Objectives - Anatomy and Physiology
advertisement

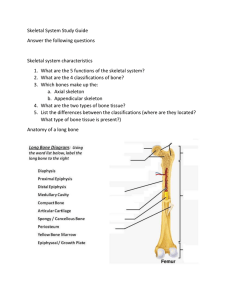
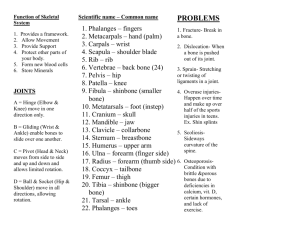
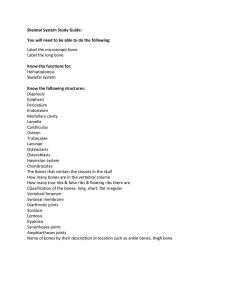
Exam 2 Review Sheet 4: Tissue: The Living Fabric Objectives Preparing Human Tissue for Microscopy 1. List the steps involved in preparing animal tissue for microscopic viewing. Epithelial Tissue 2. List several structural and functional characteristics of epithelial tissue. 3. Name, classify, and describe the various types of epithelia, and indicate their chief function(s) and location(s). 4. Define gland. 5. Differentiate between exocrine and endocrine glands, and between multicellular and unicellular glands. 6. Describe how multicellular exocrine glands are classified structurally and functionally. Outline Preparing Human Tissue for Microscopy (pp. 114–115) A. Tissue specimens must be fixed (preserved) and sectioned (sliced) thinly enough to allow light transmission. B. Tissue sections must be stained with dyes that bind to different parts of the cell in slightly different ways so that anatomical structures are distinguished from one another. Epithelial Tissue (pp. 115–124; Figs. 4.1–4.6) A. Features of Epithelia (p. 115) 1. An epithelium is a sheet of cells that covers a body surface or lines a cavity. 2. Epithelium occurs in the body as covering or lining epithelium, and as glandular epithelium. B. Special Characteristics of Epithelium (pp. 115–116) 1. Composed of closely packed cells with little extracellular material between. 2. Adjacent epithelial cells are bound together by specialized contacts such as desmosomes and tight junctions. 3. Exhibits polarity by having an apical surface (free) and a basal surface (attached). 4. Supported by the underlying connective tissue. 5. Innervated but avascular. 6. Has a high regeneration capacity. C. Classification of Epithelia (pp. 116–121; Figs. 4.1–4.3) 1. Each epithelial tissue is given two names. a. The first name indicates the number of layers present, either simple (one) or stratified (more than one). b. The second name describes the shape of the cells. 2. Simple epithelia are mostly concerned with absorption, secretion, and filtration. a. Simple squamous epithelium is a single layer of fish scale–shaped cells. b. Simple cuboidal epithelium is a single layer of cube-shaped cells forming the smallest ducts of glands and many kidney tubules. c. Simple columnar epithelium is a single layer of column-shaped cells that line the digestive tract. d. Pseudostratified columnar epithelium contains cells of varying heights giving the false impression of the presence of many layers. 3. Stratified epithelia’s main function is protection. a. Stratified squamous epithelium is composed of several layers with the cells on the free surface being squamous shaped and the underlying cells being cuboidal or columnar in shape. b. Stratified cuboidal epithelium is rare, found mostly in the ducts of some of the larger glands. c. Stratified columnar epithelium is found in limited distribution with small amounts in the pharynx, in the male urethra, and lining some glandular ducts. d. Transitional epithelium forms the lining of the hollow organs of the urinary system that stretches as they fill. D. Glandular Epithelia (pp. 121–124; Figs.4.4–4.6) 1. Endocrine glands are ductless glands that secrete hormones by exocytosis directly into the blood or lymph. 2. Exocrine glands have ducts and secrete their product onto a surface or into body cavities. a. Exocrine glands may be unicellular or multicellular. b. Exocrine secretions in humans may be merocrine, which are products released through exocytosis, or holocrine, which are synthesized products released when the cell ruptures. Tissue Repair (pp. 138–141; Fig. 4.12) A. Tissue repair occurs in two ways: regeneration and fibrosis (p. 138). B. Three steps are involved in the tissue repair process (pp. 139–140; Fig. 4.12). 1. Inflammation prepares the area for the repair process. 2. Organization restores the blood supply. 