Case 1
advertisement

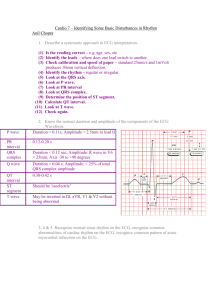
Introduction to ECG Interpretation Electrocardiogram interpretation is an invaluable clinical skill that is taught in many different ways at medical schools across the country. It is often informal and clinicians are expected to "pick it up" as they see patients on the wards and in clinics. There are many "courses" which can be purchased off the shelves at the bookstore -some of them too simplistic and others hopelessly detailed. In an effort to better meet the needs of ecg interpretation this course started out at UW Madison as a self study manual with some workshops where clinicians reviewed tracings with preceptors. The popularity of this course was immediate - we soon had clinicians asking for it on other rotations and the workshops were often visited by an assortment of clinicians from the health care fields. Reasons identified for the course's success was that it was directly applicable to patient care, a skill that was enjoyable to master, of value as a lifelong career tool (ecg interpretation content has been stable for years),and "adult learning" principles were respected. This computerized version of the course has some significant improvements. At the end of each content area is a quiz. This not only reinforces the material but the advanced clinician can try the quiz first, if they already feel comfortable with the content material, and go on to another section, to optimize their time. The tool bars at the bottom of the page allow this flexibility to go directly to any section. The "guidelines" which summarize the ENTIRE interpretive process can be printed out on a single page and carried in the lab coat pocket when seeing patients. The clinical cases at the end are an assortment of real life cases to demonstrate that ecgs are always interpreted in the context of patient care and not in a "vacuum". Differential diagnosis is emphasized to encourage thinking about the "art" of interpretation, not just a cookbook mechanistic approach. In addition, this course sets up the basic skills needed for interpretation in a self directed learning format, allowing clinicianpreceptor interaction to focus on more advanced patient specific ecg correlation Primer on Basic Concepts P wave = depolarization of the atria. QRS = depolarization of the ventricle. T wave = repolarization of the ventricle 1. Cardiac muscle cells depolarize with a positive wave of depolarization, then repolarize to a negative charge intracellularly. 2. Skin "leads" or electrodes have a positive and negative end. 3. A positive wave form (QRS mainly above the baseline) results from the wave of depolarization moving towards the positive end of the lead. A negative waveform (QRS mainly below the baseline) is when a wave of depolarization is moving away from the positive 4. electrode (towards the negative end of the lead). 1. ECG paper has 1 millimeter small squares - so height and depth of wave is measured in millimeters. 10 mm = 1.0 mVolt 2. Horizontal axis is time. .04 seconds for 1 mm (1 small box). .2 seconds for 1 large box = 5 small boxes = 5 x .04 seconds. Positive QRS in Lead I. Negative QRS in Lead aVR. R wave = 7-8 mm high in Lead I. QRS wave = .06 seconds long in Lead I. 1.Lead nomenclature. Limb lead Chest lead Rhythm strip I, II, III aVR, aVF, aVL V1 - V6 Located on the bottom of the ECG printout. Selected to give the best relationship of the P wave to the QRS Figure 3: A normal ECG and rhythm strip 1.ECG interpretation: look at five areas, in order, on each ECG. Rate Rhythm (Intervals) Axis Hypertrophy Infarct Hypertrophy Hypertrophy criteria are fairly straightforward; we will be looking for enlargement of any of the four chambers. 1. LVH: (Left ventricular hypertrophy). Add the larger S wave of V1 or V2 (not both), measure in mm, to the larger R wave of V5 or V6. If the sum is > 35mm, it meets "voltage criteria" for LVH. Also consider if R wave is > 12mm in aVL. LVH is more likely with a "strain pattern" which is asymmetric T wave inversion in those leads showing LVH. 2. RVH: (Right ventricular hypertrophy). R wave > S wave in V1 and R wave decreases from V1 to V6. 