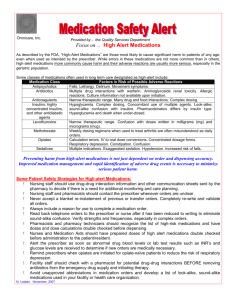
High Alert Medications
advertisement

Presented by : Abdulhadi Burzangi Pharm.D Introduction • all hospital’s pharmacy still complainhng of medications errors problems which lead to increasing number of patients die until now…. • The research for the methods or ways to reduce these medications errors is a great challenge… • So…we must know more information about medications that consider as High Alert Medications and how to deal with them? Key points • • • • • Definition. High alert medications. The top five high-alert medications. Reduce the risks of high-alert drugs. Safeguards for the use of high alert medications. I. Definition • High Alert Medications : Drugs that bear a heightened risk of causing significant patient harm when they are used in error. Although mistakes may or may not be more common with these drugs, the consequences of an error are clearly more devastating to patients. II. High Alert Medications Classes/Categories of Medications Adrenergic agonists I.V (e.g, epinephrine, phenylephrine, norepinephrine ). Adrenergic antagonists I.V ( e.g, propranolol, metoprolol, labetalol ) Anasthetic agents: inhaled and IV ( e.g, propofol, ketamine ) Antiarrhythmics, I.V ( e.g, lidocaine, amiodarone ). Anticoagulant : (e.g, heparin, warfarin ). Chemotherapeutic agents : parentral and oral. Oral hypogylcemics. Inotropic medications I.V ( e.g, digoxin , milrinone ). Moderate sedation agents I.V (e.g, midazolam), Oral (e.g, chloral hydrate) Narcotics/Opiates I.V, transdermal and oral. Neuromuscular blocking agents ( e.g, succinylcholine). Cont.. Specific medications Colchicine injection . Insulin : S.C and I.V. Magnesium sulfate injection. Methotrexate : oral ( non – oncologic use ) . Oxyticin I.V. Nitroprusside sodium for injection. Potassium chloride for injection . Promethazine I.V. Sodium chloride for injection. III. The top five high-alert medications 1- Insulin. 2- Opiate and Narcotics. 3- Injectable Potassium chloride or phosphate. 4- Injectable Anticoagulant. 5- Sodium chloride solution above 0.9%. III. The top five high-alert medications 1- Insulin • Hypoglycemia is the most common complication of any insulin therapy. • Factors contributing to harm : - Complexity of dosing. - Frequent monitoring. - Pharmacokinetics differ based on insulin type. Cont.. - Many insulin products available : ( look alike – sound alike names ) - Lack of dose check systems - Insulin and heparin vials kept in close proximity to each other on a nursing unit, leading to mix-ups. - Use of "U" as an abbreviation for "units" in orders (which can be confused with "O," resulting in a 10-fold overdose) - Incorrect rates being programmed into an infusion pump. 2- Opiates and Narcotics Cont.. Factors contributing to harm : • Calculation errors. • IV to PO conversion errors. • Errors converting potency when changing from one narcotic to another. • Many dosage forms. Cont.. - Parenteral narcotics stored in nursing areas as floor stock. - Confusion between hydromorphone and morphine. - Patient-controlled analgesia (PCA) errors regarding concentration and rate. • Adverse effet : - Respiratory depression - Confusion - Lethargy Cont.. 3- Injectable Potassium Chloride or Phosphate • Common Risk Factors - Storing concentrated potassium chloride/phosphate outside of the pharmacy. - Requests for unusual concentrations. Adverse effect : 1- Muscular or respiratory paralysis. 2- Mental confusion. 3- Hypotension. 4- Cardiac arrhythmia. 5- Heart block. Cont.. Cont.. 4- Injectable anticoagulant ( Heparin ) Common Risk Factors • Narrow therapeutic range. • • • • Complex dosing. Frequent monitoring. Patient compliance. Many interaction : – – – – Other prescription medication. OTC medications. Herbal products. Food. Cont.. • Common Risk Factors - Unclear labeling regarding concentration and total volume. - Multi-dose containers. - Confusion between heparin and insulin due to similar measurement units. Cont.. 5- Sodium chloride solution above 0.9% • Common Risk Factors - Storing sodium chloride solutions (above 0.9%) on nursing units. - Large number of concentrations/formulations available. - No double check system in place. IV. Reduce the risks of high-alert drugs • Three formulas: 1. Standardize error-prevention processes. 2. Make errors apparent. 3. Minimize the consequences of errors that reach the patient. 1. Standardize error-prevention processes Cont.. • Technological aids: 1- Computerized prescriber order entry (CPOE) 2- Bar coding • Make patient information readily accessible: 2. Make errors apparent Cont.. a. Perform independent double checks b. Rely on redundancies. c. Listen for bells and whistles. Cont.. a. Perform independent double checks • Have another person verify the medication order and infusion pump setting : – just before you start an infusion. – every time you change an infusion rate. – every time you replace an empty infusion bag or cassette. • Use this method exclusively for high-alert drugs to avoid double-check fatigue and complacency. b. Rely on redundancies Cont.. • Match high-alert drug orders to the patient’s diagnosis, the drug’s indication, and vital patient information. • If possible, avoid verbal orders. If they’re necessary, write down the order in the chart and then read back: – patient name – drug order as written – spelling of the drug name 3. Minimize consequences of errors Cont.. A. Closely monitoring the patient’s - level of consciousness - vital signs - respiratory status - lab results B. Ensuring that reversal agents and resuscitation equipment are readily available V. Safeguards for the use of high alert medications - Removal high concentrate electrolytes (e.g. potassium chloride, potassium phosphate and sodium chloride) from all nursing units. - Stop using dangerous abbreviations such as “u”. - Use of a leading zero before a decimal place. - Review the hospital formulary for sound-alike and look-alike medications. Cont.. - Use of “tall man” letters for sound-alike and look-alike names (e.g. DOBUTamine and DOPamine). - Careful review of how products are arranged on shelves to avoid similar packaged or sound-alike medications being side by side. - Use flow-control pumps for continuous intravenous (I.V.) infusions. - Educate patients and family and encourage their participation in care. Conclusion - Use of visible coloured auxiliary warning labels. • I wish to apply this procedure in this hospital. References • 5 Million Lives Campaign Getting Started Kit: Prevent Harm from High-Alert Medications How-to Guide. Institute for Healthcare Improvement, 2007. • http://www.ismp.org/newsletters/acutecare/articles/ 20070517.asp