Higher Human Biology unit 2 section 5 DIABETES
advertisement

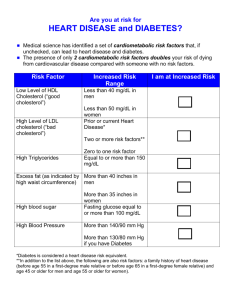
Cardiovascular Disease, Diabetes and Obesity • (c) Pathology of cardio vascular disease (CVD). • (i) Process of atherosclerosis, its effect on arteries and blood pressure and its link to cardiovascular diseases (CVD). Atherosclerosis Contributing factors to the development of atherosclerosis • High blood pressure • Carbon monoxide in cigarettes • Diabetes • High blood cholesterol levels Hypertension (high blood pressure) • Hypertension is a major risk factor for many diseases including coronary heart disease. Of hearts and hypertension film • http://www.hhmi.org/biointeractive/hearts-and-hypertensionblazing-genetic-trails Consequences • Atherosclerosis is the root cause of various cardio vascular diseases including • • • • angina heart attack stroke peripheral vascular disease Atherosclerosis • Atherosclerosis is the accumulation of fatty material (consisting mainly of cholesterol), fibrous material and calcium forming an atheroma, also known as a plaque, beneath the endothelium. As the atheroma grows the artery thickens and loses its elasticity. The diameter of the artery becomes reduced and blood flow becomes restricted resulting in increased blood pressure. • Atherosclerosis is the root cause of various cardio vascular diseases including angina, heart attack, stroke and peripheral vascular disease. • Examine league tables for coronary heart disease worldwide. • Examine trends in coronary heart disease over last 10 years. • (ii) Thrombosis— Events leading to a myocardial infarction (MI) or stroke. • Endothelium damage, clotting factors and the role of prothrombin, thrombin, fibrinogen and fibrin. Thrombus formation and effects of an embolus. Thrombosis THROMBOSIS • A thrombus is a blood clot that forms inside a blood vessel or cavity of the heart. • Thrombosis is the formation or presence of a blood clot inside a blood vessel or the heart. Thrombosis Clotting of Blood • a) Damaged endothelial cells cells release a group of proteins called clotting factors. These clotting factors are released into the plasma at a wound site. • b) Clotting factors activate the enzyme Thrombin from its inactive form to prothrombin c) Thrombin turns the soluble plasma protein fibrinogen into its insoluble fibrous form Fibrin. • d) The fibrin threads form a meshwork that clots the blood by binding platelets and blood cells to form a ‘plug’ (clot) to seal the wound and provide a scaffold for the formation of scar tissue. Thrombosis • Atheromas may rupture damaging the endothelium. The damage releases clotting factors that activate the conversion of the enzyme prothrombin to its active form thrombin. Thrombin then causes molecules of the plasma protein fibrinogen to form threads of fibrin. The fibrin threads form a meshwork that clots the blood, seals the wound and provides a scaffold for the formation of scar tissue. • The formation of a clot (thrombus) is referred to as thrombosis. If the thrombus breaks loose from the site of formation (embolus), it travels along the blood stream until it reaches an artery too narrow to allow it to get through. Stroke A stroke means that the blood supply to a part of the brain is suddenly cut off. The brain cells need a constant supply of oxygen from the blood. Soon after the blood supply is cut off, the cells in the affected area of the brain become damaged or die. Myocardial Infarction (Heart Attack or Coronary Thrombosis) Clot stops flow of blood Plaque build-up on vessel walls Where the blockage occurs in the artery Where the heart is affected Myocardial infraction • In some cases a thrombus may break loose forming an embolus and travel through the bloodstream until it blocks a blood vessel. A thrombosis in a coronary artery may lead to a heart attack (MI). A thrombosis in an artery in the brain may lead to a stroke. Either way, cells are deprived of oxygen, leading to death of the tissues. • Investigate the use of thrombolytic medications such as streptokinase and tissue plasminogen activator. • Compare and contrast the use of antiplatelet and anticoagulants therapies. • Investigate examples of bleeding disorders such as Von Willebrand disease and haemophilia A, B and C. • (iii) Causes of peripheral vascular disorders including narrowing of arteries due to atherosclerosis, deep vein thrombosis (DVT) and pulmonary embolism due to blood clots. Peripheral Vascular Disorders Peripheral Vascular