OB/GYN EMERGENCIES
advertisement
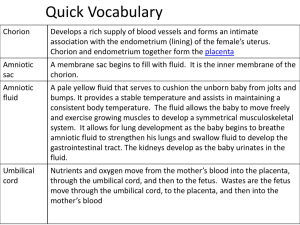
OB/GYN EMERGENCIES Anatomy & Physiology Review Menses • Onset 12 - 13 years old • Periodic discharge of blood , mucus and cellular debris • Menstrual cycle lasts 28 days • Menstrual flow lasts 4-6 days (endothelium) • Menopause occurs between ages 35 - 60 Fertilization & Implantation At ovulation , an egg is released from the ovary and begins its journey through the fallopian tubes . While in the tube the egg is fertilized by the sperm . Once the egg reaches the uterus implantation will occur . Fetal Development •8 weeks , Embryo •Through out the pregnancy , Fetus •Upon delivery , Newborn Maternal Changes During Pregnancy •Genital - Uterus, Bladder, Breasts, cervix •Gastrointestinal - Stomach, Liver, •Cardiovascular - Heart >, CO >, Circulation •Respiratory - Tidal volume <, RR > Baby Position Specialized Structures of Pregnancy •Placenta •Umbilical Cord •Amniotic Sac Placenta Serves as the organ of exchange between the mother and the fetus . •Transfers gases •Transports nutrients •Excretion of wastes Amniotic Sac Amniotic Sac is a fluid filled cavity that completely surrounds and protects the Embryo . Amniotic fluid originates from Fetal urine , skin and respiratory secretions . Vaginal Bleeding during Pregnancy Placenta Previa Painless bleeding in late 2nd or in 3rd trimester. Spontaneous. Risk of death for both mother and baby. Placental Abruption Bleeding associated with abdominal or back pain. Usually associated with a trauma; fall, MVC, Complications vary based on how far along the pregnancy is and the size of the abruption Some other causes for vaginal bleeding Etopic pregnancy Cancer Miscarrage STDs Management BSI High Flow O2 Prepare for and treat shock Emergent transport Stages of Labor Stage 1 •Pressure felt in the upper abdomen/contractions •Mucus plug expelled •Amniotic fluid released/sac ruptures •cervical dilation/Ending 1st stage Stage 2 •Complete dilation of the cervix •Contractions intensity increase/frequency •Urge to move her bowels •Crowning •Fetus delivers Stage 3 Delivery of the placenta, usually within 20 mins of the infant . Placental delivery is characterized by the lengthening of the umbilical cord and a sudden gush of blood Uncomplicated Delivery Signs of Imminent Delivery •Urge to move bowels •Water broken •Crowning •Length of contractions •Braxton Hicks ? •Distance between contractions Assessing of Imminent delivery Has the mother delivered other Children? Has the mother lost her mucus plug? Create sterile field around vaginal opening. Crowning of Infant’s Head Delivery Place gloved hand on presenting part to prevent “explosive” delivery Delivery Procedures If amniotic sac has not broken, puncture sac and pull away from baby's face. If umbilical cord is around baby’s neck, clamp and cut cord. Delivery of the Head—Prevent explosive delivery. Aid in birth of upper shoulder. Delivery Gently guide baby’s head down to deliver upper shoulder Gently guide baby’s head up to deliver lower shoulder Gently assist with delivery of rest of baby; Do NOT pull Note time of delivery of baby Support the trunk. Support the legs. Delivery Control slippery baby during delivery – Support head, shoulders, feet – Keep head lower then feet to facilitate drainage of secretions from mouth Dry baby Keep baby warm Delivery Procedures Wipe blood and mucus from nose and mouth. Suction as needed Warmth is critical! Wrap baby in warm towel, head lower than trunk. Delivery Procedures Have partner provide initial care and monitoring. Keep infant level with vagina until cord is cut. Delivery Flick baby’s feet, rub back to stimulate Do NOT shake infant Do NOT slap buttocks “Blow by” O2 if: – Heart rate < 100 – Persistent central cyanosis present Resuscitate if necessary Delivery Clamp, cut cord – First clamp about 4” from baby – Second clamp 2” further away from first – Cut between clamps – Use umbilical tape to control any bleeding from cord Clamp or tie cord; then cut. Delivery Procedures Observe for delivery of placenta. When placenta delivers, place in plastic bag for transport to hospital. Delivery “Deliver” Placenta – Place placenta in plastic bag and deliver to hospital to be examined for completeness – If placenta does not deliver within 10 minutes, transport Delivering the Placenta After-Delivery Procedures Cover vaginal opening with sterile pad. Lower mother's knees; help her to hold them together. Record time of delivery. After-Delivery Procedures Vaginal Bleeding A loss of 500 cc is well tolerated. If blood loss is excessive, massage the uterus. Treat for shock. Massage uterus to control bleeding. APGAR Postpartum Hemorrhage •Encourage the mother to breast feed the baby •Do not pack the vagina with dressings •Apply dressings to the exterior portion of the vagina to absorb the blood •Massage the uterus, place one hand on the lower abdomen feeling for a grapefruit size ball Blood lost Normal blood loss during the third stage of labor is about 150 ml – 500 ml Controlling excessive postpartum the same as normal postpartum bleeding If excessive bleeding rapid transport is needed Use pressure dressing Do not pack vagina