3. Atrial hypertrophy: (leads II and V1). Right atrial hypertrophy - Peaked P wave in lead II > 2.5mm amplitude. V1 has increase in the initial positive deflection. Left atrial hypertrophy - Notched wide (> 3mm) P wave in lead II. V1 has increase in the terminal negative deflection. Figure 32: Right ventricular hypertrophy and right atrial enlargement. Figure 33: Left ventricular hypertrophy (S wave V2 plus R wave of V5 greater than 35mm) and left atrial enlargement (II and V1). Take the hypertrophy quiz. #1 Hypertrophy Left ventricular and left atrial hypertrophy. S wave in V2 plus R wave in V5 > 35. The left atrial hypertrophy is noticaeable by a P wave that is long in lead II, with an increase in the negative terminal deflection in lead V1. [Done]. #2 Hypertrophy Left ventricular and left atrial hypertrophy. The R wave in aVL is greater than 12mm. The left atrial hypertrophy is barely noticeable by a P wave that is notched and wide in lead II and with an increase in the negative terminal deflection in lead V1. [Done]. #3 Hypertrophy Right ventricular and right atrial hypertrophy. The R wave is greater than the S wave in V1 and the R wave gets progressively smaller from V1 to V6. Normally, the R wave should increase from V1 to V6. The right atrial hypertrophy is marked by peaked P waves in lead II and a large intitial positive deflection of the P wave in lead V1. Infarct Accurate ECG interpretation in a patient with chest pain is critical. Basically, there can be three types of problems ischemia is a relative lack of blood supply (not yet an infarct), injury is acute damage occurring right now, and finally, infarct is an area of dead myocardium. It is important to realize that certain leads represent certain areas of the left ventricle; by noting which leads are involved, you can localize the process. The prognosis often varies depending on which area of the left ventricle is involved (i.e. anterior wall myocardial infarct generally has a worse prognosis than an inferior wall infarct). V1-V2 anteroseptal wall V3-V4 anterior wall V5-V6 anterolateral wall II, III, aVF inferior wall I, aVL lateral wall V1-V2 posterior wall (reciprocal) Infarct 1. Ischemia Represented by symmetrical T wave inversion (upside down). The definitive leads for ischemia are: I, II, V2 - V6. 2. Injury Acute damage - look for elevated ST segments. (Pericarditis and cardiac aneurysm can also cause ST elevation; remember to correlate it with the patient. 3. Infarct Look for significant "patholgic" Q waves. To be significant, a Q wave must be at least one small box wide or one-third the entire QRS height. Remember, to be a Q wave, the initial deflection must be down; even a tiny initial upward deflection makes the apparent Q wave an R wave. Figure 34: Ischemia: Note symmetric T wave inversions in leads I, V2-V5. Figure 35: Injury: Note ST segment elevation in leads V2-V3 (anteroseptal/anterior wall). Figure 36: Infarct: Note Q waves in leads II, III, and aVF (inferior wall). For the posterior wall, remember that vectors representing depolarization of the anterior and posterior portion of the left ventricle are in opposite directions. So, a posterior process shows up as opposite of an anterior process in V1. Instead of a Q wave and ST elevation, you get an R wave and ST depression in V1. Figure 37: Posterior wall infarct. Notice tall R wave in V1. Posterior wall infarcts are often associated with inferior wall infarcts (Q waves in II, III and aVF). Two other caveats: One is that normally the R wave gets larger as you go to V1 to V6. If there is no R wave "progression" from V1 to V6 this can also mean infarct. The second caveat is that, with a left bundle branch block, you cannot evaluate "infarct" on that ECG. In a patient with chest pain and left bundle branch block, you must rely on cardiac enzymes (blood tests) and the history. #1 Acute injury in the anterior, anterolateral, and lateral wall (ST elevation in V2-V6, I and aVL). #2 Infarct in the antereoseptal and anterior wall (Q waves in V2-V4 there is also a probable inferior infarct (Q waves in II, III, and aVF)). #3 Ischemia across the entire anterior and lateral wall (T wave inversions in V2V6, I and aVL). Also note, the injury pattern in V2 of ST elevation, the prominent Q waves in V2 and V3 show that some of the myocardium has also reached the infarct stage