Chapter 14 Section A Blood
advertisement

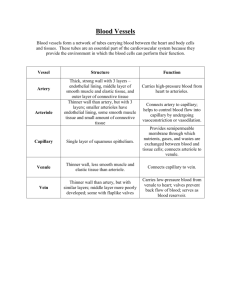
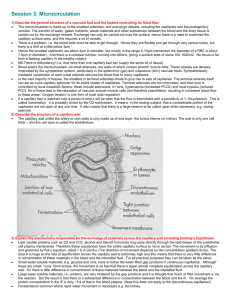
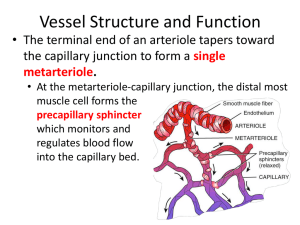
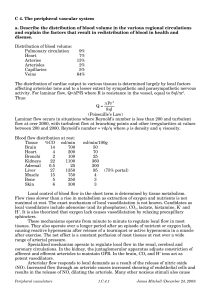
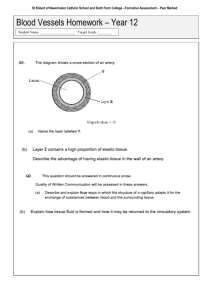
6 Chapter 12 Section C The Vascular System Revised 20 November 2011 What type of cell lines blood vessels of all types and lines the lumen of the heart chambers? How do arteries act as pressure reservoirs? What is the mathematical definition of compliance? Are arteries considered highly compliant? How do smooth muscles affect compliance of arteries? What are the normal values for systolic and diastolic pressure and pulse pressure? Why doesn't arterial pressure fall to zero between heart beats? What would mean arterial pressure be if systolic pressure is 130 and diastolic pressure is 80 mmHg? How does blood pressure typically change with advancing age? Why so? What are Korotkoff’s sounds? Are these sound heart murmurs? What are the two major functions of arterioles? How do arteriolar smooth muscles mediate vasodilation or vasoconstriction? What is intrinsic tone? How does local control of blood flow differ from extrinsic control? What is the difference between hyperemia, active hyperemia, and reactive hyperemia? What are some of the local chemical factors that lead to arteriolar dilation? What effect do these factors have on arteriolar smooth muscle? In which tissues is local control of blood flow predominant? How is local control good for matching blood flow to metabolic rate of the tissue? What is it called when blood flow is kept relatively constant in spite of changes in blood pressure? How are local metabolic factors involved in this phenomenon? Since the same factors are at work in flow autoregulation and active hyperemia, how do they initially differ? What is the myogenic response and what ion is involved? What is reactive hyperemia? What effect does norepinephrine have on vascular smooth muscle? Which receptor type is involved? 7 Why don't "beta blockers" have a large effect vascular smooth muscle? How can vasodilation be achieved via the sympathetic nerves? Is it typical for arteriolar smooth muscle to be "dually innervated?" What is the source of nitric oxide, a vasodilator? (Caution….there are actually two important sources!) In which arterioles is this agent important? How can epinephrine cause arteriolar smooth muscle to either contract or relax? What are the effects of angiotensin II, vasopressin, and atrial natriuretic factor on arteriole diameter? Name two vasodilators and one vasoconstrictor released by endothelial cells. According to table 12-5, which organs have their blood flow determined mainly by flow autoregulation? In which is blood flow controlled mainly by local metabolic factors? At any moment, what percentage of blood volume is in the capillaries? What is the diameter of a capillary? How does this compare to the diameter of an erythrocyte? Define angiogenesis. What are intracellular clefts of capillaries? How does a fused vesicle channel form in a capillary? What are metarterioles and what is their function? What is the function of precapillary sphincters? In which type of blood vessel is blood velocity the slowest? the fastest? How is it possible for blood velocity to be faster in veins than in capillaries, especially since the pressure is lower in veins? Why isn't the resistance of capillaries, which are obviously smaller diameter than arterioles, greater than the resistance of arterioles? What are the 3 means by which substance move across capillary walls? Which of these is most important for moving nutrients, gases, and waste products? What is unusual about the capillaries of the brain? Which organs have capillaries that are the "tightest?" the "leakiest?" How does metabolism affect the rate of diffusion? What is the difference between diffusion and bulk flow? 8 What is the purpose of bulk flow? Why aren't plasma proteins found in the extracellular fluid? What is the difference between a crystalloid and a colloid? What are the four Starling forces? Which of these is controlled by arterioles? For each of the following scenarios, how would bulk flow be affected? That is, would the change result in more filtration or more absorption? A) an increase in Pc (capillary hydrostatic pressure); b) in increase in PIF (interstitial fluid hydrostatic pressure) c) an increase in ∏C (capillary oncotic pressure); and d) an increase in ∏IF (interstitial fluid oncotic pressure.) For each of the 4 scenarios above, what would be a “real world” example of such a change? In other words, what would cause an increase in Pc? in PIF? in ∏C? ∏IF? How is it possible for net filtration to occur at the arteriolar end of a capillary and net reabsorption to occur at the venular end of a capillary? What is the fate of the 4 liters per day of net capillary filtration? Why doesn't net filtration normally occur in pulmonary capillaries? In what way are venules like capillaries? Why do veins have valves? How is venous pressure related to end-diastolic volume and stroke volume? At any moment in a resting person, what percentage of blood volume is in veins? How does sympathetic input affect venous compliance and venous pressure and venous return? Explain how the skeletal muscle pump and the respiratory pump assist venous return to the heart. Beginning with the extracellular fluid, trace the path of a molecule through the lymphatic system and ultimately back into the bloodstream. What is edema? Why is it that the lymphatic system is often the means by which cancerous cells spread? What drives the fluid movement through the lymphatics? What would happen to the volume of interstitial fluid in a region of the body where they lymphatic system became blocked?