Public Health Care: Reform and Financing
advertisement

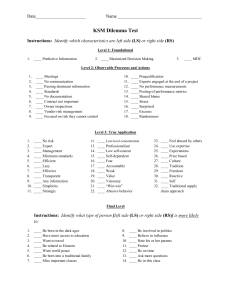
Evaluation of Health Care Financing Dr. Kyaw Swa Mya Lecturer/Head Environmental Health Department University of Community Health Outline of Presentation • Why health care financing? • Overview of health care financing • Evolution of health care financing at various stages of economic development • Criteria for evaluation of health care financing KSM, UOCH 2 Why is health care financing an important subject? • Health care is a basic necessity • Many poor cannot afford illness cost • Medical cost for treating serious illness are beyond the financial means of most households • Many households face bankruptcy when serious illness strikes KSM, UOCH 3 Philosophical Reason • Egalitarian philosophies – emphasizes equity, particularly equal access to health care and views health care as fundamental necessity for human well being • Utilitarian philosophies – views health in the context of how health contributes to a nation’s welfare KSM, UOCH 4 Policy Reason • The amount of financial resources mobilized for health care and how they are used depend on health care financing policy • Financing is the principle instrument with which to determine resource flows, distribution of resources, and incentive structures for health providers KSM, UOCH 5 Policy Reason • Unless a nation has a rational and integrated financing policy, the health care costs of elderly, disabled, and less healthy persons are left for the government to finance and the cost become a heavy financial burden on the treasury • Determine who will have access to basic health care, what services are offered, and their quality KSM, UOCH 6 Market Failure Reason • • • The distribution of health risks are highly skewed and it caused two serious market failures in private insurance market Adverse selection – high risk individual more likely to purchase insurance Risk selection – insurers exclude high risk individuals and only insure healthier persons for maximum profit KSM, UOCH 7 Macro-environmental Reason • Economic changes – reduction of government spending in public sector • Demographic changes – significant increase in the population as a whole and of those over age 60 • Epidemiological changes – double burden? Triple burden? • Political changes – increased demand and government supply KSM, UOCH 8 Six Building Blocks of a Health System Purposeful change aimed at improving health system performance for: System Inputs Source: Strengthening Health Systems to Improve Health Outcomes, WHO’s Framework for Action – WHO 2007 KSM, UOCH 9 Overview of HCF KSM, UOCH 10 HCF policy goals (WHO report, 2000) • • • • • • Financial protection Equity in finance Equity of access Transparency and accountability Quality care and efficient service delivery Administrative efficiency KSM, UOCH 11 Three basic principles for HCF • Principle 1 – Raise enough revenues to provide individuals with a basic package of essential services and financial protection against catastrophic medical expenses caused by illness and injury in an equitable, efficient, and sustainable manner • Principle 2 – Manage these revenues to pool health risks equitably and efficiently • Principle 3 – Ensure the purchase of health services in ways that are allocatively and technically efficient KSM, UOCH 12 Functions of HCF • Revenue collection • Polling resource • Purchasing services KSM, UOCH 13 Methods of HCF • Government revenue e.g. general tax, inflation, earmarked tax • Social and private insurance • User fees (OOPs) • Community financing KSM, UOCH 14 Exchange Model • Bilateral exchange model for goods Money Consumers Providers Service KSM, UOCH 15 Exchange Model • Trilateral Exchange Model for Goods Treasury Taxes Financing Organization Payments Premiums Services Consumers Providers User’s fee KSM, UOCH 16 Evolution of Health Care Financing at Various Stages of Economic Development Stage I (three tired system) Methods General revenue + donor Stage II Stage III Poor Low Segmented finance (Universal coverage) < $ 1,800 1,800 – 4,800 $ 5,000 – 12,000 $ > 12,000 $ Public health services NHS (UK, N.Z.) Public health, prevention Public health services (clinics, hospitals) (50-60%) Social insurance Medisave, Singapore (40-50%) (20-40%) For civil servant NHI (Canada) (10-20%) (30-60%) Bismarckian Negligible (5-10%) (15-40%) Medicare (USA) Self pay Self