Rate Rate is cycles or beats per minute. Normal rate for the SA node 60-100. <60 bradycardia >100 tachycardia SA node is the usual pacemaker, other potential pacemakers (if SA node fails) are atrial pacemakers with inherent rates of 60-80, AV node (rate 40-60), or ventricular pacer (rate 20-40). In certain pathologic conditions ectopic (out of place) pacemakers can go much faster at rates 150-250 cycles/minute. There are three methods of calculating rate: 1. Most Common Method: (Most rates can be calculated this way). Find an R wave on a heavy line (large box) count off "300, 150, 100, 75, 60, 50" for each large box you land on until you reach the next R wave. Estimate the rate if the second R wave doesn't fall on a heavy black line. Rate calculation Memorize the number sequence: 300, 150, 100, 75, 60, 50 1.Mathematical method: Use this method if there is a regular bradycardia, i.e. - rate < 50. If the distance between the two R waves is too long to use the common method, use the approach: 300/[# large boxes between two R waves]. : Count number of large boxes between first and second R waves=7.5. 300/7.5 large boxes = rate 40. 1.Six-second method: Count off 30 large boxes = 6 seconds (remember 1 large box = 0.2 seconds, so 30 large boxes = 6 seconds). Then, count the number of R-R intervals in six seconds and multiply by 10. This is the number of beats per minute. This is most useful if you have an irregular rhythm (like atrial fibrillation) when you want to know an average rate. Figure 6: Count 30 large boxes, starting from the first R wave. There are 8 R-R intervals within 30 boxes Concentrate on the rate for the following unknown tracings. #1 Rate The rate is about 90. The second R wave in the rhythm strip lands on a heavy line. Count "300-150100-75" over (four heavy lines) to the next R wave to determine the rate. You'll have to estimate between 75 and 100 for this example. #2 Rate ANSWER 2 The rate is about 40. Use the bradycardia method where 300 divided by the number of large boxes between R waves is the rate. In this case, there are 7.5 large boxes between R waves. 300 divided by 7.5 equals a rate of 40 #3 Rate ANSWER 3 Rate about 70-80. Use the six second strip method. There are 30 large boxes in six seconds. Multiply the number of R-R intervals in six seconds by ten to get the rate. Rhythm (to include intervals) We will focus on the basic "core" of rhythms and measured "intervals" (PR, QRS, QT). Rhythms are often the most challenging aspect of ECG's. You will see most rhythms several times over the next few years of your training, and you will eventually recognize them at a glance. Now for some basics - "arrhythmia" means abnormal rhythm. The normal conduction pathway is: SA node --> AV node --> Bundle of HIS --> Bundle Branches. Arrhythmia can be understood by realizing the existence of ectopic (out of place) foci (pacemakers) and understanding the normal conduction pathway of the heart. Very simply put, if the beat originates in the atria or AV node (supraventricular) the QRS is usually narrow (normal), because it comes from above along the normal pathway. Figure 6a: QRS is narrow (normal). If the beat is ventricular in origin, the QRS is wide and bizarre because it doesn't come down the normal pathway. Figure 6b: QRS is wide. Aberrancy is an exception to this rule - here it does actually follow the normal pathway (atria - AV node - ventricle) but for some reason the pathway is refractory to the beat and you get a wide QRS. A reasonable way to group arrhythmias is in four general groups. Let us briefly review these four groups, then we will develop some common sense principles for evaluating rhythm (to include intervals). Group 1 Irregular rhythms. (main clue is QRS is not spaced evenly apart anywhere, total irregularity of the beat). A) Sinus arrhythmia. P waves and P-R intervals are all identical because they originate from the sinus node. Sinus rate may vary normally a bit (increase with inspiration, decrease with expiration), but if the rate varies a lot, this term is used. Figure 7: Sinus arrhythmia: P waves are identical. B) Wandering atrial pacemaker. Pacemaker discharges from different atrial locations - the clue here is the P waves are of varying shape and differing PR intervals. PR