Velardo Presentation (PPT 3MB)
advertisement

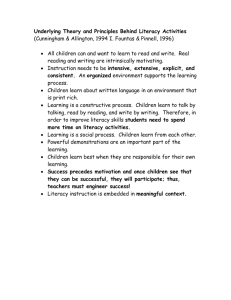
The relationship between parental health literacy and health-related parenting practices: A qualitative study of intergenerational health Stefania Velardo Honours Supervisor: Associate Professor Murray Drummond Educational Futures Annual Conference 2010 BACKGROUND Poor physical health of Australian children: Early years of life set the foundation for future health Good nutrition and PA essential (AIHW, 2009) Many children not meeting daily recommendations (AIHW, 2009; DoHA, 2008) 17% overweight and 8% obese (aged 5-17) (ABS, 2009) Obesity = poor physical and psychosocial health outcomes (Goran et al., 2003; Lee, 2009) & pressure on health system (Withrow & Alter, 2010) Increased portion sizes for packaged foods/restaurant meals Increased consumption of high-fat foods away from home (Stanton, 2006) Increased exposure to unhealthy food advertisements (Chapman et al., 2006) …”Pester Power”… (Kral et al., 2004) (Marshall et al., 2007) Increased energy consumption Increased availability of highenergy fatty foods (Popkin et al., 2005) OBESOGENIC ENVIRONMENT (Swinburn et al., 1999) Decreased energy expenditure Increase in sedentary activities (AIHW, 2009; Dennison & Edmunds, 2008) Declining cost of high energy foods & increased cost of healthy eating (NHMRC, 2003) SES Perceived parental concerns over children’s safety, e.g. “stranger danger” (Carver et al., 2007) Health improves with higher SES position (Glover et al., 2006) Inverse association between SES and childhood obesity in Australia (O’Dea, 2008). BACKGROUND Parental Influence: Home setting comprises the strongest influence on diet & PA (Golan, 2006) Parents are responsible for establishing a healthy home environment (Anzman et al., 2010; Howard, 2007; Lindsay et al., 2006; Tucker, 2009) BACKGROUND Mechanisms: DECISION MAKING– preparing foods, recreational activities, purchase and regulation of commodities (Dennison & Edmunds, 2008; Golan & Crow 2004a; 2004b) ROLE MODEL - own food preferences inextricably influence children's (Benton, 2004; Ventura & Birch, 2008) modeling of behaviours (Anzman et al., 2010; Golan & Crow, 2004b) repeated exposure (Menella et al., 2008; Wardle et al., 2003) BACKGROUND Intergenerational Transmission: Paucity of literature re transmission of health-related skills (Lindenboom et al, 2009). Health literacy (HL) Early definitions = limited concept concerned with literacy skills in health-related settings (Peerson & Saunders, 2009) Over time, a broader conceptualisation = “the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health” (Nutbeam, 1998, p. 357) Decision making about health in everyday life BACKGROUND Most studies quantitative – limited to individual health outcomes (Gazmararian et al., 2003; Yin et al., 2007) Few studies re parental HL and child health (DeWalt et al., 2007; Shone et al., 2009) but limited to chronic illness management Most studies used validated quantitative methodological tools, e.g. REALM or TOFHLA but these are not comprehensive (Baker, 2006; Nutbeam, 2008) Only two qualitative HL studies –low back pain patients/ visually impaired women (Briggs et al., 2010; Harrison et al, 2010) Themes related to socio-cultural factors affecting HL AIM & OBJECTIVES AIM: To explore the relationship between parental health literacy and healthrelated parenting practices, in a low socio-economic region. Aspects of health-related parenting practices to be examined relate to child dietary behaviours and physical activity OBJECTIVES: To understand the concept of health literacy among parents from a low socio-economic region To develop an understanding of how parents access and interpret health information To explore the ways in which health literacy is translated into health-related parenting practices To develop recommendations that focus on the needs of parents, as a point of intervention METHODS Qualitative approach - generate rich, detailed data to explain and interpret social phenomena (Pope & Mays, 2006) Theoretical framework social constructionism = development of social phenomena through social processes and practices (Burr, 2003) Society and culture impact on health – socially constructed expectations How