Emory University Department of Gynecology & Obstetrics
advertisement
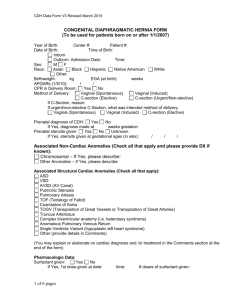
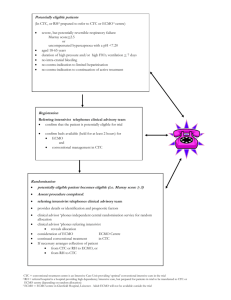
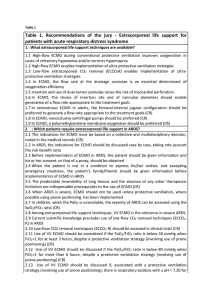
Pediatric Surgery A. Tubbs TY 7263849 1 35 week 2.2kg infant with known L CDH to a 30 year old G6 P4 AA female via SVD Intubated at 7 minutes of birth when she became apneic. Initially on minimal vent settings in NICU without need for ECMO. DOL 2 hypotension and bradycardia requiring pressor support and continued to worsen over the next two days DOL 5 ECMO, stabilized Day 8 ECMO dramatically worsened with white out on the CXR and never recovered Day 14 R chest tube placed for effusion, 50ml serous drainage, minimal improvement Day 15 overnight flows gradually decreased, O2 sat in 20’s for several hours, coded as changing the circuit Stabilized over the weekend DOL 22/ ECMO Day 18 proceeded with L CDH repair on ECMO with gortex patch Agenesis of the entire left hemidiaphragm except small anterior rim Entire bowel in the chest with minimal lung tissue Heparin bleeding Chest tube and skin only closure Actively resuscitated all night and POD 1 with ~700ml from chest tube POD 2 hypotension requiring max doses of dopamine and dobutamine, anuria Withdrawal of care TY 7263849 3 Analysis of Complication 14 • Was the complication potentially avoidable? – • Would avoiding the complication change the outcome for the patient? – • No Yes What factors contributed the complication? – Patient disease – – – – Agenesis of the diaphragm Minimal good lung tissue Prematurity ECMO/Heparin Congenital Diaphragmatic Hernia 15 Malformation of the diaphragm allowing bowel to herniate into the thoracic cavity before birth resulting in pulmonary hypoplasia and pulmonary hypertension Most are left sided and are associated with malrotation ~50% of survivors are treated with ECMO Overall survival rate is 60%, less with prematurity Delayed repair 6 Survival in early- and late-term infants with congenital diaphragmatic hernia treated with ECMO. Stevens TP, Chess PR, et al. Pediatrics. 2002 Sep;110(3):590-6. Retrospective cohort study of all infants in the ELSO registry placed on ECMO over past 25 yrs Early term 38-39w, Late term 40-41w 53% v 63% survival rate, shorter ECMO duration, shorter hospital stay and fewer complications 7 Cardiac arrest before repair or ECMO cannulation does not increase the mortality rate associated with CDH. Courcoulas AP, Reblock KK, Rowe MI, Ford HR. J Pediatric Surg. 1997 Jul;32(7):952-6. Retrospective review 119 infants 21 suffered arrest before repair or cannulation No sign difference in birth wts, GA, race/gender, preg/delivery complications Significant number of those that arrested required ECMO for prolonged time No sign difference in overall survival 8 Factors associated with survival in infants with CDH requiring ECMO: a report from the CDH study group. Seetharamaiah R, et al. J Pediatric Surg. 2009 Jul;44(7):1315-21. 3100 children Survivors: Greater gestational age Greater birth weights Less often prenatally diagnosed Required ECMO for shorter period of time (9 +/- 5 v. 12 +/- 5) Take Home Points 18 Delayed repair of CDH 50% CDH infants require ECMO Survival rate ~60%, decreased with decreased gestational age and birth weight Shorter duration of ECMO associated with improved survival Not optimal to repair on ECMO