interval is measured from the beginning of the the Pwave to the beginning of the QRS - if the atrial pacemaker location varies it will take different lengths of time to get to the ventricle - resulting in different PR intervals. If the rate of the wandering atrial pacemaker is >100 it is descriptively called multifocal atrial tachycardia. Figure 8: Multifocal atrial tachycardia. C) Atrial fibrillation. You will frequently see this arrhythmia. There are no P waves, only irregular or wavy baseline. The QRSs are irregularly spaced, therefore it is included under irregular rhythms. Figure 9: Atrial fibrillation. Group 2 Escape (late) beats and premature (early) beats. The bottom line for Group 2 arrhythmias is that the rhythm is fairly regular - then you will notice an early or late beat; try to figure out whether that beat is a premature atrial contraction, premature ventricular contraction, etc. A) Escape beats. The usual pacemaker fails, so a slower pacemaker fires at its inherent rate. Atrial escape Different appearing and late P wave. Figure 10: Atrial Escape Rhythm. Note differing appearance of the P waves for Sinus Rhythm vs. Atrial Escape Rhythm. Junctional escape No P wave, normal QRS if not aberrant. Figure 11: Note all beats are junctional escape Ventricular escape No P, wide, bizarre QRS. Figure 12: Ventricular escape. B) Premature Beats. An ectopic pacemaker fires early before the next scheduled beat. Premature atrial contraction "PAC", early and differently shaped P wave, narrow QRS. Figure 13: Premature Atrial Contraction noted by arrow. Premature junctional No P, normal QRS if not aberrant. Figure 14: Note the two early, narrow beats at the arrow. These are probably PJCs. Premature ventricular contraction No P, wide bizarre QRS. PVCs that occur three (3) or more in a row (ventricular tachycardia), multifocal PVCs (different shapes), or PVCs that land on a previous T wave (R on T phenomenon) can be dangerous ion a patient with underlying heart disease. Figure 15: Note: Every fourth beat is a PVC (beginning with the second beat). rhythms. Ectopic rate nomenclature: So, the descriptives paroxysmal tachycardia, flutter, and fibrillation refer to the "rates" of the arrhythmia, e.g. - it could be atrial fibrillation (wavy baseline refers to the atria going >350 bpm.), or ventricular fibrillation (with the ventricle not contracting in a coordinated fashion resulting in only an erratic line that isn't possible to count). [150-250] Paroxysmal tachycardia [250-350] Flutter [350+] Fibrillation So, the descriptives paroxysmal tachycardia, flutter, and fibrillation refer to the "rates" of the arrhythmia, e.g. - it could be atrial fibrillation (wavy baseline refers to the atria going >350 bpm.), or ventricular fibrillation (with the ventricle not contracting in a coordinated fashion resulting in only an erratic line that isn't possible to count). Figure 16: Paroxysmal supraventricular tachycardia: note accelerated rate and narrow QRS complexes. Figure 17: Ventricular tachycardia: note fast rate and wide bizarre QRS. Figure 18: Ventricular fibrillation: erratic and wavy baseline Group 4 Atrioventricular heart blocks. occur in three (3) degrees, like skin burns; third degree is the worst). 1st degree PR interval > 0.2 seconds (1 large box), each P is followed by a QRS. PR interval is measured from the beginning of the P wave to the beginning of the QRS. ( Figure 19: The PR interval is approximately 0.28 seconds. 2nd degree block - type 1 Also called "Wenkebach". PR interval gets progressively longer each beat until finally a QRS is "dropped" (missing). Figure 20: Note the increasing PR interval before the QRS is dropped, then the cycle is repeated. 2nd degree block - type 2 Also called "Mobitz II". Look out! A more serious conduction problem than Type 1. PR intervals are constant and a QRS is "dropped" intermittently. Figure 21: Note the dropped QRS after the second and sixth P wave in lead II (the rhythm strip). 