3. Regeneration and fibrosis effect permanent repair. C. The generative capacity of tissues varies widely among the tissue types (pp. 140–141). Developmental Aspects of Tissues (pp. 141, 144; Fig. 4.13) A. Embryonic and Fetal Development of Tissues (pp. 141, 144; Fig. 4.13) 1. Primary germ layer formation is one of the first events of embryonic development. a. Ectoderm is the most superficial of the layers. b. Mesoderm is the middle layer. c. Endoderm is the deepest layer. 2. The primary germ layers specialize to form the four primary tissues. B. With increasing age, epithelia become thin, the amount of collagen fibers in the body decreases, and bone, muscle, and nervous tissue atrophy (p. 144). 5: The Integumentary System Objectives Functions of the Integumentary System Describe how the skin accomplishes at least five different functions. Homeostatic Imbalances of Skin Explain why serious burns are life threatening. Describe how to determine the extent of a burn and differentiate first-, second-, and third-degree burns. Summarize the characteristics of the three major types of skin cancers. Developmental Aspects of the Integumentary System Describe and attempt to explain the causes of changes that occur in the skin from birth to old age. Outline Functions of the Integumentary System (pp. 160–162) A. Protection (pp. 160–161) 1. Chemical barriers include skin secretions and melanin. 2. Physical or mechanical barriers are provided by the continuity of the skin, and the hardness of the keratinized cells. 3. Biological barriers include the epidermal dendritic cells, the macrophages of the dermis, and the DNA itself. B. The skin plays an important role in body temperature regulation by using the sweat glands of the skin to cool the body, and constriction of dermal capillaries to prevent heat loss (p. 161). C. Cutaneous sensation is made possible by the placement of cutaneous sensory receptors, which are part of the nervous system, in the layers of the skin (p. 161). D. The skin provides the metabolic function of making vitamin D when it is exposed to sunlight (p. 161). E. The skin may act as a blood reservoir by holding up to 5% of the body’s blood supply, which may be diverted to other areas of the body should the need arise (pp. 161–162). F. Limited amounts of nitrogenous wastes are excreted through the skin (p. 162). Homeostatic Imbalances of Skin (pp. 162–165; Figs. 5.8–5.10) A. Skin Cancer (pp. 162–163; Fig. 5.8) 1. Basal cell carcinoma is the least malignant and the most common skin cancer. 2. Squamous cell carcinoma tends to grow rapidly and metastasize if not removed. 3. Melanoma is the most dangerous of the skin cancers because it is highly metastatic and resistant to chemotherapy. B. Burns (pp. 163–165; Figs. 5.9–5.10) 1. A burn is tissue damage inflicted by intense heat, electricity, radiation, or certain chemicals, all of which denature cell proteins and cause cell death to infected areas. 2. The most immediate threat to a burn patient is dehydration and electrolyte imbalance due to fluid loss. 3. After the first 24 hours has passed, the threat to a burn patient becomes infection to the wound site. 4. Burns are classified according to their severity. a. First-degree burns involve damage only to the epidermis. b. Second-degree burns injure the epidermis and the upper region of the dermis. c. Third-degree burns involve the entire thickness of the skin. Developmental Aspects of the Integumentary System (p. 165) A. The epidermis develops from the embryonic ectoderm, and the dermis and the hypodermis develop from the mesoderm (p. 165). B. By the end of the fourth month of development the skin is fairly well formed (p. 165). C. During infancy and childhood, the skin thickens and more subcutaneous fat is deposited (p. 165). D. During adolescence, the skin and hair become oilier as sebaceous glands are activated (p. 165). E. The skin reaches its optimal appearance when we reach our 20s and 30s; after that time the skin starts to show the effects of cumulative environmental exposures (p. 165). F. As old age approaches, the rate of epidermal cell replacement slows and the skin thins, becoming more prone to bruising and other types of injuries (p. 165). 