PowerPoint File - American College of Cardiology
advertisement

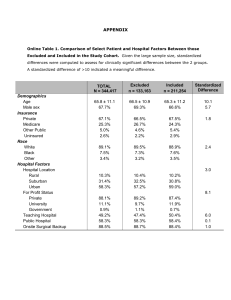
Appropriate Use Criteria for Coronary Revascularization and Trends in Utilization, Patient Selection and Appropriateness of Percutaneous Coronary Intervention Nihar R. Desai, MD, MPH; Steven M. Bradley, MD, MPH; Craig S. Parzynski, MS; Brahmajee K. Nallamothu, MD, MPH; Paul S. Chan, MD, MSc; John A. Spertus, MD, MPH; Manesh R. Patel, MD; Jeremy Ader, AB; Aaron Soufer, MD; Harlan M. Krumholz, MD, SM; Jeptha P. Curtis, MD Funding Support and Disclaimer This research was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR). The views expressed in this presentation represent those of the author(s), and do not necessarily represent the official views of the NCDR or its associated professional societies identified at www.ncdr.com. Disclosures Drs. Desai and Krumholz are recipients of a research agreement from Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing. Drs. Desai, Krumholz and Curtis receive funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting. Dr. Krumholz receives research support from Medtronic, through Yale University, to develop methods of clinical trial data sharing and of a grant from the Food and Drug Administration to develop methods for post-market surveillance of medical devices. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth. Dr. Spertus discloses funding from the American College of Cardiology to analyze the NCDR registries, membership on the United Healthcare cardiac scientific advisory board and an equity interest in Health Outcomes Sciences. Dr. Patel has research grants through Duke University with Johnson and Johnson, AstraZeneca, Maquet, National Heart Lung and Blood Institute, AHRQ, and is on the Advisory Board for Bayer Healthcare, Jansen, and Genzyme. Dr. Curtis discloses equity interest in Medtronic. No other disclosures were reported. Dr. Desai is supported by grant K12 HS023000-01 from the Agency for Healthcare Research and Quality. Drs. Krumholz and Curtis are supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr. Bradley is supported by a Career Development Award (HSR&D-CDA2 10-199) from Veterans Affairs Health Services Research and Development. This research was supported by the NCDR. The analytic work for this investigator-initiated study was performed by the Yale Center for Outcomes Research and Evaluation Data Analytic Center with financial support from the American College of Cardiology. Background • The Appropriate Use Criteria (AUC) for Coronary Revascularization were developed to critically examine and improve patient selection for PCI as well as address concerns about potential overuse. • Previous studies have demonstrated that 1 in 6 PCIs performed for nonacute indications were classified as inappropriate with substantial variation in performance across hospitals. • Reducing the number of inappropriate PCIs became and remains a priority for national performance improvement initiatives. • Despite the attention this topic has received, the quality improvement initiatives that have been launched in response, and the implications for health care quality and spending, there has been no national examination of trends in patient selection and appropriateness of PCI following the introduction of the AUC. Study Aims 1. Examine national trends in the characteristics of patients undergoing PCI between July 2009 and December 2014. 2. Evaluate trends in the appropriateness of PCI over the study interval. 3. Identify the presence and extent of hospital-level variation in inappropriate PCI. AUC Methods Overview • The AUC synthesize clinical trial evidence, practice guidelines, and expert opinion to determine procedural appropriateness based upon: 1. Clinical indication (i.e. acute or non-acute); 2. Angiographic findings; 3. Magnitude of ischemia on non-invasive testing; 4. Severity of anginal symptoms; and 5. Intensity of background medical therapy, AUC Rating Coronary revascularization likely to improve patient’s health status and/or outcomes Appropriate (Appropriate) Uncertain (Maybe Appropriate) Inappropriate (Rarely Appropriate) + +/- - Methods • Study population: All patients undergoing PCI between July 1, 2009 and December 31, 2014 at hospitals continuously participating in NCDR CathPCI Registry and performing at least 10 non-acute PCIs each year. • Primary Outcome: Proportion of non-acute PCIs classified as inappropriate at the patient- and hospital-level using the 2012 AUC. • Statistical analysis plan: – PCI volume and the relative proportions of acute, non-acute, and non-mappable PCIs were examined over time. – Baseline demographic and clinical characteristics were compared among those undergoing non-acute PCI over time. – The proportions of appropriate, inappropriate, and uncertain nonacute PCIs at the patient-level were calculated for each 6-month interval and compared over time. The proportion of non-acute PCIs considered inappropriate at the hospital level was calculated by aggregating all non-acute PCIs in the calendar year. Study Population Percutaneous coronary interventions between July 1, 2009 and December 31, 2014 submitted to NCDR CathPCI Registry (n=3,604,365; 1561 hospitals) Final Study Cohort (n=2,685,683; 766 