednisolone 20mg OD Systemic corticosteroid Antiinflammatory mechanism; beneficial effect- reduction in capillary permeability to decrease mucus, inhibition of release of proteolytic enzymes from leukocytes, and inhibition of prostaglandin. Precaution: # Use with caution in patients with thyroid disease, hepatic impaired, renal impairment, cardiovascular disease, diabetes, patients at risk of osteoporosis, patients at risk of seizure, patients at risk of GI disease (peptic ulcer). Drug-drug interaction: # CCB (nondihydropyridine), azole antifungal, macrolide- may increase the serum level of prednisolone # Prednisolone may increase the hypokalemia effect of potassium wasting diuretic (loop or diuretic) # Concurrent use of NSAIDs and salicylate with corticosteroid- may increase GI adverse effect. # Antacids may reduce absorption of corticosteroid- separate administration by 2 hours. # Prednisolone may cause reduction in warfarin effect. Drug-food interaction: #Avoid ethanol- may increase gastric mucosal irritation. # Prednisolone interfere with absorption of calcium. # Limit caffeine. Adverse drug reaction: # Increase appetite # Weight gain # Peptic ulcer # Hypokalemia # Convulsion # Diabetes mellitus ACTRAPID HM PENFILL HUMAN INSULIN SOLUTION FOR INJECTION WHAT ARE THE DIFFERENCES BETWEEN THE TYPES OF INSULIN? Types of Insulin Names of Insulin How Fast They Start Humalog/Lispro Rapid Acting Novolog/Aspart 5 - 15 minutes When the Action Peaks How Long They Last 30 - 90 minutes 1 - 3 hours 3 - 5 hours Short Acting Regular 1/2 - 1 hour 2 - 4 hours 6 - 8 hours Intermediate NPH 1 - 2 hours 6 - 10 hours 10 - 16 hours 1 - 2 hours No peak action 24 - 36 hours Lantus/Glargine Long Acting Levemir/Detemir COMPOSITION Active substance: Human insulin, ( recombinant DNA produced in Saccharomyces cerevisiae) 1 IU is corresponds to 0.035mg of anhydrous human insulin. INDICATIONS Treatment of diabetes mellitus. Initial stabilization of diabetes especially in diabetes emergencies. MODE OF ACTION The blood glucose lowering effect of insulin is due to : Facilitated uptake of glucose following binding of insulin to receptors on muscle and fat cells. Simultaneous inhibition of glucose output from the liver. An average action profile after subcutaneous injections indicates: Onset: within half hour Maximum: between 1 and 3 hours Duration: approximately 8 hours. DOSAGE Dosage is individual and determine by the doctor in accordance to the patient requirement. the average doses is in between 0.5 to 1.0UI/kg. This patient need to take 16IU for morning, 14 IU during afternoon and night. in geriatric patients, the primary aim of treatment is to relief symptoms and to avoid hypoglycemic events. HOW TO ADMINISTER ACTRAPID? 1. Actrapid HM is usually injected subcutaneously (SC) onto the abdominal region, thigh,gluteal region and deltoid region. 2. SC injection into the abdominal wall ensures a faster absorption than other injection sites. 3. Injection into a lifted skin fold minimises the risk of intramuscular injection. 4. After the injection, the needle should remain under the skin for at least 6 seconds. 5. Keep the push button fully depressed until after the needle has been withdrawn from the skin. 6. Injection sites should be rotated within an anatomic region in order to avoid lipodystrophy. The above pictures shows lipodystrophy that occur at the insulin injection sites. 7. The insulin penfill should be used by one person only to avoid risk of passing diseases. 8. An injection should be followed within 30 minutes by a meal or snack containing carbohydrates. UNDESIREBLE EFFECTS Hypoglycemia is a frequently occurring in insulin therapy. The symptoms are include: cold sweat, cool pale skin, nervousness, confusion, difficulty in concentration, headache, nausea and palpitation. severe hypoglycemia may lead to unconsciousness and may result temporary or permanent impairment of the brain function and even death. Local hypersensitivity reaction may occur at the injection sites during treatment with insulin. OVERDOSE Mild hypoglycemic episodes can be treated by oral administration of glucose or sugary products. It is recommended for diabetic patients constantly caries some sugar lumps, sweets, or sugary fruit juices. For severe hypoglycemic episodes, patients can be treated by IM or SC injection of glucagon (0.1 to 1.0mg) or glucose given by IV injection by medical professionals. STORAGE Actrapid HM Penfill which is not in use should be stored at 2⁰C to 8 ⁰C in a refrigerator. If in use, should not kept in the refrigerator, keep in room temperature for up to 4 weeks. Keep protected from light. Keep out from the reach of children. Remove the needle after each injection. Keep out from exposed to heat or direct sunlight and should never be frozen. Insulin product which has been frozen must not be used. Never use insulin after the expiry date or the solution is not clear. A. FELODIPINE 15 mg OD Indication- lowering blood pressure -To be taken once daily without food. -Calcium channel blocker- act by inhibits calcium ion from entering the slow channel s or select voltage sensitive areas of vascular smooth muscle and myocardium during depolarization causing relaxation of coronary vascular smooth muscle and coronary vasodilation. Precaution : 1. peripheral edema is the most common SE occurs w/in 2-3 weeks of starting therapy. 