13 Respiration - bloodhounds Incorporated
advertisement

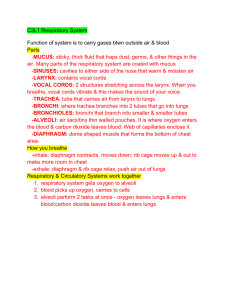
PHYSIOLOGY EXTERNAL AND INTERNAL RESPIRATION EXTERNAL RESPIRATION Respiration Movement of gases between the environment and the body’s cells – The exchange of air between the atmosphere and the lungs Known as ventilation or breathing Inspiration and Expiration – The exchanges of O2 and CO2 between the lungs and the blood – Transport of O2 and CO2 by the blood – The exchange of gases between blood and the cells RESPIRATION Anatomy of the Respiratory System Nasal Concha – Air eddies Air is cleaned Warmed Humidified Tonsils and Adenoids – Lymph nodes that filter the air – Located in the nose, back of the throat, below the tongue Larynx Contains Vocal Cords – Connective tissue bands that tighten to create sound when air moves past them Thyroid Cartilage – Sensitive to Testosterone levels Trachea Conducts Air – Lined with pseudostratified ciliated columnar epithelium – Cilia can be paralyzed by cigarette smoke Surrounded by C-shaped Cartilagenous rings and the trachealis muscle – Esophagus is dorsal to the trachea Approximately 4 inches long The nose serves all the following functions except A. As a passageway for air movement B. As the initiator of the cough reflex C. Warming and humidifying the air D. Cleansing the air Conducting System or Respiratory Tree Primary Bronchi – Surrounded by O-shaped cartilagenous rings – Bifurcates to Secondary Bronchi in the lungs – Respiratory Bronchioles Surrounded by smooth muscles Diameter of the airways becomes progressively smaller from the trachea to the bronchioles The total cross-sectional area increases with each division of the airways Pleural Membranes Visceral Pleura – Attached directly to the lungs Parietal Pleura – Attaches to the visceral pleura – Also attaches to the thoracic cavity Serous Fluid – Separates the two pleura and lubricates in order to decrease friction – Consistency of egg whites – Pleurisy occurs when the fluid decreases The Function of the Pleural Membranes is to hold the lungs open Alveoli Clustered at the ends of the terminal bronchioles Makes up the bulk of lung tissue Primary function is the exchange of gases between themselves and the blood Surrounded by elastic fibers – Creates Elastic Recoil Capillaries The alveoli are closely associated with an extensive network of capillaries – Blood vessels cover 80-90% of the alveolar surface forming a continuous “sheet” of blood in close contact with the air-filled alveoli Respiratory Membrane Consists of – The Wall of the Alveoli – The Respiratory Space This is a fluid filled space Pneumonia may cause the space to fill with more fluid than normal – This decreases the ability to exchange gases – The Wall of the Capillary Surfactant helps to prevent the alveoli from collapsing by A. Humidifying the air before it enters B. Warming the air before it enters C. Interfering with the cohesiveness of water molecules, thereby reducing the surface tension of alveolar fluid D. Protecting the surface of alveoli from dehydration and other environment variations The respiratory membrane is a combination of A. Respiratory bronchioles and alveolar ducts B. Alveolar walls, alveolar space and capillary walls C. Atria and alveolar sacs D. None of the above Gas Laws At sea level normal atmospheric pressure is 760mmHg – On top of Mt. Everest Patm = 153mmHg Dalton’s Law The total pressure exerted by a mixture of gases is the sum of the pressures exerted by the individual gases – 78% N2 – 21% O2 – 1% CO2 Partial Pressure of gases – The pressure of a single gas in a mixture Gas Law The total pressure of a mixture of gases, is the sum of the pressures of the individual gases (Dalton’s Law) Gases, singly or in a mixture, move from areas of higher pressure to areas of lower pressure If the volume of a container of gas changes, the pressure of the gas will change in an inverse manner (Boyle’s Law) Dalton’s Law To find the partial pressure of any one gas in a sample of air, multiply the atmospheric Pressure (Patm) by the gas’s relative contribution (%) to Patm. – Partial pressure of an atmospheric gas = Patm X % of gas in atmosphere – Partial pressure of oxygen = 760mmHg X 21% PO2 = 760 X 0.21 = 160mmHg Gases Move from High Pressure to Low Pressure Air flow occurs whenever there is a pressure gradient Boyle’s Law The pressure exerted by a gas or mixture