Burns - University of Maryland School of Medicine
advertisement

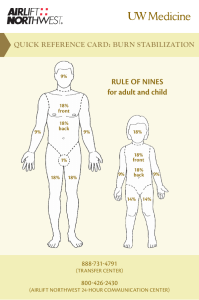
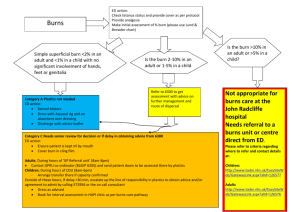
New Approaches in Burn Management Ken Butler D.O. Associate Professor Associate Residency Director Emergency Medicine Residency Program University of Maryland New Concepts in the Management of Thermal Injuries Objectives Smoke inhalation--who can be sent home? What really predicts intubation in smoke inhalation? RSI in smoke inhalation Whose palm is it anyway? Is the rule of nines really the rule? Challenging the Parkland formula New imaging for burn depth Blister management Hands Prehospital Care Pain Management by EMS EMS personnel hesitate to give an appropriate amount of pain medication to burn patients Airway Management EMS personnel are concerned about the airway NOT about making it to the regional burn center. so these patients show up in your ED Know the Burn Depth “Lingo” For the Consultants Emergency Physicians 1st Degree 2nd Degree 3rd Degree Know the Burn Depth “Lingo” For the Consultants Plastic Surgeons 3 Zones Partial Thickness Full Thickness Epidemiology as Easy as Two-Three 2/3 male 2/3 white 2/3 drunk 2/3 have flammable liquid 2/3 reduction in death due to smoke detectors 23 mean age Mechanisms Six groups based on mechanism of injury Scalds 30% Contact burns 30% Fire 30% Chemical 3% Electrical 5% Radiation 1% Flash Burns lighting BBQ – microsecond of exposure singed facial hairs – NO INHALATIONAL BURN Chemistry Flash Backs Tar Burns “Likes dissolve likes” Excellent removal with butter Wet Cement CaOH Treat like an ocular alkali burn Hydrofluoric Acid Burn Dissolve 10% calcium gluconate solution in 3 times the volume of a water-soluble lubricant. For burns to the fingers, retain gel in a latex glove. Chemistry Flash Backs Microwaves cause “superheating” Heating a liquid to a temperature above its normal boiling point, making it unstable. Microwave energy burns are based on the water content of tissue Muscle burns more than fat Delay between time of injury and signs of skin damage or pain Alexander RC, Surrel JA, Cohle SD. Microwave oven burns to children: An unusual manifestation of child abuse. Pediatrics. 1988;79(2):255-260. Just Admit Him for Syncope? Fireman has sudden collapse at a house fire His firefighter partner called it a “Knock Down Fire” This is classic presentation of CN CO requires longer exposure for symptoms Smoke Inhalation Who Can We Discharge Home? Arterial blood gases, chest radiography and carboxyhemoglobin estimation rarely influence immediate management. Bottom Line Patients presenting with normal vital signs and examination and short smoke exposure may be safe to discharge from the emergency department without further investigation. Mushtag,F, et al, Discharge from the accident and emergency department after smoke inhalation: influence of clinical factors and emergency investigations. J Emerg Med. 2004 Jun;11(3):141-4. Factors that Predict the Need for Intubation in Patients with Smoke Inhalation Injury No statistically significant correlation was found between intubation and any of the “classic symptoms” of smoke inhalation: stridor hoarseness drooling dysphagia (all p = 1.0) Madnani DD, et al, Factors that Predict the Need for Intubation in Patients with Smoke Inhalation Injury Ear Nose Throat J. 2006 Apr ;85(4):278-80 Factors that Predict the Need for Intubation in Patients with Smoke Inhalation Injury Intubation positively correlates with the physical examination findings of soot in the oral cavity (p < 0.001) facial burns (p = 0.025) body burns (p = 0.025) Madnani DD, et al, Factors that Predict the Need for Intubation in Patients with Smoke Inhalation Injury Ear Nose Throat J. 2006 Apr;85(4):278-80 Factors that Predict the Need for Intubation in Patients with Smoke Inhalation Injury Conclusion Patients with 1. soot in the oral cavity, 2. facial burns, or 3. body burns have a higher likelihood of laryngeal edema and the need for intubation. Madnani DD, et al, Ear Nose Throat J. 2006 Apr;85(4):278-80 Intubation and Smoke Inhalation “Take it early” as it never gets better ! Prevent a “DOA” Developing Obstructed Airway due to progressive edema First attempt is best attempt - This is for the most experienced intubator NOT a junior resident Three Factors of Smoke Inhalation That Produce a Difficult Airway Thermal damage – Upper airway takes the brunt and causes edema due to the poor conductivity of air and the high amount of dissipation that occurs in the upper airways. Air inhaled at 142°C - by the time it reaches the carina it will have cooled to 