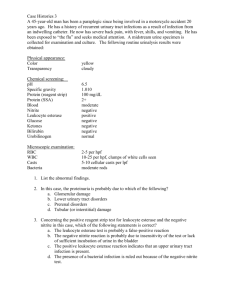
Day 3 TP, Blood, Nitrate, pH Self UA
advertisement

Day 3 Self Urinalysis TP, Blood, Nitrate & pH Urine pH • Lungs and kidneys are major regulators of acidbase content • First morning specimen slightly acidic at 5.0 to 6.0 • Postprandial specimen more alkaline • Normal range is 4.5 to 8.0 • No absolute values are assigned Urine pH (cont’d) • Considerations include – Acid-base content of the blood – Patient’s renal function – Presence of a urinary tract infection – Patient’s dietary intake – Age of the specimen • A pH above 8.5 is associated with an aged/improperly preserved specimen, so a fresh specimen should be obtained Summary of Clinical Significance of Urine pH • Respiratory or metabolic acidosis/ketosis • Respiratory or metabolic alkalosis • Defects in renal tubular secretion and reabsorption of acids and bases—renal tubular acidosis • Renal calculi formation • Treatment of urinary tract infections • Precipitation/identification of crystals • Determination of unsatisfactory specimens pH-Reagent Strip Reactions • Needed to measure between 5.0 and 9.0 in one half or one unit increments • Double-indicator system reaction – Methyl red = 4 to 6 red/orange to yellow – Bromthymol blue = 6 to 9 green to blue Methyl red + H+ → Bromthymol blue − H+ (Red/Orange → Yellow) (Green → Blue) • Interference – No known substances interfere with urinary pH measurements performed by reagent strips – RUNOVER from Protein Protein • Most indicative of renal disease – Proteinuria seen in early renal disease • Normal = <10 mg/dL or 100 mg/24 h • Low-molecular-weight serum proteins are filtered; many are reabsorbed • Albumin is primary protein of concern • Other proteins include – Vaginal, prostatic, and seminal proteins – Tamm-Horsfall (uromodulin) Clinical Significance • Presence requires determination of normal or pathological condition • Clinical proteinuria = 30 mg/dL, 300 mg/24 h • Variety of causes – Prerenal – Renal – Postrenal Prerenal Proteinuria • Conditions affecting the plasma, not the kidney • Transient, increase levels of low-molecularweight plasma proteins, acute phase reactants, exceed reabsorptive capacity • Rarely seen on reagent strip (not albumin) Bence Jones Protein (BJP) • Multiple myeloma (plasma cell myeloma) • Immunoglobulin light chains • Multiple myeloma confirmation is serum electrophoresis Renal Proteinuria • Glomerular or tubular damage – Glomerular proteinuria – Microalbuminuria – Orthostatic (postural) proteinuria – Tubular proteinuria Glomerular Proteinuria • Damage to glomerular membrane • Impaired selective filtration causes increased protein filtration leading to cellular excretion • Abnormal substances deposit on the membrane – Primarily immune disorders result in immune complex formation • Lupus erythematosus, streptococcal glomerulonephritis – Amyloids and other toxins Blood • Hematuria: intact RBCs – Cloudy red urine • Hemoglobinuria: product of RBC destruction – Clear red urine • Any amount of blood greater than five cells per microliter of urine is considered clinically significant • Chemical tests for hemoglobin provide the most accurate means for determining the presence of blood • The microscopic examination can be used to differentiate between hematuria and hemoglobinuria Blood (cont’d) • Hematuria: intact RBCs, cloudy red urine • Damage to renal system – Renal calculi – Glomerular disease – Tumors – Trauma – Pyelonephritis – Exposure to toxic chemicals – Anticoagulants Blood (cont’d) • Hemoglobinuria: clear, red urine – – – – – – Transfusion reactions Hemolytic anemias Severe burns Infections/malaria Strenuous exercise/RBC trauma Brown recluse spider bites • Hemoglobinuria may result from the lysis of red blood in dilute, alkaline urine • Hemosiderin: yellow brown granules in sediment Blood (cont’d) • Myoglobinuria: heme-containing protein in muscle tissue; clear, red/brown urine – Rhabdomyolysis: muscle destruction • • • • • • • • Muscular trauma/crush syndromes Prolonged coma Convulsions Muscle-wasting diseases Alcoholism Drug abuse Extensive exertion Cholesterol-lowering statin medications Blood Reagent Strip Reactions • Principle pseudoperoxidase activity of hemoglobin • Catalyze a reaction between the heme component – Hemoglobin and myoglobin – Chromogen tetramethylbenzidine – Produce an oxidized chromogen • Green-blue color Blood Reagent Strip Reactions hemoglobin H2O2 + chromogen --------------- oxidized chromogen + H2O peroxidase • Two charts corresponding to different reactions • Free hemoglobin shows uniform color • Intact RBCs show a speckled pattern on pad – Report: trace, small (1+), moderate (2+), large (3+) – Sensitivity 5 RBCs/μL Blood Reaction Interference • False-positive – Menstrual contamination, strong oxidizing agents, bacterial peroxidases • False-negative – Ascorbic acid >25 mg/dL – High SG/crenated cells – Formalin – Captopril – High concentrations of nitrite – Unmixed specimens Nitrite • Clinical significance • Rapid screening test for the presence of urinary tract infection (UTI) – – – – Cystitis (initial bladder infection) Pyelonephritis (tubules) Evaluation of antibiotic therapy Monitoring of patients at high risk for urinary tract infection – Screening of urine culture specimens (in combination with LE test) Nitrite Reagent Strip Reaction • Tests ability of bacteria to reduce nitrate (normal constituent) to nitrite (abnormal) • Greiss reaction: nitrite reacts with aromatic amine to form a diazonium salt that then reacts with tetrahydrobenzoquinoline to form a pink azodye • Correspond with a quantitative bacterial culture criterion of 100,000 organisms/mL • Results: negative and positive Nitrite Reagent Strip Reaction (cont’d) Acid para-arsanilic acid or sulfanilamide + NO2 —————→ diazonium salt (nitrite) Acid diazonium salt + tetrahydrobenzoquinolin —————→ pink azodye Nitrite Reaction Interference • False-negative – – – – – – – – Nonreductase-containing bacteria Insufficient contact time between bacteria and urinary nitrate Lack of urinary nitrate Large quantities of bacteria converting nitrite to nitrogen Presence of antibiotics High concentrations of ascorbic acid High specific gravity Negative results in the presence of even vaguely suspicious clinical symptoms should always be repeated or followed by a urine culture Nitrite Reaction Interference (cont’d) • False-positive – Old specimens (bacterial multiplication) – Highly pigmented urine – Pink edge or spotting on reagent strip is considered negative – Check automated readers manually for color interference