pay Private insurance Private hospitals & clinics Self pay (OOPs) Pharmacists Indigenous providers (35-45%) (20-40%) (15-25%) (15-25%) Bangladash Philippines Thailand USA, Singapore India Indonesia Malaysia Canada KSM, UOCH 18 Criteria for Evaluation of HCF • Equity – in financing - in provision of health care • Efficiency – in financing - in provision of health care • Other criteria – quality, sustainability, risk pooling KSM, UOCH 19 Definition of Health Equity • The International Society for Equity in Health (ISEqH) defined equity in health as “the absence of systematic and potentially remediable differences in one or more aspects of health across populations or population subgroups defined socially, economically, demographically, or geographically” KSM, UOCH 20 Difference of inequity and inequality • Health inequalities are differences in health that are “avoidable,” “unjust, and unfair” Whitehead 1990 KSM, UOCH 21 Determinants of Health Inqualities 1. Natural, biological variation 2. Differential health-damaging behavior that is freely chosen 3. Differential health-promoting behavior that is freely chosen 4. Differential health-damaging or health-promoting behavior, where choices are restricted 5. Differential exposure to unhealthy, stressful conditions (home, work, etc…) 6. Inadequate access to basic social and essential health services 7. Health-related social mobility KSM, UOCH Generally perceived as unavoidable or fair Generally perceived as avoidable or unfair 22 Vertical and horizontal equity • Horizontal equity applies to people in the same status or situation, and people who are alike should be treated in the same fashion, – in other words, equal treatment for equal need • Vertical equity focuses on the difference between individuals or groups of people, and people who are unlike in relevant respects (e.g. income, health needs), and states that the differences should be treated differently in a just way KSM, UOCH 23 How to measure equity? • • • • Lorenz curve Gini coefficient Kakwani index Concentration index KSM, UOCH 24 Lorenz Curve • Lorenz curve is a graphical representation of the proportionality of a distribution (the cumulative percentage of the values). It was developed by Max O. Lorenz in 1905 for representing income distribution KSM, UOCH 25 Lorenz Curve KSM, UOCH 26 Gini Coefficient Note: Gini Coefficient is a tool for measuring inequality of income. The value of Gini coefficient ranges from 0 to 1. A low Gini coefficient indicates more equal income or wealth distribution, while a high Gini coefficient demonstrates more unequal distribution. KSM, UOCH 27 Gini Coefficient KSM, UOCH 28 The Kakwani index • Is defined as twice the area between the concentration curve of health payment and the Lorenz curve of household income • The value of the Kakwani index ranges from -2 to 1 • A negative Kakwani index value indicates the regressive nature of health care payments • In contrast, a positive value indicates the progressive nature of health care payments KSM, UOCH 29 The Concentration Curve and Index • The concentration curve graphs on the x-axis the cumulative percentage of the sample ranked by living standards, beginning with the poorest, and on the y-axis the cumulative percentage of the health service use corresponding to each cumulative percentage of the distribution of the living standard variable • The concentration index is a means of quantifying the degree of income-related inequality within a specific health variable, for example, health service use, and government health subsidies KSM, UOCH 30 The concentration index • is defined as twice the area between the concentration curve and the line of equality (the 45-degree line running from the bottom-left corner to the top-right) • In the case where there is no income-related inequality, the concentration index is zero • The index takes a negative value when the concentration curve lies above the 45-degree line of equality, indicating disproportionate concentration of health service use or other health variables among the poor, and a positive value when it lies below the 45-degree line of equality KSM, UOCH 31 Equity in Health Care Financing Kakawani Index Concentration curve for health payment and lorenz curve for health expenditure, Egypt 1997 KSM, UOCH 33 Concentration curve for health payment and lorenz curve for health expenditure, Egypt 1997 KSM, UOCH 34 Progressive & Regressive result of previous figure • Kakawani index (direct tax) = 0.2501 • Kakawani index (indirect tax) = 0.1435 • Kakawani index (social insurance) = - 0.0532 • Kakawani index (OOPs) = 0.0644 KSM, UOCH 35 Trends of Kakawani indices of HCF Methods in Thailand (1986 – 1998) 0.4 0.3 0.2911 0.2479 0.2545 0.2 0.2546 0.2309 0.2372 0.2269 0.1 0 -0.064 -0.1 -0.2 -0.3 -0.1322 -0.2273 -0.0362 -0.0667 -0.1019 -0.1911 -0.2327 -0.1787 -0.2317 -0.1635 -0.238 -0.2044 -0.2227 -0.3176 -0.0972 -0.108 -0.1507 -0.2406 -0.2515 -0.254 -0.4 1986-1988-1990-1992-1994-1996-1998 Direct indirect Both direct & indirect KSM, UOCH OOPs 36 Progressivity of HCF KSM, UOCH 37 Equity in Provision of Health Care Concentration Index Selected concentration curves of ambulatory service use among different types of health facilities in 2003 KSM, UOCH 39 Selected concentration curves of ambulatory service use among different types of health facilities in 2003 KSM, UOCH 40 Selected concentration curves of ambulatory service use among different types of health facilities in 2003 KSM, UOCH 41 Selected concentration curves of ambulatory service use among different types of health facilities in 2003 KSM, UOCH 42 Concentration curve for health sector subsidies and lorenz curve of household consumption, Egypt 1997 KSM, UOCH 43 Regressive result of previous figure • • • • Kakawani index (inpatient) = - 0.1785 Kakawani index (outpatient) = - 0.1069 Kakawani index (health centre) = - 0.4797 Kakawani index (total subsidy) = - 0.2124 KSM, UOCH 44 Efficiency in Health Care Financing and Provision of Health Efficiency Measures Overview It is organized in three tiers 1. Perspective Function of Health system esp in Health Care Financing 2. Output Revenue collection, risk pooling, purchasing 3. Type of Efficiency Allocative, Technical/ Productive and Social Efficiency KSM, UOCH 46 Efficiency Overview Perspective Society Health Care Financing Health Plans Providers Purchasers Type Output Individuals Revenue collection, Risk pooling Technical Productive KSM, UOCH Purchasing Social 47 Allocative Efficiency A firm achieves technical efficiency when it cannot produce the same output with any fewer inputs KSM, UOCH 48 Technical/Productive Efficiency A firm achieves productive efficiency when it cannot produce the same output at a lower cost KSM, UOCH 49 Social efficiency • Social efficiency is more often the focus for society than for firms and mainly consider for social inclusion • No person can be better off without making somebody worse off (Pareto optimality) KSM, UOCH 50 Public Finance Challenge Pure Private Goods Cosmetic surgery Open heart surgery Curative Kidney dialysis VIP IP care 2nd class IP care OP hospital self-referrals OP hospital referrals Health center OP curative Family Planning Actual funding ends up here Maternal and Child Health Preventive Poor Vector control Environmental sanitation Water supply Rich Pure Public Goods KSM, UOCH Government policy dictates most resources flow here 51 Financing: Filling the gaps Pure Private Goods Curative Public / private collaboration in curative service delivery Self- Subsidized pre-pmt Schemes Preventive financing Pre-pmt Schemes Pure private provision + service contracts SHI - public/private provision Public provision & finance The poor The rich Pure Public Goods KSM, UOCH 52 References • Andres Vork et. al, 2010. Income related inequality in health care financing and utilization in Estonia since 2000. WHO health financing paper 2010/3 • Innovative Medicine South Africa, 2009. National health insurance Background brief: Understanding Health Care Financing • Mara Brain, 2008. Public Health Care: Reform and financing, A big picture • Owen O’donnel et. al, 2008. Analyzing health equity by using household survey data: A guide to techniques and their implimentations KSM, UOCH 53 References (Contd) • Pablo Gottret & George Schieber, 2006. Health financing revisited: A practitioner’s guide • Supasit Pannarunothai and Direk Patmasiriwat, 2000. Equity-directed health care reform in Thailand: The use of macroeconomic indices • The alliance, 2006. Efficiency in Health Care: What does it mean? How is it measured? How can it be used for valued based purchasing? • WHO, 2007. Strengthening Health System to improve Health Outcomes: WHO’s framework for action • William Hsiao, 2000. Health care financing in developing nations KSM, UOCH 54 KSM, UOCH 55