2. May cause hypotension with reflex tachycardia resulting in MI Common adverse effect: - headache - peripheral edema - tachycardia - flushing Interaction: A. Drug – Drug interaction - Cimitidine, erythromycin,itroconazole and ketoconazole cause increase plasma concentratin of felodipine. - Phenytoin, carbamazepine, rifampicin and barbiturate cause decrease plasma concentration of felodipine. B. Drug – Food interaction - Ethanol will increase felodipine absorption, greater hypotensive effect. - Grapefruit juice increase effect of felodipine lead to severe hypotension if concurrent use. B. PRAZOSINE 4 mg tds Indication: for treatment of hypertension. -Starting dose is best taken with dinner, at least 2-3 hr before retiring. Maintenance doses may be taken with or without meals. -Is alpha adrenergic blocker- act as antagonist of α adrenergic receptors which lower blood pressure by relaxing blood vessels. Precaution: - First dose may cause orthostatic hypotension and syncope associated with the body's poor ability to control blood pressure without active alpha-adrenergic receptors. Patients on prazosin should be told not to stand up too quickly, since their poor baroreflex may cause them to faint as all their blood rushes to their feet. Common side effect: - orthostatic hypotension - syncope - priapism Interaction: Drug –Drug interaction - May increase plasma concentrations of digoxin - Risk of 1st dose hypotension is increased in patients receiving βblockers or calcium-channel blockers. C. FUROSEMIDE 40 mg OD Diuresis agent used for treatment of hypertension. Is a loop diureticFurosemide inhibits reabsorption of Na and chloride mainly in the medullary portion of the ascending Loop of Henle. Excretion of potassium and ammonia is also increased while uric acid excretion is reduced. It increases plasma-renin levels and secondary hyperaldosteronism may result. Furosemide reduces BP in hypertensives as well as in normotensives. It also reduces pulmonary oedema before diuresis has set in. Precaution: - may cause prostate enlargement - may lower serum calcium and magnesium level Adverse effect: - abdominal discomfort - orthostatic hypotension - dizziness and headache - git disturbances Interaction: Drug – Drug interaction - it enhances toxicity of aminoglycoside, cephalosporine, salicyclates and lithium. - decreased effect by probenecid - orthostatic hypotension increased if used together with alcohol, barbiturate, and narcotic. DRUG RELATED PROBLEM 1. Combivent Nebulizer [1,2] beta-agonist induced hypokalaemia beta-agonist induced hypokalaemia may be increased by concomitant treatment with prednisolone and diuretic (Lasix). Slow K tablet (2 tablets 600mg per day) can be given to prevent hypokalaemia [1] Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. [2] MIMS Malaysia 113th edition 2008 Changes In dosage regimen Drug Start- stop date Combivent Nebulizer 8 hourly 9/8-17/8 Combivent Nebulizer 2 hourly for 4 times then 4 hourly for 4 times 17/8-19/8 Combivent Nebulizer 4 hourly 19/8- 21/8 Combivent Nebulizer 8 hourly 21/8- Continue Use Regimen of Combivent Nebulizer is changed from 8 hourly to 2 hourly for 4 times then 4 hourly for 4 times may due to the frequent bronchospasms of the patient. After 2 days (19/8), the regimen changes to 4 hourly and subsequent 8 hourly at 21/8 may due to the conditions of patient more controlled and less frequent attacks. 2. PREDNISOLONE1 Increase the risk of hypokalaemia with diuretic (Lasix) and β-agonists (Salbutamol) Prednisolone interfere with calcium absorption and lower bone density lead to high risk of osteoporosis if use for long term Calcium level and bone density of patients need to monitor frequently and biphosphonates (Alendronate 5mg daily[3] ) can be used. Risk of peptic ulcer in patient Calcium channel blocker may increase serum level of Prednisolone Need to ensure lowest effective dose is used in elderly [1]Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. [3] Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer and Cindy W. Hamilton, 2006. Pharmacotherapy Handbook, 7th edition, The McGraw-Hill Companies, Inc Changes In dosage regimen Drug Start- stop date Prednisolone 20mg, OD 16/8-17/8 Hydrocortisone 200mg, IV, QID 17/8 Hydrocortisone 100mg, IV,TDS 17/8-20/8 Prednisolone 30mg, OD 20/8-23/8 Prednisolone 20mg, OD 23/8-Continue Use Prednisolone has been changed to hydrocortisone IV 200mg may due to the severe inflammation of respiratory tract. The hydrocortisone dose is decreased to 100mg and later changed to oral prednisolone 30mg when the inflammation is more controlled. The patient continues to take Prednisolone 20mg for antiinflammation in respiratory tract. 