3rd degree block The atrial rate is independent of the ventricular rate (P wave and QRS march out separately. The clue here is no relationship at all of the P-R intervals). The P-R interval is constantly changing, the QRS is usually wide and bizarre because it is ventricular origin. Figure 22: Note the P waves and QRS waves are independent of each other. Intervals An interval is a portion of the baseline and at least one wave. We measure an interval on the horizontal axis in seconds. The PR, QRS, and QT are the intervals which should be routinely scanned on each ECG. For measuring intervals, look at the widest form in any lead. 1.PR interval (beginning of P wave to the beginning of the next QRS). Normally, < .2 seconds or one large box. If it is > .2 seconds, it is a first degree block. (Note: this concept was introduced under blocks). Figure 24: Note the prolonged PR interval (.28 seconds), especially at the second beat QRS interval (beginning of Q to the end of the S wave) should be < .12 seconds (< 3 small boxes). If QRS is > .12, check for bundle branch block. A QRS > .12 and RR (2 peaks or R waves in QRS) occurring in the right chest leads (V1-V2) indicates a right bundle branch block. Figure 25: RBBB. If QRS is > .12 and RR occurs in the left chest leads (V5-V6), this indicates a left bundle branch block. Figure 26: LBBB. Very important: For left bundle branch block, the ECG is often unreliable for identifying infarct. Infarct is a concept explained later in this tutorial, but don't forget that with left bundle branch block, one cannot rely on the ECG for diagnosis of infarct. 1.QT interval (beginning of QRS to end of T wave) should be less than half of the preceding RR interval - this varies with the rate. For normal rates, QT < .4 seconds (2 large boxes). "QT prolongation" (too long) can lead to a refractory form of ventricular tachycardia called torsades de pointes. Figure 27: The QT interval is greater than half the preceding RR interval. Look at lead I. Rhythm Guidelines 1. Check the bottom of the rhythm strip for regularity, i.e. - is it completely regular, mostly regular with a few extra beats, or totally irregular? 2. Check for a P wave before each QRS, QRS after each P. 3. Check RR interval (for AV blocks) and QRS interval (for bundle branch blocks). Check for prolonged QT. 4. Continue to recognize "patterns" such as atrial fibrillation, PVCs, PACs, escape beats, ventricular tachycardia, paroxysmal atrial tachycardia, AV blocks and bundle branch blocks. Rhythm and Intervals Quiz: Question 1 Match the tracings with the correct interpretation: A. First Degree Block B. Sinus Arrhytmia C. Third Degree Block D. Atrial Fibrillation Rhythm and Intervals Quiz: Question 1 The correct matches are: C. Third Degree Block The atrial rate is independent of the ventricular rate so the P waves are independent of the QRS's. The P waves are regular and can be marched out with calipers. The same can be done with the QRS complexes. D. Atrial Fibrillation No P wave, irregular QRS with a wavy baseline. A. First Degree Block PR interval is greater than .2 seconds (one large box). Note that there is a P wave before each QRS and a QRS after each P wave. Rhythm and Intervals Quiz: Question 2 Match the tracings with the correct interpretation: A. Second Degree Block Type 1 B. PAC C. Second Degree Block Type 2 D. Paroxysmal Supraventricular Tachycardia Rhythm and Intervals Quiz: Question 2 The correct matches are: C. Second Degree Block Type 2 PR intervals are the same, but every other beat is dropped. D. Paroxysmal Supraventricular Tachycardia Regular narrow QRS. Often it's hard to determine whether it's atrial or junctional as it is going too fast to see P waves. Clinically it doesn't matter since they are treated the same. B. PAC The third beat is premature. It has a P wave of different morphology than the sinus beats. This defines it as a premature atrial contraction. Rhythm and Intervals Quiz: Question 3 Match the tracings with the correct interpretation: A. Ventricular Tachycardia B. Second Degree Block Type 1 (Wenckebach) C. Junctional Rhythm D. Wandering Atrial Pacemaker Rhythm and Intervals Quiz: Question 3 The correct matches are: D. Wandering Atrial Pacemaker (It's called Multi focal Atrial Tachycardia if the rate is >100). Strict definition is 3 different P wave morphologies and 3 different PR intervals. A. Ventricular Tachycardia Fast, wide, regular, bizarre QRS. B. Second Degree Block Type 1 (Wenckebach) The PR gets progressively longer until a beat is dropped. Rhythm and Intervals