Edema
advertisement

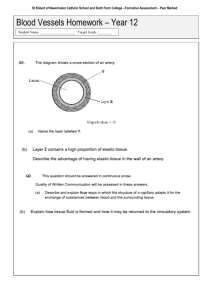
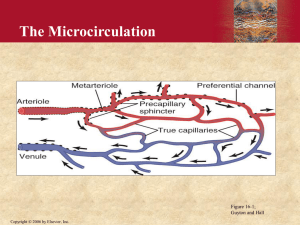
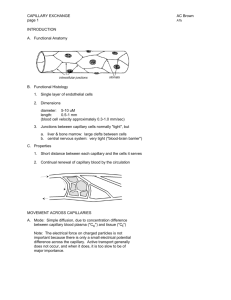
Cardio February 3rd, 3:00PM Dr. Downey Matt Messa Page 1 of 3 Lymphatic and Interstitial Fluids Edema We have all seen pictures of children in other countries who have bloated bellies from not eating enough protein A shortage of amino acids in the serum decreases the colloid osmotic pressure in the vessels severely There is less pressure to act as a retaining force in the capillary, so fluid leaves the vessels for the interstitial spaces This increases the tissue pressure significantly above its normal level of about zero mm/Hg Lymphatics try to remove the excessive filtration out of the circulation along with the plasma protein that have filtered out from the capillaries The tissue colloid osmotic pressure is not has high as would be expected though because protein is being washed into the lymphatics Does an increase in filtration always cause edema? NO NO NO This is because the lymphatics are like a sump pump in your basement. For you nonhandy people out there, a sump pump is a pump that is a rescue device designed to prevent flooding in your basement. It pumps the water out before it has a chance to come into the home. The rate of fluid removal by the lymphatics is influenced by the pressure back in the interstitial space. As the pressure increases, the efflux of fluid and the wash out of plasma protein will increase. Obstruction of lymphatic drainage Picture (the one with the HUGE leg) Recall that the lymphatics are essential for removing fluid and protein that enters the interstitial space from the capillaries Slowly, the colloid osmotic pressure of the tissue will increase, and it will continue to increase until the protein concentration is higher than the protein concentration in the blood capillaries. When that occurs, the tissue colloid osmotic pressure of the tissues is so high that water leaves the vascular space to enter the interstitial space. Dr. Downey pointed out that this does happen in the real world, and that it is often related to malignant obstruction of the lymphatics. In fact, he had a colleague professor that had an obstruction from a breast cancer (and yes he was male) that obstructed the axillary lymph drainage to cause unilateral edema of the chest wall The last example Dr. Downey used was the example of what occurs when we get bit by an insect. The toxins from the insect increase capillary permeability which allow proteins to escape, resulting in increased tissue osmotic pressure, which causes fluid to shift from the capillaries and causes swelling Be able to process the information in a way that you can know whether filtration or absorption will occur in any specific example where you are given all the numbers of the various pressures as in the powerpoint slides. Cardio February 3rd, 3:00PM Dr. Downey Matt Messa Page 2 of 3 Question by someone in the back, I think Lili….. SHE’S going to be a fine physician. Do we need to know all the normal values for the pressures??? Dr. D- YES. And he gave the normals once again. Here they are Capillary Pressure (BP) aka…(Mean fluid pressure of the capillary)- 25 Capillary colloid osmotic pressure- 28 Tissue Hydrostatic Pressure aka…(Tissue Pressure, or Interstitial Fluid Pressure)- 0 Tissue Colloid Osmotic Pressure -6-7 Lymph Flow There are some large spaces between lymphatic capillary endothelial cells where 2 endothelial cells overlap, and there are often filaments extending out from these sites (see figure 31-2 in ppts). These filaments are thought to control the opening and closing of these junctions to allow the passage of fluid and proteins into them (to be transported away from the tissues) It is also thought that these overlapping junctions allows overlapping compression during states of high pressure in the capillary lymphatics. This allows the lymph to not leak out of the capillary and instead head back to the venous network in the thorax. There are also a lot of valves in the lymphatic capillaries that allow for less backflow. Recall that lymph flow is controlled by muscular compression in the same manner as venous flow. Graph (figure 31-4) in the ppts. The relative lymph flow can probably increase up to 20 x normal Ignore the fact that this graph shows tissue pressure to be below zero. This is because the physiology book by “Guyton” believes this. Dr. Downey told me that this is still theory and that we should follow the principle that normal tissue pressure is about 0. This graph shows that the lymph flow increases dramatically as the filtration causes increases in interstitial pressures (tissue pressures). Lymph flow does not reach its maximum until it is 20 x its normal flow. This is a built-in safety factor that keeps small increases in lymph flow from causing noticeable edema. Reminder about Complete Lymphatic Obstruction (figure “C” in the ppts) The big deal here is that tissue pressure has now matched the capillary fluid pressure (This does not happen in any other condition) This is because the tissue colloid osmotic pressure has risen so high to pull fluid out of the capillary Margin of Safety There are many ways that the body can avoid a state where edema builds up. Precapillary resistance (via arterioles) can increase to decrease the flow to the capillary, which will decrease capillary pressure to prevent edema distally. Cardio February 3rd, 3:00PM Dr. Downey Matt Messa Page 3 of 3 Interstitial pressures can also accumulate high enough that they increase transmural pressure around supplying arterioles, to again create less flow into the capillaries. Both of these first two conditions create a capillary that has a low hydrostatic pressure (capillary pressure), and actually causes it to absorb fluid from the interstitium and transport it back in the venous network. This is backwards because capillaries usually filter, not absorb. As filtration increases excessively from the capillaries, the interstitial proteins get diluted and this causes a decrease in the tissue colloid osmotic pressure. This is another safety valve to prevent excessive lymph accumulation. Lastly, if there is an increase in interstitial pressure (tissue pressure), this causes interstitial fluid to move into the lymphatic capillaries. Coincident with this, the proteins in the interstitium wash out as well and this contributes to less colloid osmotic pressure in the tissues, which will be another safety valve to prevent edema.