Impact and Lack of Impact of the 2004
advertisement

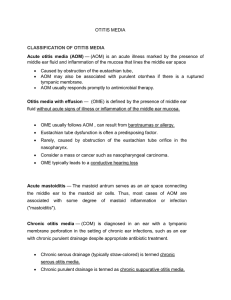
Impact and Lack of Impact of the 2004 Clinical Academies’ Guidelines on the Medical Management of Otitis Media in the United States Lawrence C Kleinman, MD, MPH Leonardo Trasande, MD, MPP Salomeh Keyhani, MD, MPH Mount Sinai School of Medicine New York, NY Dr. Kleinman has no financial or other conflicts to disclose Evaluation of OM Guidelines Clinical and Policy Context The Clinical Academies’ Guidelines Data and Analysis Findings Conclusion Clinical Context: Otitis Media Acute Otitis Media – Symptomatic disease acute onset – Presents typically with fever and ear pain – Infectious etiology: bacterial or viral – “Ear Infection” Otitis Media with Effusion – Often asymptomatic, hearing loss frequent – Rarely infectious (may follow AOM) – “Fluid in the ear” or “Glue Ear” (UK) Policy Context Antibiotic resistance increasing ca. 1998 CDC strategic decision to focus on ↓ Abx use by pediatricians Otitis Media most common illness in children – #2 in medicine (HTN) The Guidelines 2004 AAP/AAFP Guideline on AOM recommends watchful waiting as a preferred initial Rx in some circumstances – Clinical Data: ∃ Large subset of children for whom delaying Abx does not result in lasting harm – Abx shorten course of AOM by 1 day on average 2004 update of 1994 AAP/AAFP/AAO-HNS OME Guideline removes Abx option except as last ditch effort to avoid surgery that parents don’t want – Clinical Data: Treat seven children with Abx to eliminate one child with effusion 2004 AAP/AAFP AOM Guideline Age < 6 months Age 6 m to 2 years Severe Not Severe Certain Dx Uncertain Dx Antibiotics Antibiotics Antibiotics Antibiotics Antibiotics WW Antibiotics WW WW WW Age > 2 years Severe Not Severe • Certain dx is all 3 of: rapid onset, signs of middle ear effusion, and symptoms of middle ear inflammation. • Severe: moderate to severe otalgia and/or fever > 39oC in past 24 hours. • Observation (watchful waiting) option is only appropriate when follow-up can be assured and antibiotics started if symptoms persist or worsen. Study Overview Did antibiotic use for AOM or OME change as a result of (in association with) the 2004 OM Guidelines? Interrupted Time Series – Segmented regression analysis of nationally representative data of ambulatory medical care Data Ambulatory visits for children birth through 16 years old from 2 National Center for Health Statistics annual surveys National Ambulatory Medical Care Survey (NAMCS) – Doctors offices National Hospital Ambulatory Medical Care Survey (NHAMCS) – Hospital Clinic visits – Emergency Department visits Segmented Regression Analysis CounterFACTUAL GUIDELINE EFFECT (2004) Washout Period FACTUAL ABX Use in AOM Abstract Period Proportion AOM with ABX 1 0.9 0.8 0.7 0.6 0.5 1992 1994 1996 1998 2000 2002 2004 2006 2008 Findings: AOM Trend Before: -0.2% /yr (p=0.45) Trend After: -2.0% /yr (p=0.57) Effect size: +4.3% (p=0.35) Factual : 82.3% Counter Factual 82.0% Guideline impact + 0.3% AOM: Ratio of Abx Use in Children Older than 2 yrs to Children < 2 yrs Abx use 2 or older / < 2 1.4 1.2 1 0.8 0.6 0.4 0.2 0 1992 1994 1996 1998 2000 2002 2004 2006 AOM: Ratio of Abx Use in Children Older than 2 yrs to Children < 2 yrs Trend Before*: ↓ 0.005 /yr (p=0.13) Trend After*: ↑ 0.12 /yr (p=0.88) Effect size: ↓ 0.009 (p=0.01) Factual : 1.28 Counter Factual 1.04 Guideline impact + 0.24 *Difference p<.01 OME Proportion OME with ABX 1 0.75 0.5 0.25 0 1992 1994 1996 1998 2000 2002 2004 2006 Findings OME Trend Before*: ↓ 1.9% /yr (p=0.004) Trend After*: Effect size: ↑ 9.9% /yr (p=0.30) - 6.3% (p=0.60) Factual : 51.6% Counter Factual 38.1% Guideline impact +13.5% *Difference p<.01 Antibiotic Use for Isolated URI Upper Respiratory Infection without OM, strep throat, pneumonia, UTI In 2006: 3.96 million children (22.4 %) received antibiotics Segmented Regression – ↓ 0.8% per year before guideline (p=0.38) – Guideline effect ↓ 