38°C. Asphyxiation – Tissue hypoxia alone - with CO or CN?? Pulmonary irritation – Particulate matter causes a decrease in all lung volumes and lung compliance CHEMICAL COMPONENTS OF SMOKE COMPOUNDS SOURCE Ammonia CLOTHING, FURNITURE, SULFUR DIOXIDE WOOL, SILK CHLORINE HYDROGEN CHLORIDE PLYVINYL CHLORIDE, PHOSGENE FURNITURE, (WALL, FLOOR COVERINGS) ACETALDEHYDE WALL PAPER FORMALDEHYDE LACQUERED WOOD ACROLEIN COTTON, ACRYLIC CYANIDE POLYURETHANE UPHOLSTERY CARBON MONOXIDE NYLON (ANY COMBUSTIBLE SUBSTANCE) EFFECT TIMING Mucous membrane irritation, bronchospasm, bronchorrhea Early onset (first several hours) Severe mucosal damage; ulcers, mucous plugging, mucosal slough, pulmonary edema Delayed often 1-2 days immediate Tissue hypoxia immediate RSI in Burn Patients Don’t take away what they already have Should be your thought before pushing any paralytic Why a 7.5 ETT ? What is your plan B ? The Difficult Airway in Smoke Inhalation You’re in. All you see is a “pink dead end” with charcoal. No landmarks. You reposition. Still a “pink dead end.” Now what? With your right hand, press down on the lower rib cage. LOOK FOR “tiny bubbles.” Now pass the tube or bougie. Hypotension Post Intubation in a Burn Patient Now the patient is intubated but your bagging is becoming an isometric exercise. And the patient is developing hypotension. Why? Is this burn shock? Is the vent setting wrong? What else might the patient need? Escharotomy “SNAP, CRACKLE, POP” The Palm and the Assessment of TBSA #1 Problem The area of the palm alone is 0.5 percent TBSA in males 0.4 percent TBSA in females Whereas the area of the palm plus the palmar surface of the five digits is 0.8 percent BSA in males 0.7 percent BSA in females Therefore, if a hand alone is used to assess the size of a burn, the percent BSA is overestimated. Rossiter ND et al. How big is a hand? Burns. 1996 May;22(3):230-1. Palmar Estimation and BMI #2 Problem The mean HSA diminishes significantly as BMI increases in both sexes (P<0.001). This difference is more pronounced in women, particularly those with a BMI >31 kg/m2 Awareness of the potential for overestimation of burn surface area using this method alone may improve the accuracy of burn area estimation. Berry MG et al. The influence of body mass index on burn surface area estimated from the area of the hand. Burns. 2001 Sep;27(6):591-4. The Rule of Nines Isn’t Always the Rule The Rule of Nines Isn’t Always the Rule The Rule of Nines provides reasonable estimates of body surface area for patients ranging from 10 to 80 kg. For obese patients weighing more than 80 kg, a rule of fives is proposed: 5% body surface area for each arm 5 x 4 or 20% for each leg 10 x 5 or 50% for the trunk and 2% for the head Livingston EH. Percentage of burned body surface area determination in obese and nonobese patients. J Surg Res. 2000 Jun 15;91(2):106-10 5% 50% 20% Livingston EH. Percentage of burned body surface area determination in obese and nonobese patients J Surg Res. 2000 Jun 15;91(2):106-10. Fluids and Formulas Lactated Ringer’s in all burn resuscitation Burn resuscitation requires more fluid than trauma resuscitation. Prevent hyperchloremic acidosis and buffer lactate Fluids and Formulas On the Horizon Adjuvant administration of high-dose ascorbic acid (66 mg/kg/hr) during the first 24 hours after thermal injury significantly reduces resuscitation fluid volume requirements by 30% wound edema severity of respiratory dysfunction Reduction of Resuscitation Fluid Volumes in Severely Burned Patients Using Ascorbic Acid Administration Arch Surg. 2000;135:326-331. Fluids and Formulas Formulas Parkland LR 4 mL/kg per percent burn ???? Modified Brook LR 2 mL/kg per percent burn Galveston LR 5000 ml/m² BSA burned/day plus 2000 ml/m² BSA total/day (also used in TEN) Barret J.P et al. Survival of paediatric burns involving 100% total body surface area Ann Burns Fire Disasters 1999; 12:139. Spies et al. Treatment of extensive toxic epidermal necrolysis in children Pediatrics 2001;108:11621168. How Well Does the Parkland Formula Estimate Actual Fluid Resuscitation Volumes? Despite its effectiveness, the Parkland formula underestimates the volume requirements in most adults with isolated cutaneous burns, especially in those with large full thickness burns. New data suggest 5.5-6.0 ml/kg per TBSA% Cartotto RC et. al. How well does the Parkland formula estimate actual fluid resuscitation volumes? Burn Care Rehabil. 