Charles Hoopes, MD - American Heart Association
advertisement

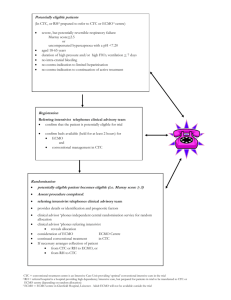
Veno-arterial ECLS for cardiogenic shock STS Symposium: Mechanical Circulatory Support for Advanced Cardiopulmonary Disease September 2013 Chicago I have no financial interests in any of the technologies discussed and nothing to disclose Charles Hoopes MD University of Kentucky Questions & learning objectives…ECLS & cardiogenic shock Is “salvage” ECLS in the patient with cardiopulmonary collapse an evidence based approach … the clinical rationale for and clinical limitations of ECMO What are the physiological goals of ECLS in cardiogenic shock … what are the biological and clinical markers of success ? How does “emergent” ECLS in the patient with cardiogenic shock change the options and the risk profile of subsequent durable LVAD implantation and transplant ? “Our interventionists had a case recently where patient had a LAD PCI then was brought back a couple of days later for a RCA mid lesion. She arrested on insertion of the catheter in the aortic root -- never did a manipulation -- and after initial unsuccessful resuscitation, placed an impella and kept it up. They injected her L and it was open and, while still arrested opened the mid RCA. They called us after about 45 min of arrest when she was still in asystole. We then had ECMO there but by then it was an hour of arrest with no rhythm and felt ECMO would be futile. Do you have or know of any experience that would justify a trial of ECMO in this situation. I could understand if it was a bridge to recovery with severe shock, but with a rhythm -- or if there was a L main or other proximal lesion to open.” veno-arterial ECMO/ECLS ? 41 yo male Vfib arrest (in house) … total occlusion LAD. Acute thrombosis of RCA during LAD PCI … ventricular arrhythmias with cardioversions x 16. IABP and Impella 2.5 … transferred to ICU with patent LAD, recurrent thrombosis of RCA (100% mid), inotropes. Clotting diathesis … ? 24 hours post cath … CI 1.6, Cr 5.5, AST > 5000, lactate > 6 …Q’s in II, III, aVF … trops > 50. Adequate gas exchange … Return to cath lab … patent LAD, 100% mid RCA … Vfib veno-arterial ECMO/ECLS ? “Defibrillation was attempted again but remained unsuccessful. CPR continued. We suspected that the patient’s heart was too distended to permit termination of ventricular fibrillation … a decision was made to consult cardiac surgery about the initiation of extracorporeal membrane oxygenation (ECMO) for full hemodynamic support and to decompress the heart and facilitate termination of ventricular fibrillation.” n engl j med 369;11 nejm.org september 12, 2013 Pubmed search: “ECMO and cardiogenic shock” … 403 citations (60% w/in the past 60 months) … the large randomized IABP-Shock II Trial did not show a significant reduction in 30-day mortality in cardiogenic shock with IABP insertion. … both the Impella pump and the Tandem Heart did not reduce 30day mortality when compared with IABP in small randomized controlled trials … no randomized study data available for ECMO/ECLS use in cardiogenic shock Trends in the incidence rates of cardiogenic shock in patients with acute myocardial infarcts. Goldberg et al. Thirty-year trends (1975 to 2005) in the magnitude of,management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction Circulation 2009;119:1211 1 in 20 Trends in hospital case fatality rates in patients with acute myocardial infarct according to the presence of cardiogenic shock. 40% Is ECLS the answer ? 