are social institutions perpetuated and maintained from one generation to the next? A Conceptual Framework for Understanding Children’s Physical Health SES Parental Health Literacy (Socioeconomic Status) Social construction of parenting Primary construction of child’s health-related behaviours and attitudes Via Cultural norms that suggest suitable behaviours Intergenerational Health Social construction of the meaning of health Construction of the Obesogenic Environment Socio-cultural changes become social norms around eating/physical activity “…A culture of convenience…” Children’s Physical Health Dietary Patterns Physical Activity Peers Reinforcement of constructed norms/behaviours Media Advertising Fast Foods Preparation Practices Portion Sizes Pricing Sedentary activities Safety School SAMPLE 14 parents from two-parent families Children aged from birth to 12 years Living in the City of Onkaparinga Purposive sampling – local service providers, snowball Basis for recruitment: significant role of parents & decline of influence as children become adolescents (Lindsay et al., 2006) differences between single and two parent families (Gorman & Braverman, 2008) low SES region in accordance to SEIFA (ABS, 2008) DATA COLLECTION & ANALYSIS 2 semi-structured focus groups (4/6 participants) Interaction, exchange of ideas, rich data (Kitzinger, 2006) 4 in-depth individual interviews Pursue issues in a private manner Basis of triangulation – cross check findings, increase internal validity (Bryman, 2008) Audio-recorded, transcribed verbatim (Halcomb & Davidson, 2006) Thematic analysis RESULTS 5 principal themes related to how parents access, understand and use health-related information with children 1. USING THE INTERNET AS A TOOL 2. INTERPERSONAL VERSUS ORGANISATIONAL NETWORKS 3. THE NOTION OF PHYSICAL HEALTH: COMMON SENSE VERSUS COMPLEXITY 4. THE COST OF PHYSICAL HEALTH 5. THE INFLUENCE OF THE MEDIA RESULTS 1. USING THE INTERNET AS A TOOL Information-seeking and networking tool Google, online forums E-health literacy (Kreps & Neuhauser, 2010) the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem Barrier = time constraints, “information overload” (*pros & cons) Barrier = ability to critically seek and evaluate information “When you look on the Internet, you could just be someone like me, or somebody who doesn’t have a qualification could write something, put their name on it, and call themselves a health professional, and you read what they’ve written. You’ve really just got to look on the Internet and hope you’re reading the right thing” RESULTS 2. INTERPERSONAL VERSUS ORGANISATIONAL NETWORKS Interpersonal networks – family & friends, other parents Experienced, comfortable – relevant, trustworthy info “A lot of it is just talking to groups of mums who are similar to me, who’ve had kids. So you know, what they do and what they suggest. I mean my girlfriend just went to a talk about preservatives at the school so then she may bring that information back to me and say “look, these certain biscuits have a lot of preservatives so don’t get those”. And then I might do the same for her. So yeah it’s mainly feedback from other mums which is useful.” Organisational networks – GPs, dieticians, parent help line Associated with illness/specific concern RESULTS 3. THE NOTION OF PHYSICAL HEALTH – COMMON SENSE VERSUS COMPLEXITY Good Physical Health Common sense viewpoint Complex aspects of dietary intake & PA recommendations Common sense viewpoint Basic components – easy, straightforward, common sense “But you know, everyone knows that you should eat more fruit and veg and organic and all that sort of stuff. Like fresh food, everyone knows that. They put across that message a lot through the TV and newspapers. You hear about it all the time.” Key messages – “Go for 2&5”, “Be active” – reaching wider community RESULTS Complex aspects = RDI/FOOD LABELS Australian Guide to Healthy Eating VS food pyramid “Like you know roughly what foods they can have but sometimes it’s how often. Like how many times for carbohydrates a week. I just do a rough guide but at the end of the day, how do I know if it’s right? It’s hard and it comes down to your judgment.” Food labels –useful aspects per 100g/%RDI Barrier = calculating