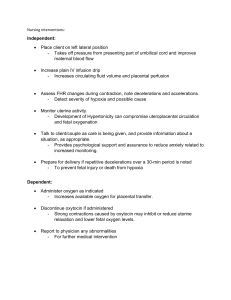
ABRUPTIO PLACENTA Before we go straight into the signs and symptoms of abruptio placenta or placental abruption, I would just like to reiterate its definition: placental abruption occurs when the maternal vessels separate from the placenta, which causes blood to accumulate between the uterine lining and the maternal side of the placenta. This accumulation of blood pushes the uterine wall and placenta apart, leading to the premature separation of the placenta before birth. Keeping this definition in mind, we can say that the signs and symptoms of placental abruption correlate to the following classifications, such that, according to Pamela Schmidt, et al., from the National Library of Medicine, the clinical manifestations depend on the degree of separation and the location of separation. It is also in this way that the classifications we deduce from the signs and symptoms are also the types of placental abruption. CLASS 0: Asymptomatic The clinical sign here is the discovery of a blood clot on the maternal side of a delivered placenta. Emphasizing on “delivered placenta,” this means that this class of abruptio placenta is diagnosed retrospectively or that it is only known after it has happened. CLASS 1: Mild The signs and symptoms here are: there may be LITTLE to no sign of vaginal bleeding, a slight uterine tenderness, normal maternal blood pressure and heart rate, and no signs of fetal distress. CLASS 2: Moderate The signs and symptoms here are: MODERATE to no sign of vaginal bleeding, significant uterine tenderness with tetanic/sustained contractions, maternal tachycardia and orthostatic changes in blood pressure, evidence of fetal distress and hypofibrinogenemia which may manifest as excessive or prolonged bleeding, especially after injuries or surgeries. CLASS 2: Moderate The signs and symptoms here are: MODERATE to no sign of vaginal bleeding, significant uterine tenderness with tetanic/sustained contractions, maternal tachycardia and orthostatic changes in blood pressure, evidence of fetal distress and hypofibrinogenemia which may manifest as excessive or prolonged bleeding, especially after injuries or surgeries. CLASS 3: Severe Lastly, the signs and symptoms here are: HEAVY to no sign of vaginal bleeding, a tetanic uterus or a uterus that is board-like or hard in consistency upon palpation, maternal shock (rapid heart rate, low BP, confusion, weakness, cold and clammy skin, among other subsigns and symptoms), hypofibrinogenemia and coagulopathy or impaired blood clotting, and even fetal death. Conversely, JoAnne Silbert-Flagg, in the Maternal & Child Health Nursing book, states the following general signs and symptoms for abruptio placenta: • Sharp abdominal pain, and/or a sharp, stabbing sensation in the upper uterine fundus as initial separation occurs • Uterine tenderness, as the blood continues to accumulate between the placenta and the uterine wall o this may also lead to a Couvelaire uterus when the blood infiltrates the uterine musculature, and this is the phenomenon of a hard, board-like consistency of the uterus upon palpation • Vaginal bleeding, • Signs of hypovolemic shock; and • Fetal distress. Considering all of that, the signs and symptoms of abruptio placenta must be thoroughly monitored, and it especially must be detected early in order to implement the necessary interventions to prevent the condition from worsening and causing further complications, the worst being maternal and/or fetal demise. NURSING MANAGEMENT Nurses play a role in the management of abruptio placenta, such that their early recognition of the signs and symptoms, timely intervention, and skilled nursing care are vital in lessening the occurrence of complications. Given so, here are the following nursing priorities in managing a patient with placental abruption: 1. Monitor maternal vital signs and assess for signs of shock. 2. Continuous fetal monitoring to assess fetal well-being. 1. Monitor fetal heart sounds externally every 5-15 minutes. 3. Place the woman in a lateral position to avoid pressure on the vena cava. 4. Administer oxygen therapy as needed. 5. Administer intravenous fluids and blood products as necessary. 6. Monitor and manage pain. 7. Assess and manage any associated bleeding. 8. Avoid performing any vaginal or abdominal examinations to prevent further injury to the placenta. 9. Prepare for a potential emergency cesarean section. 10. Assess the need for immediate delivery, especially if the client is in active labor and bleeding cannot be stopped. MEDICAL MANAGEMENT Keeping in mind that medical management differs from nursing management in their focuses, as the former is concentrated on treating the cause and the condition itself, whereas nursing management treats the patient’s responses to the condition, here are some medical interventions for abruptio placenta: 1. Begin continuous external fetal monitoring for the fetal heart rate and contraction. 2. Obtain IV access using 2 large-bore intravenous lines. 3. Institute crystalloid fluid resuscitation for the patient. 4. Type and crossmatch blood for the patient, in case of blood transfusions. 5. 6. 7. 8. Begin a transfusion if the patient is hemodynamically unstable after fluid resuscitation. Correct coagulopathy, if present. Administer Rh immune globulin if the patient is Rh-negative. Begin course of corticosteroids for fetal lung maturity (if the patient is less than 37 weeks gestation and they have not been previously given during pregnancy). PHARMACOLOGIC MANAGEMENT There are two pharmacologic components in treating abruptio placenta: 1. CORTICOSTEROIDS, which are used to accelerate fetal lung maturation in patients less than 37 weeks gestation. a. these drugs lessen the risks of premature delivery and also the risk of neonatal respiratory distress, necrotizing enterocolitis, and intracranial hemorrhage b. two of the most common corticosteroids used are: Betamethasone and Dexamethasone. 2. TOCOLYTIC THERAPY, which allow effective administration of gluco- or corticosteroids to the preterm fetus. a. these drugs are also believed to stop the abruption cycle because they prevent contractions which may worsen placental separation and exacerbate bleeding b. two of the most common tocolytics used are: Nifedipine and Magnesium Sulfate, both of which decrease contractions, but the latter, MgSO, is the drug of choice for tocolysis in abruptio placenta. SURGICAL MANAGEMENT These measures are employed usually only when the condition has progressed critically and endangers both the mother and fetus. In most cases, cesarean delivery is the preferred method of birth as it facilitates rapid delivery and direct access to the uterus, but in cases wherein a fetus has died due to placental abruption, the preferred method is vaginal delivery, although its completion depends on the mother’s condition. A hysterectomy may be done after, in the worst-case scenario wherein a pregnant woman develops a disseminated intravascular coagulation (DIC) and is at-risk for bleeding out. A C-hysterectomy is done in place if bleeding cannot be controlled in that same scenario.