30% survival to discharge ! ELSO Registry Jan 2010 Among 98 patients … cardiogenic shock (34), ventricular fibrillation or pulseless ventricular tachycardia (23), or asystole /pulseless electrical activity (41) 96% underwent emergency revascularization (2 received CABG) with successful angioplasty achieved in 71% (TIMI 3 flow) 55% were weaned from ECLS … ECLS-related complications occurred in 36%... cannulation site bleeding All-cause in-hospital mortality rate was 67.3%, and the survival rate to hospital discharge was 32.7% “ …disappointing results for the sole use of ECLS … aggressive initiation of ECLS could improve survival rates to 70% to 80% … the reason for cardiac surgeons to understand its lessons: Prolonged cardiogenic shock carries a high mortality without a plan for definitive additional therapy Revascularization in the setting of cardiogenic shock provides little or no additional benefit and in the short term may be detrimental by delaying definitive support ECLS is an effective method of early resuscitation of the moribund patients in shock … its effectiveness depends on end organ ischemic time, early ventricular recovery, or use of more definitive devices for long-term support” Invited Commentary George L Hicks, MD University of Rochester Medical Center “ECMO in advanced refractory AMICS is associated with acceptable outcomes in a well-selected population. ischemic 50% at 6 mos non-ischemic 20% ECMO in patients with an acute decompensation of a chronic cardiomyopathy should be carefully considered to avoid futile support.” Kaplan-Meier survival curve of all patients supported on ECMO for cardiogenic shock (subsequent management strategies included revascularization, VAD, or heart transplantation) Bermudez et al (2011) ECMO for advanced refractory shock in acute and chronic cardiomyopathy. AnnThorac Surg 92:2125 Cannulation and initiation of flow … vascular access, gas exchange , and flow Do what you need to get what you want … perfusion w/o ischemia adequate hemodynamics “viable patient” Engineering should inform the discussion around patient care … “Thought algorithms” vs “protocols” ECMO: simple operation, complex procedure “Truisms” about ECLS/ECMO … ECMO resuscitates the moribound … it cannot reanimate the dead … question of patient viability or myocardial recovery ECMO remains a non-durable technology … ECLS is a simple procedure, extracorporeal technologies are a complex management paradigm ECLS accomplishes nothing (it is non-therapeutic), but facilitates everything Two types of ECMO/ECLS program … public health perspective … clinical goals define infrastructure (technology and personnel) Acute stabilization and short term transfer “moratorium of decision” programs (in house … cath lab, ED, OR) duration of support < 72 hrs, limited infrastructure rapid deployment technology (non-durable technologies) Integrated programs (ICU and/or transplant) “recovery” and “bridge to transplant” (referral based) duration of support > 72 hrs, extended infrastructure (MCS) durable technologies (“ambulatory ECMO”) … institutional culture and hospital structure impact on ECLS program design The 30-day mortality rate in patients with witnessed OHCA undergoing ECLS treatment can be significantly improved if ECLS support is established within the first 30 min after admission …rdECMO Leick et al (2013) Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin Resarch Cardiol 102:661. Sheu et al (2010) ECMO assisted primary percutaneous coronary intervention improved 30-day clinical outcomes in patients with ST-segment elevation myocardial infarction complicated with profound cardiogenic shock. Crit Care Med 38:1810. Basic ECMO… Cannulation...clinical need determines strategy femoral vein to IJ (traditional VV) femoral vein to femoral artery (traditional VA) femoral vein and RIJ to femoral artery (VVA) RIJ dual lumen and subclavian artery (“walking hybrid”) RA to Ao (central VA)..”ambulatory CPB” (VAD) RA to PA…right heart bypass (VAD) PA to LA…right heart bypass (VAD) RIJ dual lumen cannula (VV Avalon DLC) RIJ dual lumen and femoral artery (VVA “sedate hybrid”) femoral artery to RA (AV) …reverse “pumpless” arterio-venous cannulation (pECLA) Membrane oxygenator (Quadrox) Centrifugal blood pump (Centrimag or Rotaflow), roller pump, or “native flow” (cardiac output) Anticoagulation (heparin ACT “point of care”, TEG) Personnel (MCS service line or ECMO specialists) Cardiopulmonary collapse (circulatory arrest) CPR “salvage” ECLS “moratorium of decision” … end organ injury “bridge to recovery” … myocardial