Quiz: Question 4 Match the tracings with the correct interpretation: A. Normal Sinus Rhythm B. Ventricular Fibrillation C. Sinus Arrhythmia D. Junctional Rhythm Rhythm and Intervals Quiz: Question 4 The correct matches are: A. Normal Sinus Rhythm Normal appearing P waves and QRS complexes. D. Junctional Rhythm Relatively narrow QRS, absence of P waves. C. Sinus Arrhythmia Irregular, but note P wave morphology and PR intervals are identical, this identiies it as a sinus rhythm. Rhythm and Intervals Quiz: Question 5 For the following two 12 lead ECGs verify that the QRS is prolonged in each. Which of the following 12 leads is a Right Bundle Branch Block and which is a Left Bundle Branch Block? Right Bundle Branch Block There is a RR' in V1 and V2 with a QRS greater than .12 seconds (three small boxes). You can measure the interval in the lead that shows the widest QRS. Also with right bundl branch block, the T wave is often affected (at least partially inverted) as part of the bundle branch block. Axis Direction of depolarization (vector) of the QRS complex. 1.The left ventricle is thicker so the mean QRS vector is down and to the left. (The origin of the vector is the AV node with the left ventricle being down and to the left of this). 2.The vector will point toward hypertrophy (thickened wall) and away from the infarct (electrically dead area). Figure 28: Axis nomenclature. Normal axis Left axis deviation Right axis deviation Indeterminate (extreme) axis deviation -30 to +90 degrees -30 to -90 degrees +90 to +/-180 degrees -90 to +/-180 degrees Since lead I and aVF are perpendicular to each other, you can use those two leads to quickly determine axis. Lead I runs from right to left across a patient's body, positive at the left hand:. If the QRS in lead I is positive (mainly above the baseline), the direction of depolarization will be in the positive half (right half) of the circle above. You can make a diagram and shade in the positive half of the circle. Lead aVF runs from top to bottom across a patient's body, positive at the feet. If the QRS in lead aVF is positive (mainly above the baseline), the direction of depolarization will be in the positive half (lower half) of the circle above. You can make a diagram and shade in the positive half of the circle: To find the axis overlap the two circles. The common shaded area is the quadrant in which the axis lies. In this example, the axis lies in the normal quadrant, which on a patient, points down and to the left. You can repeat this process for any two leads, but I and aVF are the classic places to look. If you realize that there are two leads to consider and a positive (+) or (-) orientation for each lead, there would be four possible combinations. Memorize the following axis guidelines. 1. Normal axis (0 to +90 degrees) Lead I Lead aVF Positive Positive 2. Left axis deviation (-30 to -90) Also check lead II. To be true left axis deviation, it should also be Positive down in lead II. If the QRS is upright in II, the axis is still normal (0 to -30). Negative 3. Right axis deviation (+90 to +180) Positive Negative 4. Indeterminate axis (-90 to -180) Negative Negative Normal axis. Left axis deviation Right axis deviation. The bottom line is, if the axis is shifted out of the normal quadrant, evaluate the reasons for this. Differential Diagnosis Left axis deviation LVH, left anterior fascicular block, inferior wall MI Right axis deviation RVH, left posterior fascicular block, lateral wall MI #1 Axis Normal Axis. Positive QRS in Lead I and aVF #3 Axis Left axis deviation. Positive QRS in lead I, but negative QRS in leads II and aVF. Right axis deviation. Positive QRS in lead aVF, but negative QRS in lead I. fascicular Blocks fascicular blocks are blocks of part of the left bundle, either the posterior or anterior division: : Divisions of the bundles. Anterior fascicular block - the most common. You will see left axis deviation (-30 to -90) and a small Q wave in lead I and an S in lead III (Q1S3). The QRS will be slightly prolonged (0.1 - 0.12 sec). Anterior fascicular block. Posterior fascicular block - less common. You will see right axis deviation, an S in lead I and an Q in lead III (S1Q3). The QRS will be slightly prolonged (0.1 - 0.12 sec). Posterior