2002 JulAug;23(4):258-65. Mitra B et.al. Fluid resuscitation in major burns J Surg. 2006 Jan-Feb;76(1-2):35-8. Inhalation and Fluid Requirements Patients with flame burns and inhalation injury have a mean fluid requirement of 2 ml/kg/% burn above patients with flame burns without inhalation injury for adequate resuscitation. Dai NT et al. The comparison of early fluid therapy in extensive flame burns between inhalation and noninhalation injuries. Burns 1998 Nov;24(7):671-5. Early Fluid Resuscitation Improves Outcomes in the Pediatric Patient The incidence of sepsis, renal failure, death due to cardiac arrest, and overall mortality is significantly higher in burned children receiving fluid resuscitation that was delayed >2 hr. Fluid resuscitation, given within 2 hr of a thermal injury, may be one of the most important steps in the prevention of multiorgan failure and mortality. Barrow RE et al. Early fluid resuscitation improves outcomes in severely burned children. Resuscitation. 2000 Jul;45(2):91-6. Emergency Department Fluid Resuscitation of Burn Patients Transferred to a Burn Center The average total body surface area (TBSA) estimated by the referring emergency department staff was 23.9% Compared with the burn intensive care unit staff ’s average estimation of 17.8% More importantly 47% were underresuscitated. Hagstrom M et al. A review of emergency department fluid resuscitation of burn patients transferred to a regional, verified burn center. Ann Plast Surg. 2003;51:173-6. Emergency Department Fluid Resuscitation of Burn Patients Transferred to a Burn Center Bottom Line Early communication permits review of estimated TBSA burn evaluation and permits cooperative calculations and optimal delivery of early fluid resuscitation. Burn center practitioners can improve care of patients before arrival by appropriately guiding the referring physician. Hagstrom M et al. A review of emergency department fluid resuscitation of burn patients transferred to a regional, verified burn center. Ann Plast Surg. 2003 Aug;51(2):173-6. Advances in Modalities Used for the Assessment of Burn Wound Depth Depth dictates prognosis Although bedside clinical evaluation remains the most widespread and cost-effective method, it is accurate only 2/3 of the time and is limited by poor interrater reliability New techonological modalities are now in use Laser Doppler Imaging (LDI) Burn Assessment by Laser Doppler Imaging Noncontact scanning technique that measures the entire burn wound surface. Color-coded perfusion map corresponds to varying burn depth. Accuracy up to 99% The latest, most accurate, most advanced modality of diagnosing burn depth Lara Devgan, BA, Modalities for the Assessment of Burn Wound Depth J Burns Wounds. February 2006; 5: e2. Management of Blisters in the Partial-Thickness Burn Previously a controversial topic Preservation: intact blister provides natural biological protection to the wound; blister fluid supports wound healing Blister debridement and fluid evacuation; components of blister fluid are detrimental to wound healing Management of Blisters in the Partial-Thickness Burn Blisters do not indicate burn depth Blisters typically signify the presence of a superficial partialthickness wound. We can get into trouble: they may occur over deeper dermal injuries that require excision and skin grafting. It is imperative to accurately identify the depth, as it correlates with the risk of wound infection. Visually Deceiving Burns Many burn injuries involve various depths of burn. Debridement of blisters aids in accurate wound depth identification by allowing direct visualization of the wound bed. Flame burn (direct contact) looks superficial with blisters. When gently cleansed, the wound is found to be a combination of deep second- and third-degree burn. Management of Blisters in the Partial-Thickness Burn Infection 3 Zones of Injury Coagulation Stasis central devitalized tissue marginally perfused Hyperemia outlying tissue Management of Blisters in the Partial-Thickness Burn Knowledge of these zones and the associated risk of conversion of partial-thickness to full-thickness injury requires ongoing assessment, especially during the first 48 hours. Prevention of wound conversion is key. Debridement of Burn Blisters Protective to the fragile zone of stasis in the early stages of injury Inflammatory mediators within blister fluid contribute to increasing size of the blister as the result of effect on microcirculation and increased capillary permeability Mechanical pressure from the blister on ischemic tissue contributes to deepening the wound Debridement of Burn Blisters Prevention of wound conversion reduces the risk of infection. Partial thickness wounds retain intact vascular supply and tissue viability are therefore less