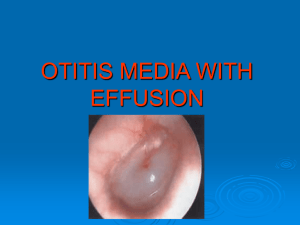
OTITIS MEDIA CLASSIFICATION OF OTITIS MEDIA Acute otitis
advertisement
OTITIS MEDIA CLASSIFICATION OF OTITIS MEDIA Acute otitis media (AOM) — (AOM) is an acute illness marked by the presence of middle ear fluid and inflammation of the mucosa that lines the middle ear space Caused by obstruction of the eustachian tube, AOM may also be associated with purulent otorrhea if there is a ruptured tympanic membrane. AOM usually responds promptly to antimicrobial therapy. Otitis media with effusion — (OME) is defined by the presence of middle ear fluid without acute signs of illness or inflammation of the middle ear mucosa. OME usually follows AOM , can result from barotraumas or allergy. Eustachian tube dysfunction is often a predisposing factor. Rarely, caused by obstruction of the eustachian tube orifice in the nasopharynx. Consider a mass or cancer such as nasopharyngeal carcinoma. OME typically leads to a conductive hearing loss Acute mastoiditis — The mastoid antrum serves as an air space connecting the middle ear to the mastoid air cells. Thus, most cases of AOM are associated with some degree of mastoid inflammation or infection ("mastoiditis"). Chronic otitis media — (COM) is diagnosed in an ear with a tympanic membrane perforation in the setting of chronic ear infections, such as an ear with chronic purulent drainage despite appropriate antibiotic treatment. Chronic serous drainage (typically straw-colored) is termed chronic serous otitis media. Chronic purulent drainage is termed as chronic suppurative otitis media. ETIOLOGY OF OTITIS MEDIA Eustachian tube dysfunction (ETD)— Persistent eustachian tube dysfunction-----induces negative pressure in the middle ear space, lack of aeration and the accumulation of effusions--- causes-- AOM or otitis media with effusion (OME). Seasonal allergic rhinitis Upper respiratory tract infections. Other Causes of ETD are mucosal disease (inflammatory, immunologic impairment, or immotile cilia), extrinsic compression (nasopharyngeal tumor or enlarged adenoid), or palatal muscle dysfunction (cleft palate and other craniofacial anomalies). MICROBIOLOGY S. pneumoniae is the most important bacterial cause of AOM in adults. Staphylococcus aureus, including MRSA, are an uncommon cause of AOM but can occur in patients with chronic suppurative otitis media and may be associated with persistent otorrhea that follows insertion of tympanostomy tubes. Group A streptococcus (GAS) was the leading cause of AOM during the preantibiotic era. CLINICAL MANIFESTATIONS OF AOM — Otalgia (ear pain) and decreased hearing. ( usually relieved by perforation ) Fever may not be present. A preceding URTI or exacerbation of seasonal allergic rhinitis may herald the onset of AOM by several days. Dysequilibrium is described infrequently. Conductive hearing loss is usually transient. High fever, severe pain behind the ear, or facial paralysis, suggest unusual complications DIAGNOSIS Use pneumatic otoscopy to evaluate the eardrum for evidence of OME. Tympanic membrane redness, opacification, bulging, and poor mobility when pneumatic pressure is applied using a pneumatic otoscope. Air fluid Level Purulence in the ear canal if there is an associated tympanic membrane rupture. Tympanometry Techniques to predict the presence or absence of middle ear effusion. If tympanometry is normal, acute otitis media is unlikely. Consider other causes of hearing loss. If the eardrum is mobile and tympanometry is negative, consider other causes of hearing loss. Evaluate hearing in patients with persistent OME for more than 3 months. Hearing test in cases of persistent OME with a tuning fork examination (512 Hz) may demonstrate conductive hearing loss. .Fiberoptic nasopharyngoscopy should be performed to rule out nasopharyngeal pathology in patients with recurrent unilateral serous otitis media. ( individuals from China, Southeast Asia, and Northern Africa are at increased risk for nasopharyngeal carcinoma TREATMENT Choice of initial antibiotic — must be active against S. pneumoniae, NT H. influenzae, and M. catarrhalis Amoxicillin remains the drug of choice for initial therapy of AOM:: ●Mild to moderate disease: 500 mg every 12 hours, or 250 mg every 8 hours ●Severe disease (eg, patients with fever, significant hearing loss, severe pain, and/or marked erythema): 875 mg every 12 hours, or 500 mg every 8 hours Streptococcus pneumoniae that are not fully susceptible to penicillin. Amoxicillinclavulanate should be considered for patients with severe otalgia or elevated temperature to cover the possibility of beta-lactamase producing NT H. influenzae. Duration of Treatment : Mild to moderate disease be treated for five to seven days, Severe disease receive a 10-day Penicillin allergy — Choice depends upon the type of the previous hypersensitivity reaction. ●If no type 1 hypersensitivity reaction (urticaria or anaphylaxis), consider the following: •Cefdinir (300 mg twice a day or 600 mg once daily) •Cefpodoxime (200 mg twice a day) •Cefuroxime (500 mg every 12 hours) •Ceftriaxone (2 g IM or IV once) ● If known and severe allergy to beta-lactam antibiotics, a macrolide (erythromycin combined with sulfisoxazole, or azithromycin, or clarithromycin) is the preferred drug. Trimethoprim-sulfamethoxazole Lack of initial response — With appropriate antimicrobial therapy, most patients with AOM are significantly improved within 48 to 72 hours. If there is no improvement, the patient should be reexamined. Assess for a new focus of infection or have received inadequate therapy. When amoxicillin fails, consider second-line regimens include amoxicillinclavulanate or a second-generation cephalosporin such as cefuroxime axetil, or a third-generation cephalosporin (such as oral cefdinir or intramuscular ceftriaxone). Effusions will resolve over the course of 12 weeks Myringotomy with tympanostomy tubes may be considered for persistent symptomatic effusions at 12 weeks, and earlier for selected patients with need for immediate pressure equalization (eg, air travel that cannot be deferred)