hospitals) Exclusions • Hospital did not participate in NCDR CathPCI registry over the entire study period (n=550,836; 583 hospitals) • Hospital with an average of fewer than 10 non-acute PCIs per year (n=273,167; 212 hospitals) • Second PCI if multiple PCIs in a single visit (n=94,679) Trends in Indication for PCI PCI indication/Year Overall 2009* 2010 2011 2012 2013 2014 Overall, n 2,685,683 243,580 538,076 502,995 481,889 462,636 456,507 Acute, n (%) 2,047,853 (76.3) 168,366 (69.1) 377,540 (70.2) 373,423 (74.2) 380,331 (78.9) 373,650 (80.8) 374,543 (82.0) Non-acute, n (%) 397,737 (14.8) 41,024 (16.8) 89,704 (16.7) 78,328 (15.6) 66,849 (13.9) 62,457 (13.5) 59,375 (13.0) Non-mappable, n (%) 240,093 (8.9) 34,190 (14.0) 70,832 (13.2) 51,244 (10.2) 34,709 (7.2) 26,529 (5.7) 22,589 (4.9) *Includes 6-months of data (July 1 to December 31, 2009) Changes in Baseline Characteristics Among Patients Undergoing Non-acute PCI # 89,704 % 22.6 # 59,375 % 14.9 Absolute Change from 2014-2010 # % -30,329 -7.7 26,313 47,710 15,681 29.3 53.2 17.4 12,890 23,689 22,796 21.7 39.9 38.4 -13,423 -24,021 +7,115 -7.6 -13.3 +21.0 27,076 42,610 20,011 30.2 47.5 22.3 11,521 27,031 20,816 19.4 45.5 35.1 -15,555 -15,579 +805 -10.8 -2.0 +12.8 10,328 33,468 12,460 39,231 18.4 59.5 22.2 43.7 4,708 23,475 14,018 28,192 11.2 55.6 33.2 47.5 -5,620 -9,993 +1,558 -11,039 -7.2 -3.9 +11.0 +3.8 2010 Patient Characteristics N Angina No symptoms CCS I or II CCS III or IV No. of antianginal medications 0 1 >=2 Stress test results (among those with a test) Unavailable Low or intermediate risk High risk Multi-vessel CAD on angiography 2014 Patient-level Trends in Appropriateness of Non-acute PCI 100 90 Non-acute PCIs, % 80 70 60 50 Uncertain 40 Appropriate 30 Inappropriate 20 10 0 2009* 2010 *Includes July to December 2009 2011 2012 Year 2013 2014 Patient-level Trends in Appropriateness of Non-acute PCI 100 90 Non-acute PCIs, % 80 70 60 Appropriate 50 40 Uncertain 30 20 Inappropriate 10 0 2009* 2010 *Includes July to December 2009 2011 2012 Year 2013 2014 Patient-level Trends in Appropriateness of Non-acute PCI 100 90 Non-acute PCIs, % 80 70 60 Appropriate 50 40 Uncertain 30 20 Inappropriate 10 51% relative reduction, p<0.001 0 2009* 2010 *Includes July to December 2009 2011 2012 Year 2013 2014 Non-acute PCIs classified as inappropriate, % Hospital-level Trends in Inappropriate Non-acute PCIs 100 90 80 70 60 50 40 30 20 10 0 2009* Median (IQR) 2010 2011 2012 25.8 (16.7-37.1) Year *Includes July to December 2009 2013 2014 Non-acute PCIs classified as inappropriate, % 100 Hospital-level Trends in Inappropriate Non-acute PCIs 90 80 70 60 50 40 30 20 10 0 2009* Median (IQR) 25.8 (16.7-37.1) 2010 24.3 (15.2-33.3) *Includes July to December 2009 2011 21.4 (13.3-30.7) 2012 17.0 (9.1-26.8) Year 2013 2014 14.3 (6.3-24.4) 12.6 (5.9-22.9) Limitations • Not all hospitals that perform PCI in the United States participate in the registry and we further excluded hospitals that did not participate in the registry throughout the entire study period. • Our analysis focused mostly on trends in potential overuse of PCI. Understanding whether the AUC have introduced new barriers to the performance of medically necessary procedures remains an important topic that could not be fully addressed in our study. • We cannot determine whether the observed changes fully reflect improvements in the quality of care and patient selection. • Specifically, we cannot exclude the possibility that the findings may derive, at least in part, from changes in documentation or even intentional up-coding, particularly of subjective data elements such as symptom severity. Conclusions This study of a large, national cohort of patients undergoing PCI from July 2009 to December 2014 demonstrates: 1. There has been a significant, 34% decline in non-acute PCI volume while the volume of acute PCIs remained stable. 2. Among patients undergoing non-acute PCI, there have been marked increases in reported angina severity, use of background anti-anginal medications, and high-risk findings on non-invasive testing. 3. Among non-acute PCIs, there has been a highly significant 51% reduction in the proportion classified as inappropriate and a 64% reduction in the absolute number of inappropriate PCIs. 4. Hospital-level variation in the proportion of inappropriate PCI persisted over the study interval. Implications • This is the first study to assess the national impact of a societal effort to quantify the appropriateness of a procedure on clinical practice. • Taken together, these findings suggest that there has been a marked change in patient selection for PCI and the practice of interventional cardiology since the introduction of the AUC. • There is a need for ongoing performance improvement initiatives and continued investigation of procedural appropriateness particularly as the AUC are further refined and revised. Backup Slides Patient-level Trends in Appropriateness of Non-acute PCI 100 Appropriate 90 Inappropriate Uncertain Year 2010 2011 2012 2013 2014 Non-acute PCIs, % 80 70 60 # of Inappropriate PCIs 21,781 16,429 11,779 9,299 7,921 64% reduction in absolute number, p<0.001 50 40 30 20 26.2% to 13.3%, 51% RR, p<0.001 10 0 2009* 2010 *Includes July to December 2009 2011 2012 Year 2013 2014