susceptible to microbial invasion CLINICAL PRACTICE GUIDELINES Bottom line of blister management Blisters should be debrided to stop burn wound conversion remove non-viable tissue allow proper visualization of the wound bed evacuate fluid that will increase the size of the blister evacuate fluid that suppresses local and systemic immune function Sargent RL. Management of blisters in the partial-thickness burn: an integrative research review. J Burn Care Res. 2006;27(1):66-81 Hand Burns Disability Edema hinders motion contraction compartment syndrome Elevation is crucial Evaluation of radial, ulnar, and palmar arch pulses by palpation/Doppler hourly “If they can’t make a fist, make it to a Burn Center.” Two Bedside Tests for the Detection of Developing Compartment Syndrome of a Digit Use a pulse oximeter to detect extremity hypoxia. <95% O2 saturation may require escharotomy Place an 18-gauge needle on the pressure tubing used to monitor arterial pressure and insert the needle into the compartment. Pressures >30 mmHg require escharotomy Hand Burn Contractures The typical contracture is an "intrinsic minus" position: the MP joints are fixed in hyperextension and the PIP joints are fixed in flexion. For this reason, positioning of the burned hand should place the MP joints at maximum flexion (90 degrees) to maximally stretch the collateral ligaments. Hand Burn Devices A vacuum-assisted closure device for treatment of hand burns is in prospective clinical trials. This device reduces edema and provides an excellent method of splinting. Synthetic Skin Substitutes Biobrane® is a bilayer synthetic skin substitute An outer epidermal analog is constructed of a thin silicone film that functions comparable to skin. Small pores in the silicone allow exudate removal and permeability to topical antibiotics. An inner dermal analog is composed of a three-dimensional irregular nylon filament weave to which type I collagen peptides are bonded. Synthetic Skin Substitutes Synthetic Skin Substitutes Outpatient Management of PartialThickness Burns: Biobrane versus 1% Silver Sulfadiazine Across multiple trials comparing rates of healing in partialthickness wounds, Biobrane® significantly reduced healing time without increased infection rates compared with topical SSD. When used on properly selected wounds, Biobrane therapy significantly decreases pain and total healing time without increasing the cost of outpatient burn care. Gerding RI et al. Outpatient management of partial thickness burns. Biobrane versus 1% silver sulfadiazine. Ann Emerg Med 1990:19:121-124. Sulfamylon Mafenide acetate diffuses through devascularized tissue. 80% is delivered to burned tissue over the first 4 hours following topical application. Sulfamylon® exerts bacteriostatic action against many gramnegative and gram-positive organisms, including Pseudomonas aeruginosa and certain strains of anaerobes. Silver Sulfadiazine SSD The use of SSD in partial-thickness wounds delays healing. Use of SSD requires dressing changes BID, which may cause trauma to the epidermal cellular bed. Despite its availability, its soothing effects and ease of application make its use widespread. Contraindicated Pregnancy Nursing mothers Allergy to sulfa Facial burns Aug. 8, 2005 Issue The Fallout: 'I Felt My Face Just Melting' Burn units struggle to cope with the flow of meth users straining their resources. Methamphetamine Burn Patients: What Makes Them Different? Key points A 2-year retrospective revealed that the methamphetamine burn patient requires two to three times the standard Parkland formula resuscitation. Methamphetamine burns larger than 40% TBSA have a 100% mortality. Warner P et al. The methamphetamine burn patient J Burn Care Rehabil. 2003;24:275-8. Burns in Pregnancy Clinical Challenges Intravascular volume is increased by 50% Fall in colloid pressure – increases extravasation Increase in TBSA Parkland formula is inaccurate INCREASE IN FLUID LOSS VS NONPREGNANT Third-trimester patients may require TWICE the Parkland formula for adequate resuscitation Pacheoco LD. et al. Burns in Pregnancy Obstet Gynecol. 2005 106:1210-2. Outcome and Changes in Survival Following Severe Burns (1985 to 2004) Outcome was evaluated in relation to the presence of three major risk factors for death: age 60 years or over total burned surface area 40% or more inhalation injury When zero, one, two, or three risk factors were present, mortality was respectively 0.5%, 9.9%, 48.0%, and 90.5%. Brusselaers N. et al. Outcome and changes over time in survival following severe burns from 1985 to 2004 Intensive Care Med. 2005;31(12):1648-53