Presentation - Bradford VTS
advertisement
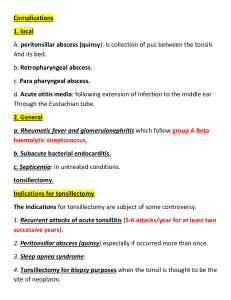
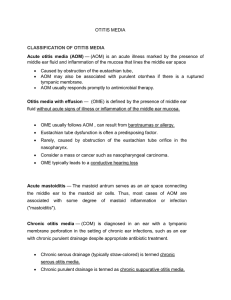
ENT for General Practice George Vattakuzhiyil MBBS;MS(ENT);FRCS Objectives Detailed examination of ENT/H&N Learn to diagnose & treat common ENT pathology Recognise serious complication, request additional tests, specialty referral Quick recap of ear anatomy Hearing tests Rinne and Weber tests Rinne Ac better than BC Hearing loss < 15db 256Hz 512HZ 1024Hz 15-30db x x 30-45db 45-60db x x x x x Weber test Hold the base of the tuning fork in the midline (forehead, incisor teeth) Laterelising to the left: conductive loss on left or SNHL on right Otitis Externa Inflammatory disorder of skin lined EAC Acute/Chronic Generelised skin disorder Pathogens: staph, pseudomonas, Fungus Topical antibiotic/steroid Sofradex,otomize spray,otosporin,GHC, locorten- vioform Otitis externa Extension to pre/post auricular area Microsuction/IV antibiotics Diabetic patient/ Pseudomonas inf ? Malignant otitis externa Acute otitis media Common in children otalgia/discharge Unwell/pyrexia TM: red, bulging,oedematous Streptococcus/Haemo philus Amoxycillin 5-7 days complications Acute mastoiditis Chronic otitis media Intracranial complications CSOM Recurrent ear discharge Hearing loss Perforation of the TM – central Presence of cholesteatoma Marginal, Attic perforation Offensive discharge, bleeding, granulations Complications Vestibular symptoms Facial palsy Intracranial complications Management Medical: Dry mopping,suction clearance,/ Ear drops, rarely systemic antibiotics Surgical Myringoplasty/ Tympanoplasty Combined Mastoidectomy/Tympanoplasty Otitis media+effusion-Glue ear Common in children Reduced hearing noticed by parents/teacher Recurrent ear infection Unsteadiness- child falling over Effusions persist for weeks after AOM 80% clear at 8 weeks Signs of OME Dull retracted TM May show air-fluid level Conductive hearing loss(whisper test, Rinne/weber tests) OME persistant over 3 months ENT referral Treatment Failed audio Flat tympanograms h/o >3 episodes in 6/12 or >4 in 12/12 Grommet insertion Evaluate adenoids, especially in recurrent grommet insertions Syringing the ear Which ear needs syringing? Occlusive cerumen Causing pain Hearing loss Tinnitus Avoid syringing Non occlussive cerumen Previous ear surgery Only hearing ear Perforated TM Kerotosis obturans Acute/Chronic tonsillitis Sorethroat, fever, malaise Tender cervical lymph nodes Enlarged congested tonsils with pus Analgesia Penicillin Prolonged course, worsening symptoms consider glandular fever Quincy (peritonsillar abscess) pain + trismus Swelling of the soft palate Displacement of uvula Refer for I/V antibiotics drainage Allergic rhinitis Seasonal : allergen usually outdoor perennial: indoor dust, mite, cat dander O/E pale mucosa, boggy turbinate Avoid allergen, antihistamines, topical vasoconstrictors, steroids Surgery- SMD, laser, Turbinectomy sinusitis Facial pain/ pressure/ fullness Nasal obstruction/ discharge Altered smell Pyrexia in acute sinusitis Headache, halitosis, dental pain Minor factors: cough,ear pressure, fatigue sinusitis Acute sinusitis < 4/52 Chronic >4/52 or 4 or more episodes O/E nasal congestion, polyps, pus in MM Structural changes: DNS, concha bullosa sinusitis Sinus X ray usually unhelpful CT sinuses Acute: amoxicillin clavulonate, oxymetazoline Chronic: Pus c/s, augmentin+metronidazole, Treat the cause: allergy, surgery(FESS) CT sinuses Epistaxis Most common site – littles area Cause: Idiopathic, trauma (nose picking), dry mucosa, hypertension, coagulopathy, NSAID, Warfarin, tumours Try naseptin cream for a short course Silver nitrate cautery Electrocautery/ packing/ surgery Common Pathology Viral laryngitis Viral URTI preceding aphonia Hx sorethroat B/L V.c. oedema/erythema voice rest, antibiotics Hoarseness Symptom of both local, systemic pathology Often the early symptom of ca larynx Persistent > 2/52 or worsening Associated with loss of weight, smoking, Vocal cord nodules Singer / teacher / children / Often B/L – Junction ant/ middle 1/3 Voice rest / speech therapy Rarely – MLS excision Laryngitis - GORD Hx of GORD Inflammation of Post larynx Treatment for reflux Raising head end of cot Vocal polyp/Reinkes oedema Male Smoker Irritant exposure Hoarseness Dyspnoea Irritant cough Treatment: Voice rest, speech therapy,stop smoking, Microlaryngoscopy and vc stripping Sq papilloma Anterior commissure/ true VC Complete excision Laser treatment Laryngeal Malignancy Risk factors Smoking Alcohol Radiation exposure HPV Nickel exposure Symptoms Hoareseness associated with Dysphagia Odynophagia Otalgia Haemoptysis Signs Dysplasia/Ca in situ Leukoplakia Ulcero/Exophytic growth Neck mass URGENT REFERRAL Cord paralysis Breathy voice (air escape) B/L airway compromise P/H of thyroid, cardiovascular Sx Cord in paramedian position Refer for investigations and treatment Functional aphonia Psychogenic Only able to speak in forced whisper Normal cough Spastic dysphonia strained/strangled voice Onset related to major life stress Hyperadduction of true/false cord Speech therapy, ? Botulinum toxin inj Dysphagia Progressive dysphagia for solids structural lesion Dysphagia for liquids Neurological Painful swallow spasm of cricopharynx, ulcer Signs of reflux Signs of aspiration Examination-key points Oral cavity Tongue, gag reflex,soft palate Pharynx pooling, lesions larynx Elevation of larynx, scopy Neck masses Investigations Ba meal Video fluroscopy Oesophagoscopy Imaging CT/MRI Salivary glands Painful diffuse swelling sailadinitis Plus fluctuation with meals calculi Non painful swelling Tumour Examination Unilateral/bilateral ? Diffuse/well circumscribed? Is it tender? Any discharge from the ducts? Enlarged nodes? Palpable calculi? Investigations Plain X-ray lateral view FNAC CT scan Sialogram Tinnitus SNHL Drugs-NSAID, Aminoglycosides, Antidepressants Tumors- Acoustic neuroma, Temporal lobe tumor Anxiety/ Depression Tinnitus If unilateral refer: MRI Serology: FTA Haematocrit Lipids Audiogram/ ABR Consider hearing therapy referral councilling/ tinnitus masker