CNS Infection
advertisement

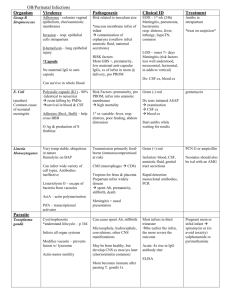
CNS Infection Meninges and Prions 1 CNS Infection - Meninges • CNS infections: most are due to sepsis • Pathogenesis: – – – – Hematogenous spread (most common) Traumatic implantation Local extension from nearby infection Ascent of peripheral nerve 2 Meningitis • • Inflammation of pia mater covering the brain Usually due to hematogenous spread; mechanism for bacterial meningitis: – – – Adherence of bacteria to mucosa of nasopharynx Bacteremia Translocation through blood-brain barrier (BBB) • – – • Involves bacterial lysins Bacteria in subarachnoid space attract neutrophils. Acute meningitis Risk factors in children – – – – Undernutrition; otitis media Pneumonia; immunodeficiency Viral infection; sickle cell disease Craniofacial abnormality 3 Viral Meningitis • Pathogenesis: – – • Most transmitted by fecal-oral route Respiratory route less common Clinical findings: – Fever, nuchal rigidity, headache 4 Complications of meningitis • • • • Seizures; focal neurologic deficits Cranial nerve palsies Sensorineural hearing loss Communicating and noncommunicating hydrocephalus 5 Laboratory findings in viral meningitis (CSF) • Increased CSF protein – • Increased total CSF leukocyte count – • Due to increased vessel permeability Initially neutrophils but converts to lymphocytes in 24 hours Normal CSF glucose 6 Laboratory findings in bacterial meningitis (CSF) • • • Increased CSF protein Increased total CSF leukocyte count Decreased CSF glucose – Usage of glucose for bacterial and fungal growth (bacterial & fungal meningitis) 7 Chronic Meningitis • – – Tuberculous meningitis • • • – • • headache, malaise, mental confusion, and vomiting moderate increase in cellularity of the CSF mononuclear cells, or a mixture of polymorphonuclear and mononuclear cells the protein level is elevated the glucose content typically is moderately reduced or normal may also lead to well-circumscribed intraparenchymal mass (tuberculoma) arachnoid fibrosis (hydrocephalus) 8 TB Meningitis - Pathology • • – – • • • • – – – The subarachnoid space contains a gelatinous or fibrinous exudate most often at the base of the brain obliterating the cisterns and encasing cranial nerves There may be discrete white granules scattered over the leptomeninges Arteries running through the subarachnoid space may show obliterative endarteritis inflammatory infiltrates in their walls marked intimal thickening The infection may spread through the CSF to the choroid plexuses and ependymal surface Florid cases show well-formed granulomas often with caseous necrosis and giant cells Similar findings are observed in tuberculomas within the brain 9 Chronic Meningitis • Meningovascular neurosyphilis – – Neurosyphilis is a tertiary stage of syphilis occurs in only about 10% of individuals with untreated infection – major manifestations is meningeal, called meningovascular neurosyphilis – As with other chronic infections, there can be parenchymal disease as well • Paretic neurosyphilis • Tabes dorsalis 10 Meningovascular neurosyphilis • • • involving the base of the brain and sometimes the cerebral convexities and the spinal leptomeninges associated obliterative endarteritis with distinctive perivascular inflammatory reaction rich in plasma cells and lymphocytes cerebral gummas (mass lesions rich in plasma cells) may also occur in relation to meninges and extend into the brain 11 Prion Diseases • This group of diseases includes – sporadic, familial, iatrogenic and variant forms of Creutzfeldt-Jakob disease (CJD) several animal diseases from this group are also known – • – including scrapie in sheep and goats and bovine spongiform encephalopathy in cattle ("mad cow" disease) all these disorders are associated with abnormal forms of a normal cellular protein, prion protein (PrPc) The abnormal form of this protein can act as an infectious agent – • • – it propagates itself injures the cells in which it is present Most cases of prion disease are either • • sporadic or associated with mutations in the gene that encodes PrPc 12 Pathogenesis of Prion Diseases • – – • • • • • – – – – Related to changes in the conformation of PrP from its native PrPc form to an abnormal configuration called either PrPsc (for scrapie) or PrPres (for protease resistant) in the abnormal conformation, the prion protein becomes resistant to protease digestion Once formed, PrPsc can then initiate comparable transformation of other PrPc molecules The infectious nature of PrPsc protein ability to propagate the pathologic conformational change The conformational change can occur spontaneously at an extremely low rate sporadic cases of prion disease If there is a mutation in the gene encoding PrPc, then the change can occur at a higher rate familial forms of prion disease Accumulation of PrPsc in neural tissue causes cell injury – how this material leads to the development of cytoplasmic vacuoles and eventual neuronal death is still unknown 13 Creutzfeldt-Jakob Disease • • • – – • • • – – CJD is a rare but well-characterized prion disease clinically as a rapidly progressive dementia It is sporadic in about 85% of cases (1 per million worlwide) familial forms also exist The disease has a peak incidence in the seventh decade There are well-established cases of iatrogenic transmission deep implantation electrodes contaminated preparations of human growth hormone Clinically, subtle changes in memory and behavior that rapidly progress to dementia The disease is uniformly fatal, with an average duration of only 7 months 14 Creutzfeldt-Jakob Disease • • The progression of the dementia in CJD is usually rapid – – – • • • • no or very little macroscopic evidence of brain atrophy On microscopic examination, the pathognomonic finding is a spongiform transformation of the cerebral cortex and deep gray matter (caudate, putamen) this consists of a multifocal process that results in the uneven formation of small, apparently empty, microscopic vacuoles of varying sizes within the neuropil and sometimes in the perikaryon of neurons In advanced cases, there is severe neuronal loss, reactive gliosis, and sometimes expansion of the vacuolated areas into cystlike spaces ("status spongiosus") No inflammatory infiltrate is present In all forms of prion disease, immunohistochemical staining demonstrates the presence of proteinase K-resistant PrPsc in tissue Western blotting of tissue extracts after partial protease digestion allows detection of diagnostic PrPsc 15 Variant Creutzfeldt-Jakob Disease • – – – • • • – – – They differed from typical CJD in several important respects: the disease affected young adults behavioral disorders figured prominently in the early stages of the disease neurologic syndrome progressed more slowly than in individuals with other forms of CJD The neuropathologic findings and molecular features of these new cases were similar to those of CJD a close relationship between the two illnesses Multiple lines of evidence indicate that this new disease is a consequence of exposure to the prion disease of cattle, bovine spongiform encephalopathy vCJD has a similar pathologic appearance with spongiform change and absence of inflammation there are abundant cortical amyloid plaques, surrounded by spongiform change 16 Variant Creutzfeldt-Jakob Disease • – – – • • • – – – They differed from typical CJD in several important respects: the disease affected young adults behavioral disorders figured prominently in the early stages of the disease neurologic syndrome progressed more slowly than in individuals with other forms of CJD The neuropathologic findings and molecular features of these new cases were similar to those of CJD a close relationship between the two illnesses Multiple lines of evidence indicate that this new disease is a consequence of exposure to the prion disease of cattle, bovine spongiform encephalopathy vCJD has a similar pathologic appearance with spongiform change and absence of inflammation there are abundant cortical amyloid plaques, surrounded by spongiform change 17