overall intake, time consuming & difficult What is actually healthy? Lack of services/resources = guessing, own judgment, avoidance RESULTS Complex aspects (cont.) = PA/screen time recommendations No parents familiar with PA guidelines (2 aware of screen time) Predominantly common sense attitude – lack of concern The physical part is more straightforward, like you know they should be active every day, but the nutritional bit is more involved. Like that could be more confusing, there’s more to think about I guess... But I know that as a kid she’s going to run around and play games, so as long as she’s moving and not sitting around all the time that’s easy for me. I don’t have to worry”. Screen time – “where to draw the line?” Educational?? RESULTS 4. THE COST OF PHYSICAL HEALTH Maintaining Good Physical Health Financial burden Time constraints It costs more to be healthy $$$$ Good physical health •High cost of healthy snack foods •Fruit/veg VS junk foods •High cost of healthy snacks •Organised sport – uniforms, membership fees •Safety – decrease in “free” incidental activity “It’s hard to find the time for all of these things, whether it’s the food or the exercise, because everyone’s busy. Lifestyle choices change because people are just too busy and we’re very conscious of it.” = more time consuming •Junior sport •Accessing local resources •Safety •Food labels/meal planning •Preparing healthy meals •Social construction of the busy, modern lifestyle RESULTS 5. THE INFLUENCE OF THE MEDIA Advertising and marketing “Your ideas are competing with the world’s from the start.” TV ads – fast food/confectionery Supermarket buying power (products endorsed) Peer pressure Pester power – food/electronic devices Challenging….feelings of guilt…. succumb or “give in” There’s always so many different things coming out on the TV and the kids have got to have it. They see other kids at that same age with it, so you’ve got to try to keep up. It’s hard because they’ve actually said before, “well Mum, you’re not a good parent if you don’t buy that for us”. So it makes it hard because you feel pressure to get it because you don’t want to make them feel left out. RECOMMENDATIONS Theme Issue Recommendation 1 Internet – low levels of critical literacy & navigational difficulties Develop skills in conducting online searches (short demonstrations) (Gilmour, 2007) Lack of understanding of national dietary/PA recommendations Emphasise national guidelines through additional media campaigns to convey simple, consistent messages Difficulty interpreting food labels & converting knowledge to food choice Improve underlying literacy and numeracy skills (Rothman et al., 2006) 3 Promotion of already established sites which are accurate & user-friendly Promotion of Australian Guide to Healthy Eating (proportions/recommended daily serves) Improving design of Australian food labels – quick, simplified strategies such as UK Traffic Light System (Kelly et al., 2009) 4 Social construction of good physical health – financial burden & time scarcity Increase awareness of cost-effective healthy meals by developing capabilities around identification and use of seasonal fresh produce (Waterlander et al., 2010) Promote participation in local community gardens (Alaimo et al., 2008) Health education strategies to draw on the provision of quick, simple healthy recipes 5 Expensive fresh produce Federal support – social infrastructure Revision of agricultural policies/subsidies to support healthy crops (Swinburn, 2008) Media/peer pressure (guilt) Parents more likely to “give in” Public health programs to develop parental capacity to behaviourally manage food/recreational requests CONCLUSION Parents identified many perceived barriers to making informed, healthy choices for children, which may impact on weight status and wellbeing Complex relationship - further qualitative inquiry needed Future directions - develop a deeper understanding of factors which enhance or act as barriers to healthy nutrition and physical activity behaviours amongst children, across diverse communities Develop our understanding of the complex relationship between healthseeking behaviours and socio-economic position. REFERENCES (page 