of gases in a sealed container is created by the collisions of moving gas molecules with the walls of the container and with each other. – P1V1 = P2V2 An increase in volume will create a decrease in pressure and a decrease in volume will create an increase in pressure Boyle’s Law Changes in the volume of the chest cavity during ventilation cause pressure gradients that create air flow – When the chest volume increases, the alveolar pressure falls, and air flows into the respiratory system When the chest volume decreases, the alveolar pressure rises, and air flows out into the atmosphere Alveoli Composed of a single layer of epithelium called Type I cells Type II alveolar cells – Secretes surfactant – Surfactant decreases the surface tension of the water within the alveoli – Coats the inside of the alveoli – Cortisol causes the maturation of the type II cells in the fetal stage of development Dust Cells – Phagocytes Law of LaPlace The pressure inside a bubble formed by a fluid film is a function of two factors – Surface tension of the fluid (T) – Radius of the bubble (r) P = 2T/r Surfactant decreases the surface tension of water in the alveoli Newborn Respiratory Distress Syndrome (RDS) Air Flow Flow = changes in P / R – P = Pressure – R = Resistance to Flow Air flow in response to a pressure gradient The flow decreases as the resistance to flow increases Pressure in the System Alveolar Pressure – Pressure in the air spaces of the lungs Intrapleural Pressure – Pressure in the pleural fluid Intrapulmonary Pressure – Pressure within the lungs as a whole Atmospheric Pressure – Pressure in the atmosphere due to a column of air up to the stratosphere The pleurae are vital to the integrity of the lungs because they A. Contain cilia that protect the lungs B. control the volume of the lungs C. Secrete a lubricating serous fluid, allowing the lungs to glide over the thoracic wall during breathing D. Maintain the proper temperature of the lungs during sleep The factor(s) responsible for holding the lungs to the thoracic wall is/are A. The smooth muscles of the lung B. The diaphragm and the intercostals muscles C. The visceral pleurae and the changing volume of the lungs D. Surface tension from pleural fluid, positive pressure, and atmospheric pressure on the thorax Inspiration Time 0. – In the brief pause between breathes, alveolar pressure is equal to atmospheric pressure – When pressures are equal, there is no air flow Time 0-2 sec – Oxygen levels fall and Carbon Dioxide levels rise – Peripheral Chemoreceptors are stimulated Located in the carotid arteries Sensitive to oxygen levels – Central Chemoreceptors are stimulated Located in the Medulla Oblongata of the brain Sensitive ot carbon dioxide levels Inspiration Chemoreceptors stimulate the Medulla Oblongata The MO stimulates the Phrenic Nerve The Phrenic Nerve stimulates the respiratory muscles of the thoracic cage and the diaphragm The muscles contract and the thoracic volume increases Inspiration When thoracic volume increases then alveolar pressure fall approximately 4mmHg below atmospheric pressure Air flows from high pressure to low pressure until the pressures reach equilibrium Exhalation Time 2-4 sec: – As lung and thoracic volumes decrease air pressure in the lungs increases until the pressures equal equilibrium – Stretch receptors in the lung tissue are stimulated – Stretch receptors send information to the MO and this stops the phrenic nerve stimulation – Respiratory muscles relax Time 4 sec: – Elastic Recoil occurs – Alveolar pressure is now higher than atmospheric pressure due to a decrease in lung volume – Air leaves the lungs until pressures reach equilibrium Intrapleural Pressure Changes During Ventilation The lungs are “stuck” to the thoracic cage by the cohesive forces exerted by the fluid between the two pleural membranes If the thoracic cage moves, the lungs move with it Intrapleural Pressure The pressure between the pleural membranes is normally subatmospheric The combination of the outward pull of the thoracic cage and in inward recoil of the elastic lungs creates a subatmospheric intrapleural pressure of about -3mmHg What happens to subatmospheric intrapleural pressure if an opening is made between the sealed pleural cavity and the atmosphere? A knifing? Air in the pleural cavity breaks the fluid bond holding the lung to the chest wall The chest wall expands