injury (…application and deployment) “bridge to definitive therapy” … non-durable to durable support “emergent” ECLS Cardiogenic shock (INTERMACs I) Cannulation … Peripheral veno-arterial ECLS RA/femoral vein…retrograde femoral a. (ECMO) RA…antegrade right subclavian a. (8mm Dacron graft/ECMO) LA/femoral trans-septal …retrograde femoral a. Central veno-arterial ECLS RA to pulmonary a. (right heart) LA to aorta (VAD) RA to aorta (ECMO) (…application and deployment) Femoral cannulation for veno-arterial (VA) ECMO … RA/IVC drainage from CFV access (23/25F) …venous return limits flow Arterial inflow (17F) … “downsize” Distal arterial inflow (6F) … “downsize” …“open” versus “percutaneous” access ? *no complications *exit strategy VAda ECMO VenoArterial (distal artery) ECMO Non physiologic and inherently unstable Efficacy proportional to LVEF Retrograde arterial flow … LVEF and cerebral perfusion, LVEDP ! Distal malperfusion … The patient … sedate and non-ambulatory Blood path and directional flow … Aziz et al (2010) Initial experience with CentriMag extracorporal membrane oxygenation for support of critically ill patients with refractory cardiogenic shock JHLT 29:66 Determine blood flow requirements … Neonate Pediatric Adult 100 to 150 mL/min/kg 75 to 120 mL/min/kg 50 to 80 mL/min/kg Assumptions: “flow is laminar viscous and incompressible …and the flow is through a constant circular cross-section …” In reality: Flow is rarely laminar … Hct and temp affect viscosity … The cross sectional area is a composite of fixed (cannula) and variable (vessels) components …standardized system to describe the pressure-flow characteristics of a given cannula … if specific flows are needed to support a given patient, an arterial and venous cannula of an adequate Mnumber can be chosen from a given nomogram that will support flow at acceptable pressures A single number that represents the relationship between cannula size, flow, and pressure drop. M-number for tubing: 1/4 inch, 1 meter M= 3.1 3/8 inch, 1 meter M= 2.0 1/2 inch, 1 meter M= 0.9 Assuming non-turbulent blood flow M-number : resistance Cannulation … 16F 18F 20F 22F 18F 20F 22F 24F 28F (6.0mm) (6.7mm) (7.3mm) (8.0mm) (9.3mm) 55 cm (21.6”) 68 cm (26.8”) (5.3mm) (6.0m (6.7mm) (7.3mm) Femoral VA ECMO … low EF non-physiological: retrograde blood path with limited pulmonary blood flow (oxygenator) decreased LV pre-load … myocardial recovery increased LVEDP … capillary leak and acute lung injury gas exchange … membrane oxygenator cannulation … limb ischemia This is not cardiopulmonary bypass … there is no venous reservoir Veno-arterial ECLS in cardiogenic shock VA ECMO is not CPB … any decrease in pre-load is at the expense of increased afterload Left ventricular stasis … elevated LVEDP with pulmonary edema and LV thrombus RV Vent, apical cannulation, septostomy, anticoagulation, or.. “hybrid procedure” … VA ECMO and antegrade technology Acute lung injury after mechanical circulatory support implantation in patients on extracorporeal life support: an unrecognized problem. Boulatea et al (2013) European Journal of Cardio-Thoracic Surgery 44: 544–550 Femoral VA ECMO … with myocardial recovery limited retrograde blood path with significant pulmonary blood flow (oxygenator) increased LV pre-load … myocardial recovery decreased LVEDP … no lung injury gas exchange … mixed …membrane oxygenator and lungs cannulation … lower limb ischemia Management algorithms are complicated by inadequate predictors of myocardial recovery … ECHO and markers of perfusion Mean arterial pressure Veno-arterial ECLS targeted flow rates … 90 Cardiac power output > 0.6 80 70 60 50 CPO = MAP x CO/451 3.0 Cardiac output (L/min) 5.5 RIJ-subclavian VA ECMO antegrade blood path with significant pulmonary blood flow (oxygenator) increased LV pre-load … myocardial recovery decreased LVEDP … 8mm Dacron gas exchange … mixed …membrane oxygenator and lungs cannulation … upper limb ischemia RA Subclavian Artery Cannulation for Venoarterial Extracorporeal Membrane Oxygenation. Javidfar, Jeffrey; Brodie, Daniel; Costa, Joseph; Miller, Joanna; Jurrado, Julissa; LaVelle, Matthew; Newmark, Alexis; Takayama, Hiroo; Sonett, Joshua; Bacchetta, Matthew ASAIO Journal. 