CHAPTER 6 :MOOD DISORDERS - BIPOLAR INTRODUCATION
advertisement
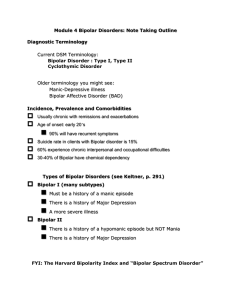
CHAPTER 6 :MOOD DISORDERS - BIPOLAR INTRODUCATION Bipolar disorder is a chronic, recurrent illness that needs a lifelong management Bipolar disorder is characterized by mood swings from profound depression to extreme euphoria (mania), with intervening periods of normalcy It is marked by shifts in the individual's mood, energy, activities, and functions Alternating mood episodes are characterized by mania, hypomania, depression, and concurrent mania and depression (mixed episodes in which depressive symptoms occur during a manic attack) The lifetime prevalence of Bipolar Disorder in the USA is 1.2% - 1.6% but research indicates that it could reach 3% The disorder emerges between the ages of 18 and 30 and can go for years without diagnosis The first episode of the disorder in males is likely to be a manic episode and a depressive episode in females During the course of the illness, the episodes increase in number and severity as the person gets older Periods of normal functioning may alternate with periods of illness (highs, lows, or mixed highs and lows) Studies indicate that 30-60% of Bipolar sufferers fail to regain full occupational and social functioning Many of the Bipolar sufferers experience chronic interpersonal or occupational difficulties during remission It has both high mortality and high morbidity rates compared to Unipolar Disorders It is associated with the highest lifetime rate of suicide of any psychiatric illness Delusions or hallucinations may or may not be a part of the clinical picture Onset of symptoms may reflect a seasonal pattern During a manic episode, the mood is elevated, expansive, or irritable The disturbance is sufficiently severe to cause marked impairment in occupational functioning or in usual social activities or relationships with others or to require Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 1 hospitalization to prevent harm to self or others. Motor activity is excessive and frenzied (furious) Psychotic features may be present A milder representation of this clinical symptom picture is called hypomania Hypomania is not severe enough to cause marked impairment in social or occupational functioning or to require hospitalization, and it does not include psychotic features TYPES OF BIPOLAR DISORDERS: 1. Bipolar I Disorder At least one episode of mania alternating with Major Depression Bipolar I disorder is the diagnosis given to an individual who is experiencing, or has experienced, a full syndrome of manic or mixed symptoms Bipolar I Disorder is found to be more common among males than females The client may also have experienced episodes of depression This diagnosis is further specified by the current or most recent behavioral episode experienced: a) The specifier might be single manic episode (to describe individuals having a first episode of mania) b) Current episode manic, hypomanic, mixed, or depressed (to describe individuals who have had recurrent mood episodes). 2. Bipolar II Disorder Hypomanic episode(s) alternating with Major Depression This diagnostic category is characterized by recurrent bouts of major depression with episodic occurrence of hypomania The individual who is assigned this diagnosis may present with symptoms (or history) of depression or hypomania Bipolar II Disorder is more common among Females Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 2 The client has never experienced an episode that meets the full criteria for mania or mixed symptomatology Patients with Bipolar II Disorder are more likely to become depressed in winter than in summer, and are more likely to make suicidal attempt 3. Cyclothymia Disorder Hypomanic episodes alternating with minor depressive episodes (for at least two years in duration) The essential feature of cyclothymic disorder is a chronic mood disturbance of at least 2-year duration, involving numerous episodes of hypomania and depressed mood of insufficient severity or duration to meet the criteria for bipolar I or bipolar II disorders The individual is never without hypomanic or depressive symptoms for more than 2 months There is a 15% - 50% risk that an individual with Cyclothymia will subsequently develop Bipolar I or Bipolar II Disorder Cyclothymia usually begins in adolescence or early adulthood Rapid Cycling refers to the patient who has four or more mood episodes in a 12month period. It is used to indicate more severe symptoms such as poorer global functioning, high recurrent risk, and resistance to conventional somatic treatments DSM-IV-TR Criteria for Bipolar Disorder A. A distinct period of abnormality and persistently elevated, expansive, or irritable mood for at least: 4 days for hypomania 1 week for mania B. During the period of mood disturbance, three or more of the following symptoms have persisted (four if the mood is only irritable) and have been present to a significant degree: 1. Inflated self-esteem or grandiosity Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 3 2. Decreased need for sleep (the person feels rested after only 3 hours of sleep) 3. More talkative than usual or pressure to keep talking 4. Flight of ideas or subjective experience that thoughts are racing 5. Distractibility (the person's attention is too easily drawn to unimportant or irrelevant external stimuli) 6. Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation 7. Excessive involvement in pleasurable activities that have a high potential for painful consequences (the person engages in unrestrained buying sprees, sexual indiscretions, or foolish business investments) MANIA Definition Mania is an alteration in mood that is expressed by feelings of elation, inflated selfesteem, grandiosity, hyperactivity, agitation, and accelerated thinking and speaking. Mania can occur as a biological (organic) or psychological disorder, or as a response to substance use or a general medical condition Severe enough to cause marked impairment in occupational activities, usual social activities, or relationships. OR Necessitate hospitalization to prevent harm to self or others, or there are psychotic features Symptoms are not due to direct physiological effects of substance (drug abuse, medication) or general medical condition (hyperthyroidism) HYPOMANIA The episode is associated with an unequivocal (unmistakable) change in functioning that is uncharacteristic of the person when not symptomatic Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 