6: Bones and Skeletal Tissues Objectives Bone Development Compare and contrast intramembranous ossification and endochondral ossification. Describe the process of long bone growth that occurs at the epiphyseal plates. Bone Homeostasis: Remodeling and Repair Compare the locations and remodeling functions of the osteoblasts, osteocytes, and osteoclasts. Explain how hormones and physical stress regulate bone remodeling. Describe the steps of fracture repair. Homeostatic Imbalances of Bone Contrast the disorders of bone remodeling seen in osteoporosis, osteomalacia, and Paget’s disease. Developmental Aspects of Bones:Timing of Events Describe the timing and cause of changes in bone architecture and bone mass throughout life. Outline Bone Development (pp. 182–185; Figs. 6.8–6.11) A. Formation of the Bony Skeleton (pp. 182–184; Figs. 6.8–6.9) 1. Intramembranous ossification forms membrane bone from fibrous connective tissue membranes, and results in the cranial bones and clavicles. 2. In endochondral ossification bone tissue replaces hyaline cartilage, forming all bones below the skull except for the clavicles. a. Initially, osteoblasts secrete osteoid, creating a bone collar around the diaphysis of the hyaline cartilage model. b. Cartilage in the center of the diaphysis calcifies and deteriorates, forming cavities. c. The periosteal bud invades the internal cavities and spongy bone forms around the remaining fragments of hyaline cartilage. d. The diaphysis elongates as the cartilage in the epiphyses continues to lengthen and a medullary cavity forms through the action of osteoclasts within the center of the diaphysis. e. The epiphyses ossify shortly after birth through the development of secondary ossification centers. B. Postnatal Bone Growth (pp. 184–185; Figs. 6.10–6.11) 1. Growth in length of long bones occurs at the ossification zone through the rapid division of the upper cells in the columns of chondrocytes, calcification and deterioration of cartilage at the bottom of the columns, and subsequent replacement by bone tissue. 2. Growth in width, or thickness, occurs through appositional growth due to deposition of bone matrix by osteoblasts beneath the periosteum. 3. Hormonal Regulation of Bone Growth a. During infancy and childhood, the most important stimulus of epiphyseal plate activity is growth hormone from the anterior pituitary, whose effects are modulated by thyroid hormone. b. At puberty, testosterone and estrogen promote a growth spurt, but ultimately induct the closure of the epiphyseal plate. Bone Homeostasis: Remodeling and Repair (pp. 185–190; Figs. 6.11–6.15; Table 6.2) A. Bone Remodeling (pp. 185–188; Figs. 6.11–6.13) 1. In adult skeletons, bone remodeling is balanced bone deposit and removal; bone deposit occurs at a greater rate when bone is injured; and bone resorption allows minerals of degraded bone matrix to move into the blood. 2. Control of Remodeling a. The hormonal mechanism is mostly used to maintain blood calcium homeostasis, and balances activity of parathyroid hormone and calcitonin. b. In response to mechanical stress and gravity, bone grows or remodels in ways that allow it to withstand the stresses it experiences. B. Bone Repair (pp. 188–190; Fig. 6.15; Table 6.2) 1. Fractures are breaks in bones, and are classified by: the position of the bone ends after fracture, completeness of break, orientation of the break relative to the long axis of the bone, and whether the bone ends penetrate the skin. 2. Repair of fractures involves four major stages: hematoma formation, fibrocartilaginous callus formation, bony callus formation, and remodeling of the bony callus. Homeostatic Imbalances of Bone (pp. 189–191, 194; Fig. 6.16) A. Osteomalacia and Rickets (p. 189) 1. Osteomalacia includes a number of disorders in adults in which the bone is inadequately mineralized. 2. Rickets is inadequate mineralization of bones in children caused by insufficient calcium or vitamin D deficiency. B. Osteoporosis refers to a group of disorders in which the rate of bone resorption exceeds the rate of formation (pp. 189–191, Fig. 6.16). 