PowerPoint - Honors Human Physiology
advertisement

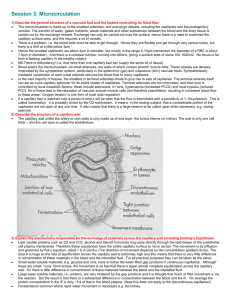
September 30, 2015 Cardiovascular 6 Special Circulations: Cardiac Muscle • The coronary arteries branch directly from the aorta, and provide the perfusion of the heart. Although blood actually is pumped through the heart, only ~ 100 µm of the inner endocardial surface can obtain significant amounts of nutrition directly from the blood supply in the cardiac chambers. Special Circulations: Cardiac Muscle • Blood flow through the coronary capillaries during systole and diastole is different than in most other tissues of the body. The blood flow to the ventricles falls during systole, and increases during diastole. During ventricular contraction, blood flow through the capillaries is obstructed by compression of the vessels. Thus, blood flow increases during diastole when the muscle around the vessels relaxes. Special Circulations: Brain The cerebral circulation is almost completely insensitive to neural and hormonal influences that produce vasoconstriction elsewhere in the body. By far the predominant factor that controls blood flow through the cerebral circulation is paracrine release. In particular, carbon dioxide has a strong vasodilation effect on the cerebral vessels. Special Circulations: Skeletal Muscle Control of blood flow to skeletal muscle is in many respects similar to that in the heart. Paracrine factors have strong influences, and vasodilation is induced by the release of epinephrine from the adrenal gland. A major difference between the two circulations is that skeletal muscle arterioles are richly innervated by sympathetic vasoconstrictor fibers, and are major resistance vessels to contribute to total peripheral resistance. Because skeletal muscle mass is so large, vasodilation of muscle vessels would greatly diminish total peripheral resistance unless vasoconstriction occurs in other vascular beds. It is thus necessary that the central nervous system provides control of blood flow through skeletal muscle. Special Circulations: Skin The skin requires little blood flow to meet its metabolic needs. However, blood flow to the skin increases tremendously when the body is overheated. Many arteriovenous shunts exist in the skin, and these are innervated by sympathetic efferents. When temperature is high, the efferents stop firing, and more blood travels into the skin for cooling. When temperature is low, the opposite occurs. Bradykinin release during sweating also leads to vasodilation of vascular smooth muscle in the skin, allowing more blood to be cooled. Where is Fluid Located in the Body? Plasma Interstitial fluid Intracellular fluid (~ 3 L) (~12 L) (~25 L) Anatomy of a Capillary • Capillaries are composed of a single layer of endothelial cells and a basement membrane. • Small intercellular clefts typically separate the endothelial cells. • Capillaries are often associated with elongated, highly branched cells that form a meshlike layer between the endothelium and interstitial fluid. These cells are called pericytes. The pericytes contribute to restricting capillary permeability. Movement of Materials Across Capillaries • Exchange of materials through capillaries usually occurs through diffusion. • Small and uncharged and lipid-soluble molecules (including O2 and CO2) have no problem passing through the capillary wall. • Larger and charged molecules may pass through the intercellular clefts or via vesicular transport. • Some capillaries have receptors for particular proteins; once the protein binds it is carried across the membrane via a process called transcytosis. Movement of Materials Across Capillaries • Water crosses the capillary through specialized water channels (aquaporins) in the endothelial cell membrane. Movement of Materials Across Capillaries • In general, large molecules have a very difficult time escaping from capillaries, unless they are lipophylic. Movement of Materials Across Capillaries • Large molecules and even whole cells can enter and leave the circulation when intercellular clefts are large. Osmosis • Osmosis is the diffusion of water molecules across a semi-permeable membrane from a region of high concentration to a region of low concentration until a state of dynamic equilibrium is reached. • A molecule is osmotically active if it causes osmosis to occur. Osmolarity • A measure of the absolute concentration of osmotically active particles. • A solution of 1 mole/L of non-dissociable solute is equivalent to 1 osmole/L (1 Osm). • Normal osmolarity of body fluids is about 300 mOsm. • The osmotic pressure of a 1 Osm solution is 22.4 Atm, or 22.4 x 760 = 17,024 mmHg. Thus a 300 mOsm solution has an osmotic pressure equivalent of 17,024 x 0.3 = 5,107 mmHg. Oncotic Pressure • Defined as the osmotic pressure generated by protein. • Protein is