3. S/C ACTRAPID 1 Decrease hypoglycemic effect with corticosteroid & furosemide Insulin decrease potassium serum concentration lead to hypokalaemia Dosage adjustment: Drug Start- stop date S/C Actrapid14IU, tds 4/8-6/8 S/C Actrapid 8IU, tds 9/8-12/8 S/C Actrapid 10IU, tds 12/8-Discontinue S/C Actrapid 18/16/16IU, tds 13/8-17/8 S/C Actrapid 14IU, tds 16/8-18/8 S/C Actrapid 14/12/12, tds 19/8-20/8 S/C Actrapid 16/14/14, tds 20/8- Continue Use [1]Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. The dose of Actrapid is adjusted from time to time. Possibilities: 1. 2. 3. Dosing adjustment is made based on patient’s glucose level. Concomitant administration of Frusemide. Frusemide will decrease glucose tolerance and require increase dose of insulin Corticosteroid 4. CLOXACILLIN[2] Cloxacillin is started since 2/8 and discontinued on 11/8. It is started again on 17/8 and is still on-going(until 23/8). Prolonged use may result in fungal or bacterial superinfection, including diarrhea and pseudomembranous colitis Risk of blood disorder and GI disturbances References: 1. Charles F.Lacy et.al, 2008. Drug Information Handbook with International Trade Names Index, 17th edition, Lexi-Comp Inc. 2. MIMS Malaysia 113th edition 2008 LASIX (FUROSEMIDE) Patient at risk of hypokalaemia [1] → Monitor potassium level daily → Slow-K (2 tablets [6oo mg/tab] per day) Frusemide level might be decreased if taken with food Glucose tolerance may be decreased – need dosing adjustment of insulin Charles F. Lacy et al. Drug information handbook with international trade name index, 17th edition, Lexi-Comp Inc., 2008-2009. For patient with concurrent hypertension and diabetes: It is recommended to used thiazide group of diuretic [2] Eg: Hydrochlorothiazide (25 – 200 mg daily) However, the prednisolone may enhance the K-depleting effect Slow K Joseph T. Dipiro et al. Pharmacotherapy. A pathophysiologic Approach, Seventh Edition, The McGraw-Hill Companies, Inc., Singapura, 2008. FELODIPINE Dose is high (15 mg ) For elderly: recommended starting dose 2.5 mg daily Increase by 5 mg daily in 2 weeks interval Usual dose: 2.5 – 10 mg Side effects due to vasodilatation (edema, flushing, dizziness and headache) occur more frequently It is suggested to use non-dihydropyridine group: verapamil and diltiazem The dose is changed from 10 mg 15 mg 20 mg 15 mg. The increment of dose: hypertension condition is not well-controlled. It is suggested to change drug: ARB (Losartan 50 mg daily) After that, the dose is decreased. This may be due to the condition is under control by the synergistic effect of other antihypertensive drugs. Decrement of dose can also reduce the incident and severity of possible side effects PRAZOSIN The dose is changing from 1 mg tds 2 mg tds 3 mg tds 4 mg tds This maybe due to the hypertension is not well-controlled Synergistic effect of antihypertensive effect with furosemide and felodipine Combination of 3 drugs cause postural hypotension, dizziness and lightheadedness Reduced to 1 mg or 2 mg three times a day once the condition is controlled [3] Prazocin www.Rxlist.com Prazosin is the best of choice if the patient has concurrent hypertension and BPH. Monitor blood pressure closely. Desired BP: < 130/80 mmHg PANTOPRAZOLE Maybe used for prophylaxis of peptic ulcer caused by prednisolone. [4] Dose: 20 mg daily(currently 40 mg BD) Normal dose for peptic ulcer treatment : 40 mg once daily 40 mg BD is used for Zollinger-Ellison syndrome MIMS, 113th Edition, 2008. Therapy is for 2 - 4weeks Long-term therapy may lead to bacterial overgrowth in the GI tract Potential of bronchitis, cough and dyspnoea happen Alternative: omeprazole LIPITOR Pantoprazole may increase the effects of Lipitor Potential respiratory (bronchitis) adverse effect Alternatives: fibric acid (eg. gemfibrozil) and niacin It may cause constipation (up to 3%) May lead to another drug use: liquid paraffin SUMMARY REFERENCE: [1] Barbara G. Wells, Joseph T. Dipiro, Terry L. Schwinghammer, Cecily V. Dipiro, Pharmacotherapy Handbook, 7th Edition, McGrawHill 2009. RECOMMENDATION LOSARTAN Dose: Usual starting dose 50mg OD (50mg/tab), LOSARTAN + HYDROCHLOROTHIAZIDE Dose: 50mg/12.5mg OD. If after 3 weeks 100mg/25mg (max effect after 3 weeks) CCB (Verapamil 40mg/tab) Dose: 240-480mg in 2-3 divided dose (HUSM Formulary) REFERENCE: [2] www.kck.usm.my/husm/pharmacy/formulary Drug- drug interaction PRESCRIPTION CASCADE DRUG 1 ADR DRUG 2 Other medication related problems ROLE OF PHARMACISTS By: GROUP F NASYARUDDIN BIN SIMALI OOI KEAN LOON SHAHMANAZREY CHE DAN CHONG HUI SAN CORINNE CHEW SHU LING LAI MEI YEN NOOR’IZAYU ABD RAZAK NOR HIDAYAH BINTI RUZALLE TEH WEN YEN