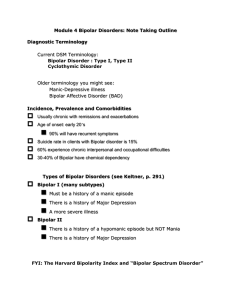
Bipolar I
advertisement

Bipolar Disorders Diagnostic Terminology Bipolar Disorder Bipolar I Bipolar II Old terminology Manic-Depressive Bipolar Affective Disorder Some Facts About Bipolar Illness Usually chronic with remissions and exacerbations Suicide rate in clients with Bipolar disorder is 15% 60% experience chronic interpersonal and occupational difficulties Age of onset: early 20’s 90% will have recurrent symptoms 30-40% of Bipolar have chemical dependency Types of Bipolar Disorder Bipolar I (many subtypes) Bipolar II Must be a history of a manic episode There is a history of Major Depression More severe There is a history of a hypomanic episode but NOT Mania There is a history of Major Depression Cyclothymic Disorder Episodes of hypomania and numerous periods of depressed mood Chronic: Never symptom free Symptoms of HYPOMANIA Similar to Mania But to a Lesser Degree Energetic and driven Excitable Overbearing Highly sociable Intense and volatile emotions Seductive Overspends Motivates others May be highly productive No delusions or hallucinations Hypomania Article NY Times 9/19/10 http://www.nytimes.com/2010/09/19/business/19entre.html?_r=1&scp=1&sq=just%20manic%20Enough&st=Search Signs/Symptoms of MANIA Mood/affect: Euphoric, Labile, Hostile Activity: Hyperactive Thought Processes: Disturbed Unable to concentrate, flight of ideas, tangential Psychotic thought content Too busy to eat or sleep Disorganized activity Delusions: of grandeur or paranoid Hallucinations Pressured speech; hyperverbal Poor judgment and impulse control: with money, sex, any pleasure Loud clothing, excessive make-up Bipolar I: Mixed Episode Meets criteria for both Mania and Major Depression symptoms Severely disturbed, rapidly alternating moods Not caused by other drugs or alcohol May be induced by antidepressant Client is miserable, may be highly suicidal and/or may be violent FYI: The Harvard Bipolarity Index and “Bipolar Spectrum Disorder” www.psycheducation.org Manic Behaviors that Result in Altered Relationships Manipulation Ability to find vulnerability in others Exploit weaknesses and create conflict Ability to shift responsibility Limit testing Alienation of family--may be aggressive and abusive Etiology: Biologic Theories Ion dysregulation: causes oversensitivity of neuron to stimuli Alteration in transcription of messengers in nerve cell nucleus Neurotransmitters involved in mania/bipolar: Excessive Dopamine and Norepinephrine availability of GABA and Serotonin Nursing Diagnoses (for Mania) Risk for Violence (Directed toward self, others) Insomnia Altered Nutrition: Less than Body Requirements Acute Confusion Disturbed Thought Processes Impaired Social Interaction Psychotherapeutic Management (Focus of presentation is primarily on management of mania except where otherwise noted) Nurse-Client Relationship and Milieu Management Matter-of-Fact Tone Clear, concise directions Limit Setting De-escalating the client Maintaining Safety Consistency among staff Reduction of environmental stimuli Milieu Management, cont’d Reinforcing appropriate hygiene and dress Supporting adequate Nutrition and Sleep Providing activities for excessive energy PSYCHOTHERAPEUTIC MANAGEMENT: MEDICATIONS Medications A Common Diagnostic Mistake Diagnosing Major Depressive Disorder when the client is in the Depressive Aspect of Bipolar Disorder Giving an antidepressant can push the client into Mania Antipsychotics All Atypicals: olanzepine: Zyprexa, quetiapine: Seroquel, ziprasidone: Geodon, risperidone: Risperdal and Risperdal Consta, aripiprazole: Abilify are FDA approved mood stabilizing agents. Used alone or with other mood stabilizing agents Other antipsychotics: used prn for agitation Lithium Mechanism of action unknown: similarity to action of Na /replaces Na in the body Slow onset: 2 weeks Narrow range of therapeutic level: 0.6 to 1.2 mEq/L; the optimum maintenance level is 0.8 mEq/L Toxic over 1.5 mEq/L “Normal side effects”- weight gain, fine hand tremor, nausea, metal taste Lithium Toxicity Narrow therapeutic range: therapeutic dose is close to a toxic dose. Mild to Moderate toxic reactions: 1.5 to 2 mEq/L Diarrhea Vomiting Drowsiness Muscular weakness Lack of coordination Dry mouth Lithium Toxicity Moderate to Severe reactions 2 to 3 mEq/L All previous symptoms & Ataxia Tinnitus Blurred vision High urinary output (osmotic diuresis) Delirium Nystagmus Lithium Toxicity Severe reactions: than 3 mEq/L All previous symptoms Seizures Organ failure Renal failure Coma Death Mood Stabilizing Medications: Anticonvulsants valproic acid/divalproex: Depakote and Depakene carbamazepine: Tegretol Side effects: many drug interactions; CNS effects; blood disorders ( RBC, bone marrow, WBC’s), liver failure; toxic reactions common Other Anticonvulsants topiramate: Topamax gabapentin: Neurontin oxcarbazepine: Trileptal lamotrigine: Lamictal-best for bipolar depression. May cause severe rash. Benzodiazepines Good for acute mania and psychomotor agitation in mania Used in acute care settings; not for long term tx. clonazepam (Klonopin) lorazepam (Ativan) Nursing Implications: Lithium What will the nurse do if a patient shows behaviors/symptoms of what looks like lithium toxicity? A. Stop/hold the medication B. Draw a lithium level, then hold the medication C. Stop/hold med., then draw a lithium level D. Draw a lithium level, keep giving the med. until results are in. Nursing Implications: Mood Stabilizing Medications What are nursing interventions for the client a) starting on, or b) being maintained on Lithium? -Labs -Other testing -Ongoing assessments What client teaching would the nurse perform for the client, family?