the only molecular species for which there is a significant concentration difference between the plasma and interstitial fluid (higher in plasma). • Hence, differences in protein concentration provide the only osmotic driving force at the capillary level. • The plasma protein concentration is about 7 gm/100 cc plasma (7 gm%). The osmotic pressure generated by this protein is known as the oncotic pressure and is in the range of 25-28 mmHg. Hydrostatic Pressure • Another major force is at play in capillaries: hydrostatic pressure, which is due to the pressure in the blood imparted primarily by the contraction of the ventricle. • The hydrostatic pressure is higher in the capillary than in the interstitial fluid, and tends to force fluid OUT of the capillary. • The balance between oncotic pressure and hydrostatic pressure across the capillary will determine whether there is a net gain or loss of fluid across the vessel. This balance can be expressed quantitatively via: Starling’s equation. Starling Equation Jv = Kf ([Pc—Pi] — σ [πc—πi]) Net fluid movement Oncotic Pressure difference Filtration coefficient Hydrostatic pressure difference Reflection coefficient Starling Equation Jv = Kf ([Pc—Pi] — σ [πc—πi]) If Jv is positive, fluid leaves the capillary (filtration) If Jv is negative, fluid enters the capillary (absorption) Starling Equation Jv = Kf ([Pc—Pi] — σ [πc—πi]) • • • The filtration coefficient ( Kf ) is the constant of proportionality. A high Kf value indicates a highly water permeable capillary. A low value indicates a low capillary permeability. The filtration coefficient is the product of two components: capillary surface area and capillary hydraulic conductance (the number of aquaporin channels present). Starling Equation Jv = Kf ([Pc—Pi] — σ [πc—πi]) • • • • The reflection coefficient (σ) is often thought of as a correction factor. Some smaller proteins can leak across the capillary membrane through the intercellular clefts, which must be accounted for as it diminishes the driving force. The reflection coefficient is used to ‘correct for’ the ineffectiveness of some of the oncotic pressure gradient. It can have a value from 0 up to 1. Non-fenestrated vessels have a reflection coefficient close to 1, whereas the value is lower for fenestrated capillaries. Starling Equation Jv = KXf ([Pc—Pi] — σ X [πc—πi]) Kf and σ are fixed for most (but not all) capillaries. Thus, changes in Jv are only due to changes in the oncotic pressure and changes in the hydrostatic pressure across the vessel. Jv ≈ ([Pc—Pi] — [πc—πi]) Starling Equation Arteriole Capillary Venule Filtration Jv ≈ ([Pc—Pi] — [πc—πi]) 25 -3 25 5 Jv ≈ ([25 J— 8 — [ 25 — 5]) v ≈-3] Starling Equation Arteriole Venule Absorption Jv ≈ ([Pc—Pi] — [πc—πi]) 25 -3 10 25 2 Jv ≈ -7 5 Arteriole Venule Filtration Jv ≈ 8 Absorption Jv ≈ -7 The net filtration pressure is 1 mmHg. In general, we tend to lose 2-4 liters of fluid per day into the interstitial space due to the 2 filtration-absorption imbalance. Increased Venous Pressure Arteriole Venule J ≈ ([60 — (-3)] — [25 — 5]) v J ≈ ([40 — (-3)] — [25 — 5]) v J ≈ v J ≈ v 43 23 Filtration occurs across the entirety of the capillary; considerable fluid is lost into the interstitial space! 2 Hypoproteinemia Arteriole Venule J ≈ ([25 — (-3)] — [11— 2]) v J ≈ ([10 — (-3)] — [11— 2]) v J ≈ v J ≈ v 19 4 Filtration occurs across the entirety of the capillary; considerable fluid is lost into the interstitial space! 2 Increased Capillary Permeability Assume 40% increase in Kf Arteriole J ≈ 1.4 * ([25 — (-3)] — [25 — 5]) v J ≈ v 11.2 Venule J ≈ 1.4 *([10 — (-3)] — [25 — 5]) v J ≈ v -9.8 The net filtration pressure increases to 1.4; more loss of fluid into the interstitial space! 2 Hemorrhage Arteriole J ≈ ([15— (-3)] — [25 — 5]) v J ≈ -2 v Venule J ≈ ([5— (-3)] — [25 — 5]) v J ≈ -12 v Consequently, fluid is absorbed from the interstitial space into the intravascular compartment. Over time, this movement of fluid will serve to increase blood volume, thereby increasing blood pressure. 2 Test your understanding! The main determinants of mean capillary hydrostatic pressure are: a) b) c) d) e) Arterial pressure and venous pressure Arterial pressure and capillary permeability Pre-capillary resistance and capillary permeability Pre-capillary resistance and venous pressure Venous pressure and capillary permeability Question for Discussion Do changes in hematocrit posture affect affect plasma fluid movement oncotic pressure? across capillaries? The Lymphatic System Because filtration typically exceeds absorption in capillaries, there is a net loss of fluid (about 2-3 L/day) into the interstitial space. It is the job of the lymphatic system to collect this fluid and return it to the circulation. Other functions include picking-up materials in the liver and intestine, and serving as a filter