Session 3: Microcirculation
advertisement

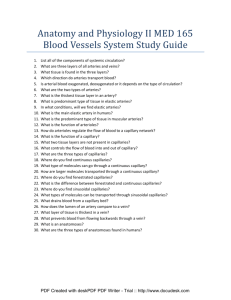
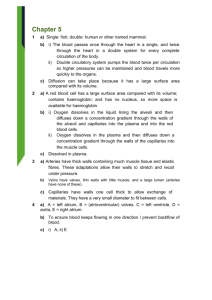
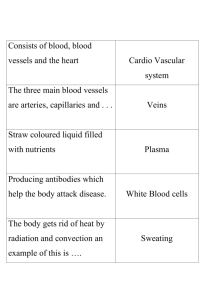
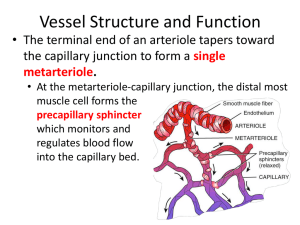
Session 3: Microcirculation 1) Describe the general structure of a vascular bed and the factors controlling its flood flow The microcirculation is made up of the smallest arterioles, and exchange vessels, including the capillaries and the postcapillary venules. The transfer of water, gases nutrients, waste materials and other substances between the blood and the body tissue is carried out by the exchange vessels. Exchange can only be carried out over the surface, hence there is a need to maximise the capillary surface-area, and this requires a lot of vessels. There is a problem, i.e. the blood cells must be able to get through. Hence they are flexible and get through very narrow tubes, but there is a limit at a little below 3μm Hence the smallest capillaries are about 4μm in diameter, but mostly in the range 5-10μm (remember the diameter of a RBC is about 7-8µm in diameter). And there is a colossal number, running into billions, giving a surface area of some 100-1000m2. No tissue is far from a feeding capillary in the healthy subject. NB There is redundancy! (i.e. that more than one capillary bed can supply the same bit of tissue) Blood enters the microcirculation via small arterioles, the walls of which contain smooth muscle cells. These vessels are densely innervated by the sympathetic system, particularly in the splanchnic (gut) and cutaneous (skin) vascular beds. Sympathetically mediated constriction of each small arteriole reduces the blood flow to many capillaries. In the vast majority of tissues, the smallest or terminal arterioles divide to give rise to sets of capillaries. The terminal arteriole itself can act as a pre-capillary sphincter for its entire cluster of capillaries. Terminal arterioles are not innervated, and their tone is controlled by local metabolic factors: these include adenosine, k+ ions, hypercapnia (increased PCO2) and local hypoxia (reduced PO2). All of these lead to the relaxation of vascular smooth muscle cells and therefore vasodilation, resulting in increased blood flow to these areas. ‘Oxygen tension’ is one form of local auto-regulation. If a capillary bed is watched over a period of time it will be seen that the flow is intermittent with a periodicity of 1-10cycles/min. This is called Vasomotion. It is probably driven by the O2 mechanism. It means, in the resting subject, that a considerable portion of the capillaries are not open at any one time. It also means that there is a large reserve to be called upon when necessary, e.g. during exercise. 2) Describe the structure of a capillary wall The capillary wall unlike the artery or vein walls is only made up of one layer: the tunica interna (or intima). The wall is only one cell thick – and this cell layer is called the endothelium. 3) Explain the mechanisms responsible for the exchange of materials across the capillary wall including starling’s hypothesis Lipid soluble proteins such as O2 and CO2, alcohol and steroid hormones may pass directly through the lipid bilayer of the endothelial cell plasma membranes. Therefore these substances have the entire capillary surface to move across. The movement is by diffusion and governed by fick’s equation: dQ/dt = D.A.(dc/dx) (The direction of movement depends on the concentration gradient dc/dx). The area A is huge so the rate of equilibration across the capillary wall is extremely high and this means that there is very little difference in concentration of these materials in the blood and the interstitial fluid. For all practical purposes they can be taken as the same. Small water soluble materials, e.g. glucose and ions, have to follow the water filled gap junctions in continuous capillaries. Although’ these are small, ~only 10nm across, the movement is so fast that there is again almost complete equilibration across the capillary wall. So there is little difference in concentration of these materials between the blood and the interstitial fluid. Large water soluble materials, i.e. proteins, are very hindered by the gap junctions and it is thought that much of their movement is via the vesicles. But the result is that there is a substantial difference in concentration between the blood and the IF. On average the protein concentration in the IF is only ~1/4 of that in the blood plasma. (Note this does not apply to the discontinuous capillaries!) Fenestrations common where rapid water movement is necessary e.g. the kidney. Discontinuities (or sinusoids) are common where easy movement of large molecules , or even cells, is necessary, e.g. the liver and bone marrow The movement of water through the walls of capillaries is governed by the pressure differentials across the walls and the fact that the walls are permeable - Ultrafiltration. There are two pressures of relevance here:- The pressure in the blood derived from the heart compared with the very low level in the IF. This results in an outward drive. - The osmotic pressure difference between the blood and the IF due to the difference in protein concentration in the two areas (Oncotic pressure). This results in an inward drive - These are referred to as the Starling Forces and the concept as Starling’s Hypothesis The result is a small, continuous but significant loss of water from the blood this, and any leaked protein, must be returned to the blood. This is the role of the Lymphatic System 4) Describe the essential structure of the lymphatic system and its role in body fluid control Most body tissues contain lymphatic capillaries, these are blind-ended bulbus tubes (15-75µm in diameter), with walls made up of a monolayer of endothelial cells. Interstitial fluid, plasma proteins and bacteria can easily enter the lymphatic vessels through gaps between these cells, the arrangement of which prevents these substances from escaping. Theses lymphatic capillaries merge to form collecting lymphatics, the walls of which contain smooth muscle cells and one-way valves. The lymph has the same composition as IF fluid Total flow ~120 ml/h, i.e. returns ~plasma volume /day Movement facilitated by muscle pump, SM contractions in the walls and valves of larger vessels 5) Explain the factors that may lead to oedema Oedema is the accumulation of excess interstitial fluid in the extra-vascular compartment; it may result from a high MABP (leading to increased hydrostatic pressure), venous obstruction (congestion leads to an increase in capillary pressure), leakage of plasma proteins into the ECM (reduces oncotic effect that pulls water back into capillaries), decreased plasma protein concentration due to disease (same consequences) and obstruction of lymphatic drainage (causing a build up of interstitial fluid) A dramatic form results from blockage of lymph nodes by parasites-leading to elephantiasis