4 The disturbance in mood and the change in functioning are observed by others Absence of marked impairment in social or occupational functioning Hospitalization in not indicated Symptoms are not due to direct physiological effects of substance (drug abuse, medication or general medical condition) TREATMENT OF BIPOLAR DISORDERS MOOD-STABILIZING AGENTS Most commonly used Mood Stabilizers: 1. Lithium carbonate: has been for many years the drug of choice for treatment and management of the mania phase of bipolar disorder 2. Anticonvulsants: Valporic Acid, Carbamazepine, Lamotrigine 3. Calcium channel blockers: Verapamil 4. Alpha-2 adrenergics (Colidine) 5. Beta adrenergics (Propranolol) Diagnosis The following nursing diagnoses may be considered for clients receiving therapy with mood-stabilizing agents: Risk for injury related to manic hyperactivity. Risk for self-directed or other-directed violence related to unresolved anger turned inward on the self or outward on the environment. Risk for injury related to lithium toxicity. Risk for activity intolerance related to side effects of drowsiness and dizziness. Planning/Implementation The plan of care should include monitoring for side effects of therapy with moodstabilizing agents and intervening when required to prevent the occurrence of adverse events related to medication administration. Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 5 Be aware of the side effects: 1) Drowsiness, dizziness, and headache: Ensure that client does not participate in activities that require alertness, or operate dangerous machinery. 2) Dry mouth; thirst: Provide sugarless candy, ice, frequent sips of water. Ensure that strict oral hygiene is maintained. 3) GI upset; nausea/vomiting: Administer medications with meals to minimize GI upset. 4) Fine hand tremors: Report to physician, who may decrease dosage. Some physicians prescribe a small dose of beta blocker propranolol to counteract this effect. 5) Hypotension; arrhythmias; pulse irregularities: Monitor vital signs two or three times a day. Physician may decrease dose of medication. 6) Polyuria; dehydration: May subside after initial week or two. Monitor daily intake and output and weight. Monitor skin turgor daily. 7) Weight gain: Provide instructions for reduced calorie diet. Emphasize importance of maintaining adequate intake of sodium Lithium Toxicity The margin between the therapeutic and toxic levels of lithium carbonate is very narrow. The usual ranges of therapeutic serum concentrations are: o For acute mania: 1.0 to 1.5 mEq/L o For maintenance: 0.6 to 1.2 mEq/l Serum lithium levels should be monitored once or twice a week after initial treatment until dosage and serum levels are stable, then monthly during maintenance therapy. Blood samples should be drawn 12 hours after the last dose. Symptoms of lithium toxicity begin to appear at blood levels greater than 1.5 mEq/L and are dosage determinate. Symptoms include: 1) At serum levels of 1.5 to 2.0 mEq/L: Blurred vision, ataxia, tinnitus, persistent nausea and vomiting, severe diarrhea. 2) At serum levels of 2.0 to 3.5 mEq/L: Excessive output of dilute urine, Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 6 increasing tremors, muscular irritability, psychomotor retardation, mental confusion, giddiness. 3) At serum levels above 3.5 mEq/L: Impaired consciousness, nystagmus, seizures, coma, oliguria/ anuria, arrhythmias, myocardial infarction, cardiovascular collapse. Lithium levels should be monitored prior to medication administration. The dosage should be withheld and the physician notified if the level reaches 1.5 mEq/L or at the earliest observation or report by the client of even the mildest symptom. If left untreated, lithium toxicity can be life threatening. Lithium is similar in chemical structure to sodium, behaving in the body in much the same manner and competing at various sites in the body with sodium. If sodium intake is reduced or the body is depleted of its normal sodium (e.g., due to excessive sweating, fever, or diuresis), lithium is reabsorbed by the kidneys, increasing the possibility of toxicity. Therefore, the client must consume a diet adequate in sodium as well as 2500 to 3000 ml of fluid per day. Accurate records of intake, output, and client’s weight should be kept on a daily basis. Client/Family Education (for Lithium) Take medication on a regular basis, even when feeling well. Discontinuation can result in return of symptoms. Not drive or operate dangerous machinery until lithium levels are stabilized. Drowsiness and dizziness can occur. Not skimp on dietary sodium intake. He or she should choose foods from the food pyramid and avoid “junk” foods. The client should drink six to eight large glasses of water each day and avoid excessive use of beverages containing caffeine (coffee, tea, colas), which promote increased urine output. Notify the physician if vomiting or diarrhea occurs. These symptoms can result in sodium loss and an increased risk of toxicity. Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 7 Carry a card or other identification noting that he or she is taking lithium. Be aware of appropriate diet should weight gain become a problem. Include adequate sodium and other nutrients while decreasing the number of calories. Be aware of risks of becoming pregnant while receiving lithium therapy. Use information furnished by health care providers regarding methods of contraception. Notify the physician as soon as possible if pregnancy is suspected or planned. Be aware of side effects and symptoms associated with toxicity. Notify the physician if any of the following symptoms occur: persistent nausea and vomiting, severe diarrhea, ataxia, blurred vision, tinnitus, excessive output of urine, increasing tremors, or mental confusion. Refer to written materials furnished by health care providers while receiving selfadministered maintenance therapy. Keep appointments for outpatient follow-up; have serum lithium level checked every 1 to 2 months, or as advised by physician. Outcome Criteria/Evaluation The following criteria may be used for evaluating the effectiveness of therapy with mood-stabilizing agents: Patient Is maintaining stability of mood. Has not harmed self or others. Has experienced no injury from hyperactivity. Is able to participate in activities without excessive sedation or dizziness. Is maintaining appropriate weight. Exhibits no signs of lithium toxicity. Essentials of Psychiatric Mental Health Nursing 5th Edition - 2012 8