to capture and destroy foreign pathogens. Lymphatic System In addition to the capillaries of the cardiovascular system, an extensive collection of lymph capillaries exists in the body. These lymph capillaries are close to “real” capillaries in all tissues of the body, except the central nervous system and kidney. Lymphatic System The thin walls of the lymph capillaries are held open by attachments to surrounding cells. Adjacent cells overlap in the lymph capillaries, providing valves that allow fluid and large molecules in the interstitial space to enter (but not to leave). Lymphatic System The lymph capillaries coalesce to form larger “collecting” lymphatics, the largest of which is the thoracic duct, which empties fluid from the entire lower body back into the cardiovascular system. The lymphatic system makes connections with the cardiovascular system near the collarbones, near the junction between the subclavian veins and the internal jugular veins. Lymphatic System The major force driving fluid to enter the lymph capillaries is interstitial fluid pressure (once the fluid is inside the lymphatic system, it is called lymph). The higher the pressure in the interstitial fluid, the more fluid will enter the lymph capillaries. This arrangement is convenient, as it helps to assure that all the fluid leaving the cardiovascular system is returned. Fluid flow into lymph capillaries will increase under any of the following conditions that raise interstitial fluid pressure: o Capillary pressure is elevated (which enhances filtration) o Plasma colloid osmotic pressure is reduced (which retards absorption) o Interstitial fluid protein is increased (which retards absorption) o Capillary permeability is increased Lymphatic System No pump moves fluid in the lymphatic system. The major force inducing lymph movement comes from compression of lymph vessels during muscular contraction (if a limb is immobilized, you have to elevate it because muscular contraction is not sufficient to induce lymph flow). Lymphatic System Edema results when interstitial fluid builds up in an area. This often happens after injury because of increases in the amount of protein in the interstitial space (which pulls fluid from the cardiovascular system). Although increased interstitial pressure usually leads to increased lymphatic drainage, this doesn’t happen after some injuries because lymph capillaries are also damaged. Furthermore, there are limits to the rate of fluid flow into the lymphatic system. Another factor that can lead to edema is blockage of the lymphatic system. In elephantiasis, for example, lymph vessels are blocked by parasites, which compromises fluid drainage. Lymphatic System As noted above, the hydrostatic pressure in the interstital space is slightly negative. This is largely due to the presence of the lymphatic system, and the movement of fluid into this system. As long as the interstital pressure is negative, no edema will occur. In addition to removing fluid, the lymphatic system is a conduit for protein to leave the interstitial space. Without the actions of the lymphatic system, the oncotic gradient between the plasma and interstital space would equalize, which would contribute to the development of edema. Changes in Plasma Osmolarity and Cell Size • Most capillaries are highly permeable to small ions such as Na+ and Cl- and water. • Although cell membranes normally are quite selective about the ions that enter or leave, and actively maintain very low intracellular Na+ levels through Na+/K+ ATPase, they are freely permeable to water. • As a result, a sudden change in the osmolarity of the plasma can result in water entering or leaving body cells, thereby causing them to expand or shrink. Example: Infusion of Hypertonic Saline Hypertonic Saline H2 O H2 O • Intravenous delivery of hypertonic saline results in the osmolarity of the intravascular space being higher than the interstital space. • Consequently, water leaves the interstitial space (osmosis) until the water concentration on the two sides of the capillary are equal. • As a result, the water concentration is higher in the intracellular space than in the interstitial space, and water leaves the cell. Cell Shrinks • Due to the loss of fluid, the cell shrinks. Example: Infusion of Hypotonic Saline Hypotonic Saline H2 O H2 O • Intravenous delivery of hypotonic saline results in the osmolarity of the interstitial space being lower than the intravascular space. • Consequently, water leaves the capillary (osmosis) until the concentration on the two sides is equal. • As a result, the water concentration is higher in the interstitial space than in the intracellular space, and water enters the cell. • Due to the gain of fluid, the cell expands. Cell Expands • Rapid infusion of hypotonic saline can cause red blood cells to explode!