Disease • Caused by narrowing of the arteries other than those of the heart or brain • A DVT is a blood clot that forms in a deep vein (most commonly in the leg) and can break off and result in a pulmonary embolism. Peripheral vascular disease • Peripheral vascular disease is narrowing of the arteries due to atherosclerosis of arteries other than those of the heart or brain. The arteries to the legs are most commonly affected. Pain is experienced in the leg muscles due to a limited supply of oxygen. • A Deep Vein Thrombosis (DVT) is a blood clot that forms in a deep vein most commonly in the leg, and can break off and result in a pulmonary embolism if it travels to a blood vessel supplying the lungs. • (iv) Control of cholesterol levels and familial hypercholesterolaemia. • Cholesterol synthesis and its function in the cell membrane and in steroid synthesis. • Roles of high density lipoproteins (HDL) and low density lipoproteins (LDL). LDL receptors, negative feedback control and atheroma formation. Ratios of HDL to LDL in maintaining health, the benefits of physical activity and a low fat diet. Reducing blood cholesterol through prescribed medications. Control of Cholesterol Levels Cholesterol facts • Found in the diet – eggs, dairy etc • Made up of lipids, component of the cell membrane and required for steroid synthesis • Removed by the liver • 2 types of cholesterol carrying proteins in the blood: 1. High density lipoproteins (HDL) 2. Low density lipoproteins (LDL) HDL transports excess cholesterol from the body cells to the liver for elimination. This prevents accumulation of cholesterol in the blood. A higher ratio of HDL to LDL will result in lower blood cholesterol and a reduced chance of atherosclerosis. Cholesterol • Most cholesterol is synthesised by the liver from saturated fats in the diet. Cholesterol is a component of cell membranes and needed for steroid synthesis. There are two types of cholesterol carrying proteins: 1. High density lipoproteins (HDL) 2. Low density lipoproteins (LDL) • HDL transport excess cholesterol from the body cells to the liver for elimination. This prevents accumulation of cholesterol in the blood. A higher ratio of HDL to LDL will result in lower blood cholesterol and a reduced chance of atherosclerosis. • Once a cell has sufficient cholesterol, a negative feedback system inhibits the synthesis of new LDL receptors and LDL circulates in the blood where it may deposit cholesterol in the arteries forming atheromas. Cholesterol • LDL transports cholesterol to body cells. Most cells have LDL receptors that take LDL into the cell where it releases cholesterol. Once a cell has sufficient cholesterol a negative feedback system inhibits the synthesis of new LDL receptors and LDL circulates in the blood where it may deposit cholesterol in the arteries forming atheromas. • Research data on the action of cholesterol reducing drugs. • Investigate current views on the use of statins in treatment of patients at risk of CVD. Lowering Cholesterol Levels • Regular physical activity tends to raise HDL levels • Dietary changes aim to reduce the levels of total fat in the diet and to replace saturated with unsaturated fats. • Drugs such as statins reduce blood cholesterol by inhibiting the synthesis of cholesterol by liver cells. Reducing cholesterol • Regular exercise tends to raise HDL levels, removing more cholesterol from the blood. • Dietary changes aim to reduce the levels of total fat in the diet and to replace saturated with unsaturated fats. • Drugs such as statins reduce blood cholesterol by inhibiting the synthesis of cholesterol by liver cells. • Genetic screening of familial hypercholesterolaemia (FH) and its treatments. Familial Hypercholesterolaemia Familial Hypercholesterolaemia Families, inherited High levels cholesterol a condition • Familial hypercholesterolaemia (FH) is due to an autosomal dominant gene which predisposes individuals to developing high levels of cholesterol. • FH genes cause a reduction in the number of LDL receptors or an altered receptor structure. • Genetic testing can determine if the FH gene has been inherited and it can be treated with lifestyle modification (see reducing cholesterol) and drugs. • Cell receptors and the role of hormones in negative feedback control of blood glucose through insulin, glucagon and adrenaline (epinephrine). Regulation of Blood Glucose Levels Blood Glucose Regulation ‘Fight or Flight’ situation. • The adrenal glands