1/4) Alaimo, K., Packnett, E., Miles, R., & Kruger, D. (2008). Fruit and vegetable intake among urban community gardeners. Journal of Nutrition Education and Behavior, 40(2), 94-101 Anzman, S., Rollins, B., & Birch, L. (2010). Parental influence on children's early eating environments and obesity risk: implications for prevention. International Journal of Obesity, 1-9. Australian Bureau of Statistics [ABS]. (2008). Census of population and housing: Socio-economic indexes for areas (SEIFA) – Data only 2006. (Catalogue No. 2033.0.55.001). Canberra, Australia: ABS. Australian Bureau of Statistics [ABS]. (2009). National Health Survey: Summary of Results 2007-2008. (Cat. No. 4364.0). Canberra: ABS. Australian Institute of Health and Welfare [AIHW]. (2009). A picture of Australia’s children 2009. (Cat. No. PHE 112). Canberra: AIHW. Baker, D. (2006). The meaning and the measure of health literacy. Journal of General Internal Medicine, 21(8), 878-883. Benton, D. (2004). Role of parents in the determination of the food preferences of children and the development of obesity. International Journal of Obesity, 28(7), 858-869. Briggs, A.M., Jordan, J.E., Buchbinder, R., Burnett, A.F., O’Sullivan, P.B., Chau, J.Y.Y., et al. (2010). Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain, 150, 275-283. Bryman, A. (2008). Social Research Methods (3rd ed.). Oxford: Oxford University Press. Burr, V. (2003). Social constructionism (2nd ed.). London: Routledge. Carver, A., Timperio, A., & Crawford, D. (2008). Playing it safe: The influence of neighbourhood safety on children's physical activity—A review. Health and Place, 14(2), 217-227. Chapman, K., Nicholas, P., & Supramaniam, R. (2006). How much food advertising is there on Australian television? Health Promotion International, 21(3), 172180. Dennison, B. A., & Edmunds, L. S. (2008). The role of television in childhood obesity. Progress in Pediatric Cardiology, 25(2), 191-197. Department of Health and Ageing [DoHA]. (2008). 2007 Australian national children's nutrition and physical activity survey: main findings. Canberra: Commonwealth of Australia. DeWalt, D., Dilling, M., Rosenthal, M., & Pignone, M. (2007). Low parental literacy is associated with worse asthma care measures in children. Ambulatory Pediatrics, 7(1), 25-31. REFERENCES (page 2/4) Gazmararian, J., Williams, M., Peel, J., & Baker, D. (2003). Health literacy and knowledge of chronic disease. Patient Education and Counseling, 51(3), 267-275. Gilmour, J. A. (2007). Reducing disparities in the access and use of Internet health information. a discussion paper. International Journal of Nursing Studies, 44(7), 1270-1278. Glover, J., Hetzel, D., Glover, L., Tennant, S., & Page, A. (2006). A social health atlas of South Australia (Third edition). Adelaide: The University of Adelaide. Golan, M. (2006). Parents as agents of change in childhood obesity–from research to practice. International Journal of Pediatric Obesity, 1(2), 66-76. Golan, M., & Crow, S. (2004a). Parents are key players in the prevention and treatment of weight-related problems. Nutrition Reviews, 62(1), 39-50. Golan, M., & Crow, S. (2004b). Targeting Parents Exclusively in the Treatment of Childhood Obesity: Long-Term Results. Obesity, 12(2), 357-361. Goran, M., Ball, G., & Cruz, M. (2003). Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. Journal of Clinical Endocrinology & Metabolism, 88(4), 1417-1427. Gorman, B. K., & Braverman, J. (2008). Family structure differences in health care utilization among U.S. children. Social Science & Medicine, 67(11), 1766-1775. Halcomb, E., & Davidson, P. (2006). Is verbatim transcription of interview data always necessary? Applied Nursing Research, 19(1), 38-42. Harrison, T., Mackert, M., & Watkins, C. (2010). Health Literacy Issues Among Women with Visual Impairments. Research in Gerontological Nursing, 3(1), 49-60. Howard, K. (2007). Childhood overweight: parental perceptions and readiness for change. The Journal of School Nursing, 23(2), 73-79. Kelly, B., Hughes, C., Chapman, K., Louie, J., Dixon, H., Crawford, J., et al. (2009). Consumer testing of the acceptability and effectiveness of front-of-pack food labelling systems for the Australian grocery market. Health Promotion International, 24(2), 120-129. Kitzinger, J (2006). Focus groups. In C. Pope & N. Mays (Eds.), Qualitative research in health care (3rd ed.) (pp. 21-31). Malden, Mass.: Blackwell Publishing. Kral, T., Roe, L., & Rolls, B. (2004). Combined effects of energy density and portion size on energy intake in women. American Journal of Clinical Nutrition, 79(6), 962-968. Kreps, G. L., & Neuhauser, L. (2010). New directions in eHealth communication: opportunities and challenges. Patient Education and Counseling, 78(3), 329336. Lee, Y. (2009). Consequences of childhood obesity. Annals Academy of Medicine, 38(1), 75-77. Lindeboom, M., Llena-Nozal, A., & Van der Klaauw, B. (2009). Parental education and child health: evidence from a schooling reform. Journal of Health Economics, 28(1), 109-131. REFERENCES (page 3/4) Lindsay, A., Sussner, K., Kim, J., & Gortmaker, S. (2006). The role of parents in preventing childhood obesity. The Future of children, 16(1), 169-186. Marshall, D., O'Donohoe, S., & Kline, S. (2007). Families, food, and pester power: beyond the blame game? Journal of Consumer Behaviour, 6(4), 164-181. Mennella, J., Nicklaus, S., Jagolino, A., & Yourshaw, L. (2008). Variety is the spice of life: strategies for promoting fruit and vegetable acceptance during infancy. Physiology & behavior, 94(1), 29-38. National Health and Medical Research Council [NHMRC]. (2003). Dietary guidelines for children and adolescents in Australia. Canberra: Commonwealth of Australia. Nutbeam, D. (1998). Health promotion glossary. Health Promotion International, 13(4), 349-364. Nutbeam, D. (2008). The evolving concept of health literacy. Social Science & Medicine, 67(12), 2072-2078. O'Dea, J. (2008). Gender, ethnicity, culture and social class influences on childhood obesity among Australian schoolchildren: implications for treatment, prevention and community education. Health and Social Care in the Community, 16(3), 282-290. Peerson, A., & Saunders, M. (2009). Health literacy revisited: what do we mean and why does it matter? Health Promotion International, 24(3), 285-296. Pope, C., & Mays, N. (2006). Qualitative methods in health research. In C. Pope & N. Mays (Eds.), Qualitative research in health care (3rd ed.) (pp. 1-11). Malden, Mass.: Blackwell Publishing. Popkin, B., Duffey, K., & Gordon-Larsen, P. (2005). Environmental influences on food choice, physical activity and energy balance. Physiology & behavior, 86(5), 603-613. Rothman, R. L., Housam, R., Weiss, H., Davis, D., Gregory, R., Gebretsadik, T., et al. (2006). Patient understanding of food labels: the role of literacy and numeracy. American Journal of Preventive Medicine, 31(5), 391-398. Shone, L. P., Conn, K. M., Sanders, L., & Halterman, J. S. (2009). The role of parent health literacy among urban children with persistent asthma. Patient Education and Counseling, 75(3), 368-375. Stanton, R. (2006). Nutrition problems in an obesogenic environment. Medical Journal of Australia, 184(2), 76-79. Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29(6), 563-570. Swinburn, B. (2008). Obesity prevention: the role of policies, laws and regulations. Australia and New Zealand health policy, 5(1), 12-19. Tucker, S. (2009). Parents as agents of change for childhood obesity prevention: a clinical nursing research programme. Paediatrics and Child Health, 19, 189193. REFERENCES (page 4/4) Ventura, A., & Birch, L. (2008). Does parenting affect children's eating and weight status? International Journal of Behavioral Nutrition and Physical Activity, 5(1), 15-27. Wardle, J., Cooke, L., Gibson, E., Sapochnik, M., Sheiham, A., & Lawson, M. (2003). Increasing children's acceptance of vegetables; a randomized trial of parent-led exposure. Appetite, 40(2), 155-162. Waterlander, W., De Mul, A., Schuit, A., Seidell, J., & Steenhuis, I. (2010). Perceptions on the use of pricing strategies to stimulate healthy eating among residents of deprived neighbourhoods: a focus group study. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 44-56. Withrow, D., & Alter, D. (2010). The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obesity Reviews. Yin, H. S., Forbis, S. G., & Dreyer, B. P. (2007). Health Literacy and Pediatric Health. Current Problems in Pediatric and Adolescent Health Care, 37(7), 258-286. QUESTIONS???