58(5):494-498, September/October 2012. DOI: 10.1097/MAT.0b013e318268ea15 RIJ dual lumen VV-subclavian Arterial ECMO … hybrid ECMO (venoveno-arterial) antegrade flow … mixed cardiopulmonary disease “hybrid” VVA, or full VV, or full VA support technology … not salvage ambulatory 8mm Dacron RA Brodie and Bacchetta (2011) NEJM …percutaneous approach … trans-septal left ventricular unloading Evolving applications … “virtual VVA ECMO” cor pulmonale and pulmonary veno-occlussive disease 68 yo scleroderma variant, elevated ANA…supra-systemic PA pressures on continuous dobutamine, lasix qtt, high flow O2. Failed vasodilator therapy x 3…non-ambulatory with progressive syncopal episodes… To cath lab…combined atrial septostomy and right IJ dual lumen venovenous ECMO cannulation…bridge to transplant (ECMO day 4) Cannulation … Peripheral veno-arterial ECLS RA/femoral vein…retrograde femoral a. (ECMO) RA…antegrade right subclavian a. (8mm Dacron graft/ECMO) LA/femoral trans-septal …retrograde femoral a. Central veno-arterial ECLS RA to pulmonary a. (right heart) LA to aorta (VAD) RA to aorta (ECMO) (…application and deployment) Central cannulation … Central cannulation … PA LA … integrated MCS ECMO cardiogenic shock … femoral ECMO … to central ECMO … to LVAD and oxyRVAD with RV failure… to long-term Centrimag RVAD support … bridge to transplant Cannulation and initiation … ten general rules and painful lessons 1. re-think “application” … why am I doing this and what do I hope to accomplish 2. re-think “deployment” … “this” cannulation strategy … “now?” 3. Got heparin ? (0.5 mg/kg) … plan an anticoagulation strategy 4. Crystalloid prime … or colloid prime (FFP) 5. Look at your lines … air, clamps, length, and entry points 6. Come up slowing … establish flow, then increase flow 7. Remember the patient … inotropes and airway (minute ventilation is 15L/min … sweep is 10L ...!!!) 8. Most disasters happen five minutes after the celebration begins .. This is a human endeavor 9. Any surgical bleeding is unacceptable 10. Have an exit strategy … mortality assessment of preoperative risk factors that might serve as targets for goal-directed interventions meant to improve LVAD candidate survival (age, albumin, renal and hepatic insufficiency, center experience) Low risk < 1.58 Medium risk: 1.58 to 2.48 High risk > 2.48 Cowger et al (2013) Predicting Survival in Patients Receiving Continuous Flow Left Ventricular Assist Devices:The HeartMate II Risk Score. J Am Coll Cardiol. 61:313–21 “… preserved end-organ function, however preoperatively achieved, might be the most important predictor of successful LVAD outcome.” bilirubin lactate RVAD AST ECMO RVAD explant Can pre-operative ECMO alter the patient risk profile of LVAD implantation … Or does it simply make the numbers better… with the additional morbidity of a pre-implant procedure? LVAD Na Cr Creatinine ECLS LVAD The Right Ventricular Failure Risk Score (RVFRS): A pre-operative tool for assessing the risk of right ventricular failure in left ventricular assist device candidates Vasopressor requirement (4) AST > 80 (2) Bilirubin > 2 (2.5) Cr > 2.3 (3) AST Low risk (OR 0.5) survival) High risk (OR 7.6) survival) RVFRS < 3 (90% six mo RVFRS > 5.5 (66% six mo Pre ECMO RVFRS score … 11.5 Post ECMO RVFRS score … 2.5 Bilirubin Can pre-operative ECMO convert a patient at high risk for biventricular support into a “conventional” LVAD recipient? Matthews at al (2008) JACC 51:2163 ECLS and cardiogenic shock… Deployment of ECMO technologies in the context of medical futility generally results in futile deployment of technology…it is rarely “the device” ECMO technology generally restores physiology but may not alter survival depending upon the specifics of deployment ECMO can support patients awaiting good clinical decision making … it is ineffective in supporting bad clinical decisions