secrete the hormone adrenaline (epinephrine). • Promotes glycogen breakdown in liver • Inhibits insulin secretion Blood glucose regulation • Receptors in the pancreas respond to high blood glucose levels by producing insulin which activates the conversion of glucose to glycogen in the liver and so decreases blood glucose concentration. • Receptors also respond to low blood glucose levels by producing glucagon which activates the conversion of glycogen to glucose in the liver and so increases blood glucose level. • During exercise and ‘fight or flight’ responses, glucose levels are raised by adrenaline (epinephrine) released from the adrenal glands which stimulate glucagon secretion and inhibit insulin secretion. • • Regulating blood glucose levels animation: • http://www.abpischools.org.uk/page/modules/diabetes_16plus/diab etes3.cfm?coSiteNavigation_allTopic=1 Diagnosing diabetes • The glucose tolerance test is used to diagnose diabetes. The blood glucose levels of the individual are measured after fasting and two hours after drinking 250–300 ml of glucose solution. Glucose Tolerance Test Hormone effects on organs animation • http://www.abpischools.org.uk/page/modules/diabetes_16plus/diab etes3.cfm?coSiteNavigation_allTopic=1 • Drag and drop quiz at bottom Diabetes The glucose tolerance test measures how quickly blood glucose levels return to normal after fasting then and two hours after drinking 250-300ml of glucose solution. In both types of diabetes individual blood glucose levels will rise rapidly after a meal. The kidneys are unable to cope resulting in glucose being lost in the urine. Testing urine for glucose is often used as an indicator of diabetes. • Diagnosis, treatments and role of insulin in type 1 and type 2 diabetes. Type 1 and Type 2 Diabetes Symptoms of Diabetes Mellitus Classic symptoms of diabetes are – • Frequent urination, with large volumes of urine (especially at night) • Excessive thirst • Hunger • Weight loss Other symptoms – • Fatigue • Blurry vision • Gum and urinary tract infections • Slow healing of skin Diabetes UK • Diabetes film • http://www.diabetes.org.uk/Guide-to-diabetes/What-is-diabetes/ Type 1 diabetes • NHS film • http://www.nhs.uk/Conditions/Diabetestype1/Pages/Introduction.aspx • Chandler’s story Type 1 Diabetes • Type 1- usually occurs in childhood. • A person with type 1 diabetes is unable to produce insulin and can be treated with regular doses of insulin Type 2 diabetes • Risk calculator: • www.nhs.uk/Conditions/Diabetes-type2/Pages/Introduction.aspx Type 2 Diabetes • Type 2 diabetes or adult onset diabetes develops later in life and occurs mainly in overweight individuals. • Type 2 diabetics produce insulin but their cells are less sensitive to it. • This insulin resistance is linked to a decrease in the number of insulin receptors in the liver • This leads to a failure to convert glucose to glycogen. Type 1 and 2 diabetes Read diabetes articles Gene therapy to diabetic treatment • 2 short videos: • http://www.abpischools.org.uk/page/modules/diabetes_16plus/diab etes9.cfm?coSiteNavigation_allTopic=1 Diabetes • Type 1 diabetes usually occurs in childhood. Type 1 diabetics are unable to produce insulin and can be treated with regular doses of insulin injections. • Type 2 diabetes or adult onset diabetes typically develops later in life and occurs mainly in overweight individuals. Type 2 diabetics produce insulin but their cells are less sensitive to it. This insulin resistance is linked to a decrease in the number of insulin receptors in the liver leading to a failure to convert glucose to glycogen. Treatment involves a low sugar diet, regular exercise and decreasing calories within the diet to reduce any obesity. • (v) Blood glucose levels • Chronic elevated blood glucose levels leads to atherosclerosis and blood vessel damage. Blood Glucose levels, Atherosclerosis and Blood Vessel Damage Complications Associated with Diabetes • Nerve damage • Vascular disease can be caused by chronic diabetes • • • • • Hypertension Stroke Kidney disease Increased risk of atherosclerosis Impaired vision due to cataracts or damaged retinas. • Elevated blood glucose levels cause the endothelial cells lining the blood vessels to absorb more glucose than normal • This cause damage to the blood vessels BLEEDING (THE RED BLOTS) FROM BLOOD VESSEL WALLSvascular DUE TO • Can leadWEAK to peripheral disease, DIABETES CVD or stroke • Small blood vessels damaged by elevated glucose levels may