fascicular block. Bifascicular block. This means two (2) of the three (3) fascicles (in diagram) are blocked. The most important example is a right bundle branch block and a left anterior fascicular block. Watch out for this. Only one fascicle is left for conduction, and if that fasicle is intermittently blocked, the dangerous Mobitz 2 is set up! : Right bundle branch block and left anterior fascicular block. "fascicular Blocks" may seem a bit complicated simply remember that axis deviation is the clue. In your differential, consider posterior fascicular blocks with right axis deviation and consider anterior fascicular blocks with left axis deviation. Fascicular blocks cause axis deviations, like infarcts and hypertrophy. If you see a left or right axis deviation, first look for infarct or hypertrophy. If neither are present, the remaining diagnosis of fascicular block is usually correct. Review differential diagnosis of right and left axis deviation. #1 fascicular Block Left anterior fascicular block (left axis deviation and Q1S3). #2 fascicular Block Left posterior fascicular block (right axis deviation and S1Q3). #3 fascicular Block Bifascicular block RBBB and LAFB (right bundle branch block and left anterior fascicular block). One Last Differential Diagnosis Four cases of an R wave taller than an S wave in V1 (normally R wave always < S wave in V1. 1.Right bundle branch block. 2.Right ventricular hypertrophy. 3.Posterior wall myocardial infarction. 4.Wolff-Parkinson-White. Case 1 A 60-year-old "walk-in" patient without a primary care physician arrives at your clinic near the end of a busy afternoon clinic session. The patient is not on any medications and has not seen a physician in years. The patient complains of several hours of severe chest pressure and as he lives nearby he thought he would come to your clinic and try to see a physician. Although the vital signs were remarkable only for some bradycardia, the medical assistant is concerned that the patient appears ill. A stat ecg was done and you are asked to see this patient immediately. The following ecg is handed to you as you are on your way to see this patient. Case 1 Answer Rate - 50 Rhythm - sinus bradycardia Intervals - PR and QRS intervals are not prolonged Axis - normal Hypertrophy - none Infarct - acute injury pattern of ST elevation noted in V1-V4 Clinical correlation - An acute myocardial infarct can be one of the most dramatic emergencies in a primary care clinic and most seasoned practitioners have seen it on an occasional basis. With the severe chest pain and acute anterior injury pattern, this patient's situation is critical. Immediate medical stabilization is started and stat (911) telemetry transport to the emergency room is arranged. Case 2 A 55-year-old patient comes in to get your advice on starting a new exercise program to get back into shape. The program involves heavy aerobic workouts and he needs a form filled out that he is medically cleared to participate in this workout program. In talking to him you learn he has cardiac risk factors for smoking, positive family history, high cholesterol and hypertension. He has a sedentary lifestyle and has not participated in any strenuous physical activity for years. Although his cardiorespiratory review of systems is negative, you are concerned that his activity level is very limited and he has significant risk factors. As part of the workup you obtain the following ecg to interpret: Case 2 Answer Rate - about 70 Rhythm - sinus rhythm with borderline first degree block Intervals - PR is prolonged at .2 seconds, QRS is not prolonged Axis - normal quadrant Hypertrophy - left ventricular hypertrophy with strain pattern Infarct - Q waves noted in V2 and V3 consistent with old myocardial infarct in the anterior septal - anterior wall area Clinical correlation - This patient should NOT be medically cleared at this time. He has significant risk factors, a sedentary lifestyle and signs of previous infarction on ECG. He needs further cardiac evaluation and testing. Case 3 A 76-year-old patient, with a history of hypertension, comes to see you. She is currently on a diuretic prescription and is complaining of a few days of "skipped heart beats". She has felt slightly dizzy lately