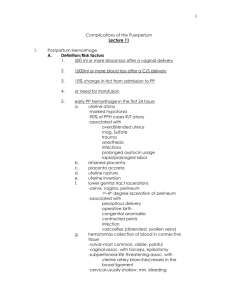
First, boil water… Obstetrics for Paramedics
advertisement

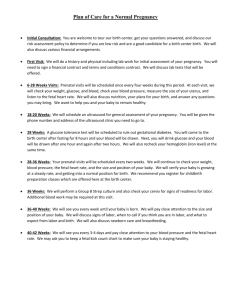
First, boil water… Obstetrics for Paramedics Rebecca Dunsmoor-Su, MD Outline • The basics (anatomy, terminology) • Normal pregnancy • Abnormal pregnancy – First trimester – Later • • • • Trauma Normal labor & delivery Abnormal labor & delivery What do you do with the baby? Anatomy Anatomy Terminology • • • • • • • • Gs and Ps LMP EDC Primip Multip Precip Antenatal Antepartum Terminology • Gravidity: Number of times pregnant • Parity: Number of deliveries (twins only counts as one) • Usually expressed as G3P2 • Can also be G3P2012 – P(term, preterm, abortions, living kids) Terminology • LMP: Last menstrual period. Pregnancies are dated from the first day of the LMP • EDC: Estimated date of confinement (EDD: estimated date of delivery) • For a rough estimate: Add 7 days to 1st day of LMP, then add 9 months. (Nagele rule) Terminology • Primip: Primipara. Technically, someone who has had one delivery. Practically, used interchangably with primagravida • Multip: Multipara. Techinically, someone who has delivered more than one baby. Practically, anyone who has delivered a baby. Terminology • Precip: Precipitous delivery. One that happens way too fast - and what you are most likely to see in your ambulance! Technically, delivery after less than 3 hours of labor. • Antenatal, Antepartum: Before delivery Normal pregnancy • Heartbeat visible on US: 5-6 weeks • Heartbeat audible with Doppler: 12 weeks • Heartbeat audible with stethoscope: 20 weeks • Viability: 24 weeks • Term: 40 weeks (>37 weeks) Normal pregnancy • Uterus palpable above pubic bone ~12 weeks • Uterus at umbilicus at 20 weeks • After 20 weeks, cm measured from symphysis to fundus is approx = to GA Fundal height Fetal HR 120-150 Physiologic changes • Respiratory: Progesterone increases respiratory drive, therefore increased rate, slightly lower PCO2 • Cardiovascular: Drop in SVR, drop in BP, increase in pulse. Increased blood volume. • Renal: Progesterone relaxes ureter, increasing risk of pyelonephritis • GI: Progesterone relaxes sphincters, slows peristalisis: increasing GERD Physiologic changes • Hematologic: Increased blood volume, but less increase in RBCs leads to relative anemia • MSK: Progesterone loosens joints, growing uterus changes center of gravity Beware supine hypotension! ALWAYS: Left lateral tilt Evaluation of a pregnant patient • ABC’s. • Mom is first priority, but always remember that you have TWO patients. • Primary survey is the same. Evaluation of a pregnant patient • Secondary survey: – Include palpation of uterine fundus – Listen for fetal heartbeat – Vaginal bleeding or leaking of fluid? – Anything protruding from vagina? – Tender abdomen? Obstetric HPI • • • • • • • Gs and Ps LMP / EDC Bleeding? Leaking fluid? Contracting? Baby moving? Medical Comorbidities? • Any prenatal care? • • • • • • Headache? Blurry vision? RUQ pain? Seizures? Trauma? Fall? Any problems with placenta? Obstetric History • POBHx: – Any C-sections? – Any surgery on uterus? – Any problems with past pregnancies? Physical exam • • • • • • Pulmonary Abdominal Uterus Fetus Perineum DO NOT do an internal vaginal exam! Abnormal pregnancy First Trimester (0-14 weeks) Bleeding: • Up to 20% of pregnancies end in miscarriage • Vaginal bleeding in the first trimester should ALWAYS make you think of ectopic pregnancy • If patient appears sick, consider septic abortion and ask about medications or instrumentation • Inevitable vs. Threatened vs. Incomplete Abnormal pregnancy First Trimester uterus ectopic • All pregnant women with bleeding and/or abdominal pain have an ectopic until proven otherwise. • Bleeding ectopic is a true OB/Gyn emergency and needs to get to an OR Abnormal pregnancy after 20 weeks Bleeding: Medical: • Placenta previa • Pre-eclampsia • Placental abruption • Eclampsia • Preterm labor • Diabetes • PPROM Placenta previa Painless vaginal bleeding Associated with placenta accreta (placenta growing into uterine wall) ANY bleeding is a bad sign, proceed with haste. Placental abruption Painful vaginal bleeding Signs: Bleeding, contractions, abdominal tenderness, pain Risk factors: Cocaine, Trauma, HTN, PPROM, Smoking, Multiparity Preterm labor • Technically, labor prior to 37 weeks. Practically, no treatment to stop contractions if >34 weeks. • Difficult diagnosis in the field, since labor implies cervical change. • Err on the side of caution and presume any abdominal or back pain is contractions. • Many causes PPROM Preterm Premature Rupture of Membranes Sometimes hard to diagnose Often caused by infection Associated with increased risk of abruption, cord prolapse, cerebral palsy (when accompanied by infection) Pre-eclampsia • Blood pressure >140/90 • Proteinuria >1+ (300mg/24h) • Symptoms: • Headache • Blurry vision • RUQ pain • Edema • Signs: • Hyperreflexia • Pulmonary edema • Oliguria Pre-eclampsia • Associated with: • Seizures (eclampsia) • Stroke • HELLP: • Hemolysis • Elevated Liver enzymes • Low Platelets • Abruption Key treatment: Magnesium sulfate and/or delivery Diabetes • Placenta makes a hormone, HPL, that creates insulin resistance. • Pre-existing diabetes is worsened by pregnancy • Some women develop gestational diabetes (like Type 2) and may be on insulin (so think about hypoglycemia) • DKA can develop more quickly and at lower blood sugar than in non-pregnant women Trauma • Number one cause of non-obstetric maternal death • Treat mom first • Volume, volume, volume (be careful) • Remember left lateral tilt • Fetal survival drops dramatically 15 minutes after a maternal arrest, but 90% will survive if C-section done prior to 15 minutes. • All but the most minor trauma over 24 weeks will have at least 4 hours of uterine monitoring to evaluate for abruption. (After 20 weeks - 5 months - ideal to transport everyone for evaluation) Normal labor and delivery What do we mean by labor? 3 stages of labor Stage 1: 0-10 cm dilation (Active phase after 34cm) Stage 2: 10cm to delivery Stage 3: delivery of baby to delivery of placenta Delivery • Don’t panic. • Control the infant head • Support maternal perineum • Once head is out, sweep for nuchal cord • Gentle downward traction, then gentle upward traction • Support fetal body Nuchal cord Third stage • Signs of placental separation: • Gush of blood • Lengthening of cord • Avoid heavy traction on the cord • Monitor for increased bleeding • Fundal massage • Pitocin (20 units in 1 litre) - can start this as soon as the baby is out. Abnormal labor and delivery • Prolapsed cord • Cephalopelvic disproportion • Shoulder dystocia • Breech presentation • Limb presentation • Meconium • Uterine rupture • Post-partum hemorrhage • Uterine inversion • Amniotic fluid embolus • Pulmonary embolus Prolapsed Cord • OB emergency: essentially cuts off all oxygen to fetus • Cesarean delivery STAT • In field: hand in vagina, elevate fetal head off the cord. • Elevate hips: knee to chest or Trendeleberg Cephalopelvic disproportion Prolonged labor • Minimal expected cervical change is ~1cm/hr in active phase. • Slower rate can indicate malposition, large baby, inadequate contractions Shoulder dystocia Anterior shoulder stuck behind pubic symphysis Signs: • Shoulder does not deliver easily with next contraction • Head retracts “turtle sign” McRoberts maneuver: Knees to ears! This is like a code: document, document, document Abnormal presentation Breech Footling breech Limb presentation Risks: Head entrapment Cord prolapse Breech delivery Allow progress of labor and pushing to deliver baby past hips Support the infant body, and wrap it in a towel Grasp infant at hips, with thumbs on sacral alae Pull gently down until you see the scapula Reach up and sweep down each arm Put fingers on maxillae to flex head and/or provide space for baby to breathe Meconium • Theory is that it indicates baby under stress • Previously all babies with meconium had deep suction prior to delivery of shoulders. • Now, only those with poor respiratory effort or sats should be intubated and suctioned. • Suction mouth and nose on perineum and be prepared. Uterine rupture Signs: • Vaginal bleeding • 0.5-1% risk in women with one prior C-section • Loss of fetal station • 5-50% risk of fetal death • Abdominal pain • Risk of maternal hemorrhage • Acute abdomen • Fetal distress • Maternal shock Post-partum hemorrhage • >500cc after vaginal delivery • Can be a sign of uterine atony, retained placenta, placenta acreta •Rx: • Fundal massage • Empty bladder • Pitocin (20-40units in 1L NS) • Misoprostol 600-800mcg per rectum • Hemabate / methergine Uterine Inversion Try to gently push it back in. Do not remove placenta! Proceed with haste to an OB Emboli Amniotic fluid or blood clot Present as sudden hypoxia, dyspnea, cardiovascular compromise Treat as any patient in shock, pulmonary arrest or with severe hypotension What do I do with the baby? Airway & Breathing Tone & Reflexes Circulation & Color Dry the baby and keep her warm: skin to skin is best APGAR Score Appearance: Grimace: Respiration 0 = blue or white 0 = No response 0 = Absent 1 = pink body, blue extrem. 1 = grimace 2 = pink 2 = Cries 1 = Slow or irregular 2 = Strong cry Pulse 0 = absent 1 = <100 2 = >100 Activity 0 = limp 1 = Some flexion 2 = Active movement Neonatal resuscitation A: Airway: Is it clear of meconium? Is the head properly positioned? B: Breathing: Is there respiratory effort? Is the baby pink? C: Circulation: Is there a pulse in the umbilical cord? Is the heart rate >100? Neonatal resuscitation Poor color Blow-by O2 Stimulation Evaluate respirations, heart rate and color Apnea HR <100 HR <60 Positive-pressure ventilation HR <60 Chest compressions Consider intubation Epi Questions?