result in haemorrhage of blood vessels in the retina, renal failure or peripheral nerve dysfunction • Investigate the symptoms associated with ‘microvascular disease’ and ‘macrovascular’. Diabetic ulceration Blood glucose levels Chronic (long term) elevation of blood glucose levels leads to the endothelium cells taking in more glucose than normal which damages the blood vessels. Atherosclerosis may develop leading to cardio vascular disease, stroke or peripheral vascular disease. Small blood vessels damaged by elevated glucose levels may result in haemorrhage of blood vessels in the retina, renal failure or peripheral nerve dysfunction. Diabetes ABPI schools • Hormones drag and drop exercise: • http://www.abpischools.org.uk/page/modules/hormones/horm10.cf m?coSiteNavigation_allTopic=1 ABPI schools • Diabetes quiz questions: • http://www.abpischools.org.uk/page/modules/diabetes_16plus/diab etes2.cfm?coSiteNavigation_allTopic=1 • And http://www.abpischools.org.uk/page/modules/diabetes_16plus/diab etes10.cfm?coSiteNavigation_allTopic=1 • (vi) Obesity linked to cardiovascular disease and diabetes. • Definition and characterisation of obesity. Body fat, body density measurements and BMI calculations. Role of exercise in reducing CVD. • Compare measurement of body composition using different methods. For example using densitometry, skin fold thicknesses, bioelectrical impedance, waist-hip ratio and body mass index. • Perform simple measurements of body composition. • Analyse data which illustrates the effect of exercise on body composition. • Examine case histories using coronary heart disease risk calculators (eg Framingham index). • Examine risk factors and remedial measures in treating cardiovascular disease. Obesity -Cardiovascular Disease and Diabetes Obesity-Risk Factor • Obesity is a major risk factor for cardiovascular disease and type 2 diabetes Obesity • Body mass index (BMI) is a simple index commonly used to classify overweight and obesity in adults. • Body mass index greater than 30 is used to indicate obesity. Body Mass Index (BMI) Classification BMI (kg/m2) Associated health risks Underweight Less than 18.5 Low Normal 18.5 - 24.9 Average Overweight Moderate Obese class 1 Obese class 2 Obese class 3 Greater than 25.0 25.0 – 29.9 30.0 – 34.9 35.0 – 39.9 Greater than 40.0 Increased Moderate increase. Severe increase. Very severe increase. Disadvantage of Calculating BMI • Classification by BMI may result in an individual being classified as overweight or obese, when in fact they have a relatively low percentage body fat but a large bone mass or muscle bulk. • Eg. – body builders Densitometry • An accurate measurement of body fat requires the measurement of body density • Densitometry depends on the fact that fat is less dense than lean tissue • Measurement of body density by underwater weighing • Density= body mass(g) body volume(cm³) • Percentage body fat can then be calculated Obesity • Obesity is a major risk factor for cardiovascular disease and type 2 diabetes. Obesity is characterised by excess body fat in relation to muscle tissue. • A body mass index (BMI) is used to estimate levels of obesity. BMI = • A BMI over 30 is used to indicate obesity. Accurate measurement of body fat requires the measurement of body density. • Skin fold thickness measurements can indicate skin fat levels by using callipers. Treatment of Obesity • Limit fats and free sugars in diet • Fats have a high calorific value • Free sugars need no metabolic energy to be expended to digest them. • Free sugars include monosaccharides and disaccharides that are added to foods and sugars naturally present in honey, syrups, fruit juices and fruit concentrates Why Exercise? • Exercise increases energy expenditure • It preserve lean tissue • Exercise can help to reduce the risk factors for CVD by • • • • keeping weight under control Minimising stress Reducing hypertension Improving HDL blood lipid profiles Obesity • Obesity is linked to high fat diets and a decrease in physical activity. The energy intake in the diet should limit fats as fats have a high number of calories per gram. Energy intake should also limit free sugars as they require no metabolic energy to be expended in their digestion. • Exercise increases energy expenditure and preserves lean tissue. It can help to reduce risk factors for CVD by keeping weight under control, minimising stress, reducing hypertension (high blood pressure) and improving HDL levels in the blood.