2.6% (p=0.88) – ↑ 1.1% per year after guideline (p=0.92) – Factual 22.4% Counterfactual 22.8% (NS) Conclusions Physicians in the US have not changed fundamentally their use of antibiotics for either acute otitis media or otitis media with effusion subsequent to the guidelines If anything use in the targeted population for AOM (over 2 years) appears to have gone up relative to use in younger kids Many children receive antibiotics for conditions (e.g. URI) for which their use is inappropriate Implications for Policy, Delivery or Practice Guidelines that prioritized societal risk of bacterial resistance over a demonstrable but modest benefit to the individual child were not successful in changing behavior Pediatricians and family physicians may not be ready to follow the lead of their clinical societies in prioritizing population risks over individual patient benefit Questions for You Why do you think that the focus has been on reducing an effective use of antibiotics for children when antibiotics are so widely used for inappropriate reasons? Can you think of an equivalent example of a national society or a federal campaign focusing on reducing useful (appropriate) services in adults? Were the Guidelines correct in their prioritization? Thank you OMV Decreasing Otitis Media Visits By Year: 1994 - 2006 Abstract Period 30,000,000 20,000,000 10,000,000 0 1994 1996 1998 2000 2002 2004 2006 Slope = -621,654 (± 108,549), p = .0002 Proportion AOM with ABX 0.9 0.88 0.86 0.84 0.82 0.8 1992 1994 1996 1998 2000 2002 2004 2006 2008 2004 OME Guideline Targeting children 2 months through 12 years Watchful Waiting Recommended •For the first 90 days of an effusion in children who are not at risk (see text for definition) and continue surveillance at 3 to 6 month intervals until the effusion is no longer present, significant hearing loss is identified, or structural abnormalities of the TM or middle ear are suspected •All children for whom there is no consensus in favor of surgery among primary care physician, parent, and otolaryngologist Antibiotics •Not recommended unless as a short (10-14 day course) when a parent has strong aversion to impending surgery Tympanostomy Tubes Recommended Tympanostomy Tubes Optional Tympanostomy Tubes Mandatory •After 90 days, persistent hearing loss > 40 dB •OME lasting 4 months or longer with persistent hearing loss or other signs and symptoms •Recurrent or persistent OME in children at risk regardless of hearing status, and •If consensus between the primary care physician, otolaryngologist, and parent or caregiver •OME with posterosuperior retraction pockets, ossicular erosion, adhesive atelectasis, and retraction pockets that accumulate keratin debris 1994 AAP/AAFP/AAO-HNS OME Guideline Targeting otherwise healthy children 1 through 3 years old Watchful Waiting •Effusion Present Less than 90 Recommended days, OR •Absence of bilateral hearing loss > 20 dB, OR •Unilateral OME Antibiotics Optional •Bilateral Effusion Present 90 – 120 days, AND •Bilateral hearing loss > 20 dB 2004 OME Guideline Targets 2 months to 12 years old Antibiotics not recommended unless a parent has strong aversion to impending surgery Initial surgery: Tympanostomy Tubes Structural damage to the tympanic membrane or middle ear Only if consensus between ENT, PCP, and parent Otherwise healthy: Consider them after 4 months if persistent symptoms / hearing loss, recommended after 6 months Sooner in “at Risk” children – – – – – – – hearing loss independent of OME language or speech disorder autism and other developmental symptoms Down syndrome or other craniofacial syndromes visual impairment cleft palate developmental delay OM is Ubiquitous Most common illness in children 67% of children have >1 AOM, by 2 years old * 90% of closely observed children have > 1 episode OME by 2 years † * Teele DW, Klein JO, Rosner BA and the Greater Boston Otitis Media Study Group. JAMA 1983, PEDIATRICS, 1984. † Paradise et al. PEDIATRICS, 1997.