1. Bones have normal bone matrix, but bone mass is reduced and the bones become more porous and lighter, increasing the likelihood of fractures. 2. Older women are especially vulnerable to osteoporosis, due to the decline in estrogen after menopause. 3. Other factors that contribute to osteoporosis include a petite body form, insufficient exercise or immobility, a diet poor in calcium and vitamin D, abnormal vitamin D receptors, smoking, and certain hormone-related conditions. C. Paget’s disease is characterized by excessive bone deposition and resorption, with the resulting bone abnormally high in spongy bone. It is a localized condition that results in deformation of the affected bone (pp. 191, 194). Developmental Aspects of Bones: Timing of Events (p. 194; Fig. 6.17) A. The skeleton derives from embryonic mesenchymal cells, with ossification occurring at precise times. Most long bones have obvious primary ossification centers by 12 weeks gestation (p. 194). B. At birth, most bones are well ossified, except for the epiphyses, which form secondary ossification centers (p. 194). C. Throughout childhood, bone growth exceeds bone resorption; in young adults, these processes are in balance; in old age, resorption exceeds formation (p. 194). 8: Joints Objectives Classification of Joints 1. Define joint or articulation. 2. Classify joints structurally and functionally. Fibrous Joints 3. Describe the general structure of fibrous joints. Name and give an example of each of the three common types of fibrous joints. Cartilaginous Joints 4. Describe the general structure of cartilaginous joints. Name and give an example of each of the two common types of cartilaginous joints. Synovial Joints 5. Describe the structural characteristics of synovial joints. 6. Compare the structures and functions of bursae and tendon sheaths. 7. List three natural factors that stabilize synovial joints. Outline Classification of Joints (pp. 248–249; Figs. 8-1–8.3; Table 8.1) A. Structural classification focuses on the material binding the bones together and whether or not a joint cavity is present (p. 249; Table 8.1). 1. In fibrous joints the bones are joined together by fibrous tissue and lack a joint cavity. 2. In cartilaginous joints the bones are joined together by cartilage and they lack a joint cavity. 3. In synovial joints, the articulating bones are separated by a fluid-containing joint cavity. B. Functional classification is based on the amount of movement allowed at the joint (p. 249). 1. Synarthroses are immovable joints. 2. Amphiarthroses are slightly movable joints. 3. Diarthroses are freely movable joints. Fibrous Joints (pp. 249–250; Fig. 8.1; Tables 8.1–8.2) A. Sutures occur between bones of the skull and use very short connective tissue fibers to hold the bones together (p. 249; Fig. 8.1). B. In syndesmoses, the bones are connected by a ligament, which is a cord or band of fibrous tissue (pp. 249–250; Fig. 8.1). C. A gomphosis is a peg-in-socket fibrous joint (p. 250; Fig. 8.1). Cartilaginous Joints (pp. 250–251; Fig. 8.2; Tables 8.1–8.2) A. Synchondroses involve a bar or plate of hyaline cartilage uniting the bones, such as the epiphyseal plate (pp. 250–251; Fig. 8.2). B. In symphyses, such as the pubic symphysis, the articular surfaces are covered with articular cartilage that is then fused to an intervening pad or plate of fibrocartilage (p. 251; Fig. 8.2). Synovial Joints (pp. 251–269; Figs. 8.3–8.8, 8.10–8.13; Tables 8.1–8.2) A. The general structure of a synovial joint contains five distinguishing features (pp. 251– 252; Fig. 8.3). 1. Articular cartilage covers the ends of the articulating bones. 2. The joint (synovial) cavity is a space that is filled with synovial fluid. 3. The two-layered articular capsule encloses the joint cavity. 4. Synovial fluid is a viscous, slippery fluid that fills all free space within the joint cavity. 5. Reinforcing ligaments cross synovial joints to strengthen the joint. B. Bursae and tendon sheaths are bags of lubricant that reduce friction at synovial joints (p. 252; Fig. 8.4).