but does not have any other symptoms. Overall she has been feeling well, her only medical issue has been hypertension. Previous electrocardiograms in her chart show normal sinus rhythm and are otherwise unremarkable. Her exam shows an irregular pulse in the 130 rate range but the rest of the exam is unremarkable. You obtain the following electrocardiogram: Case 3 Answer Rate - about 130-150 range Rhythm - atrial fibrillation Intervals - no PR to measure, QRS is not prolonged Axis - normal quadrant (aVF is downward but lead II is upward) Hypertrophy - none Infarct - none (nonspecific ST changes in lateral leads I and aVL Clinical correlation - Atrial fibrillation is the most common sustained arrhythmia for which patients seek treatment. It is more common in the elderly and is a major cause of thromboembolic events. This patient will need a workup for the etiologies of atrial fibrillation and the usual therapeutic considerations of rate control, anticoagulation and antiarrhythmic therapy. Case 4 A 35-year-old man comes into your office as a new patient. He is concerned about his elevated blood pressure. A year ago, in a physicians office, he had a reading of 150/100. A month ago, while being evaluated for bronchitis at a walk-in clinic, his blood pressure was 150/105. At today's office visit his blood pressure is 155/105. He is asymptomatic and currently takes no medications. His cardiac exam is remarkable for a laterally displaced PMI and an S4. As part of the workup, you obtain the following electrocardiogram: Case 4 Answer Rate - about 100 Rhythm - normal sinus Intervals - no prolongation of the PR or QRS intervals Axis - normal quadrant Hypertrophy - left ventricle and left atrial Infarct - none Clinical correlation - This patient has three elevated blood pressure readings over different times and findings of an S4 with hypertrophy on an ecg. He now needs evaluation and treatment for hypertension. Case 5 A pleasant, 75-year-old, man with no significant past medical history, comes in with fatigue and feeling light headed. He denies any chest pain, current medication usage, or syncope. He has had to limit his physical activity since this fatigue started about a week ago. His vital signs are remarkable for a pulse of 40 and a blood pressure of 100/60 which he states is a bit low for him. Exam is unremarkable except for the bradycardia. Because of the bradycardia an electrocardiogram is ordered as part of the initial assessment. Case 5 Answer Rate -about 40 Rhythm - second degree block type 2 Intervals - prolonged qrs in V2 consistent with right bundle branch block Axis - left axis deviation from anterior fascicular block Hypertrophy - none Infarct - none Clinical correlation - This older patient has a bifascicular block combined with a Mobitz II block and this setting often antedates complete heart block. Etiologies include conduction system disease, drug effects, and myocardial ischemia. In this case the patient was admitted to the hospital with his symptomatci high degree block. Cardiac enzymes were negative for myocardial infarct and a cardiac pacemaker was inserted with excellent results - etilolgy was conduction system disease (presumed Lev's or Lenegre's disease). Case 6 A 65-year-old, female patient comes in for a get acquainted visit. She has a history of severe chronic obstructive pulmonary disease and is on multiple medications and home oxygen. During the physical she is noted to be tachycardic with an irregularly irregular pulse. An electrocardiogram is taken for further evaluation. Case 6 Answer Rate -varies from 110 to about 140 Rhythm - multifocal atrial tachycardia Intervals - differing PR intervals, QRS interval is not prolonged Axis - normal Hypertrophy - none Infarct - none Clinical correlation - By definition, MAT requires three or more consecutive P waves of different morphologies at rates greater than 100 beats per minute. Most patients have severe associated illnesses, especially COPD. Treatment of the underlying condition is the most effective approach. Atrial fibrillation and MAT are both irregularly irregular rhythms and a 12 lead ecg may be needed to tell them apart. It is clinically important to distinguish MAT from atrial fibrillation, as they are treated differently.