outward while the elastic lung collapses to an unstretched state – Like a deflated balloon – Pneumothorax Results in a collapsed lung that is unable to function normally – Correction of a Pneumothorax Removing as much air from the pleural cavity as possible with a suction pum Sealing the hole Emphysema Loss of elastic fibers for elastic recoil during expiration – Elastin is destroyed by elastase An enzyme released by immune cells Have more difficulty exhaling than inhaling Select the incorrect statement about external respiration A. Carbon dioxide is exchanged in the alveoli. B. Cells produce nitrogen by their metabolism. C. Diffusion accounts for the transport of gases. D. Oxygen is exchanged in the alveoli. E. The pulmonary capillaries are involved. The intra-alveolar pressure A. Is the pressure within the air sacs of the lung. B. Never equilibrates with atmospheric pressure. C. Is always less than intrapleural pressure. D. All of the above are correct. Ventilation Lung Volumes – Use a spirometer to measure pulmonary function Tidal Volume Inspiratory Reserve Volume Expiratory Reserve Volume Residual Volume Tidal Volume Breathing Quietly – The volume of air that moves during a single inspiration or expiration (VT). Average tidal volume during quiet breathing is about 350 – 500ml of air Inspiratory Reserve Volume (IRV) At the end of a quiet inspiration, take in as much additional air as you possibly can – About 3000ml in a 70kg male Expiratory Reserve Volume (ERV) Stop at the end of a normal exhalation, then exhale as much air as you possibly can This is a forceful exhalation – Average is about 1100ml Residual Volume (RV) Cannot be measured direction Even if you blow out as much air as you can, air still remains in the lungs and the airways – About 1200ml Lung Capacities The sum of two or more lung volumes – Vital capacity (VC) The sum of the inspiratory reserve volume, expiratory reserve volume and tidal volume This represents the maximum amount of air that can be voluntarily moved into or out of the respiratory system with one breath Total Lung Capacity Total Lung Capacity – Vital capacity + residual volume Functional Residual Capacity – Expiratory reserve volume + residual volume Airway Resistance Bronchioles are collapsible tubes Bronchoconstriction – Increases resistance to air flow and decreases the amount of fresh air that reaches the alveoli Histamine – Bronchoconstrictor Bronchodilators – Decreases resistance to air flow PARASYMPATHIC INPUT PNS is the primary neural control of bronchioles and causes bronchoconstriction Smooth muscle in the bronchioles have β-2 receptors that respond to epinephrine and norepinephrine – Stimulation of β-2 receptors relaxes airway smooth muscle and results in bronchodilation Used to treat asthma or allergies Chronic Obstructive Pulmonary Disease (COPD) Asthma, emphysema, chronic bronchitis INTERNAL RESPIRATION Pressure Gradients Arterial Pressures – PO2 = 100mmHg – PCO2 = 40mmHg Alveolar Pressures – PO2 = 100mmHg – PCO2 = 40mmHg Venous Pressures – PO2 = 40mmHg – PCO2 = 45mmHg Tissue Pressures – PO2 = 40mmHg – PCO2 = 45mmHg Hemoglobin Oxygen is transported two ways in the blood – Dissolved in the plasma – Bound to hemoglobin Mean Corpuscular Hemoglobin – Counting the RBC’s and quantifying the amount of hemoglobin per RBC Hemoglobin Concentration or % Hemoglobin One hemoglobin molecule binds up to four oxygen molecules – Percent oxygen saturation Globin – Proteins in the hemoglobin Alpha, beta, gamma and delta types Adults have 2 alpha and 2 bets Fetal Hb – Two gamma and two alpha Affects of Oxygen-Hemoglobin Binding Any factor that changes the conformation of the hemoglobin protein can affects its ability to bind oxygen Changes in plasma pH, PCO2, 2,3DPG and temperature alters oxygen-binding affinity of hemoglobin – 2,3DPG = 2,3 Diphosphoglycerate Carbon Dioxide Transportation 7% of the CO2 is carried by venous blood dissolved in the blood 93% diffuses into red blood cells, – 70% is converted to bicarbonate ions HCO3– 23% binds to hemoglobin as carbaminohemoglobin Hydrogen Ion Transportation Hemoglobin binds hydrogen ions – Prevents large shifts in the body’s pH – Too many hydrogen ions in the blood may cause respiratory acidosis This is caused by an increase in CO2 levels in the blood H2O + CO2 = H2CO3 = H+ + HCO3- Carbonic Anyhydrase Death from carbon monoxide poisoning would be due to A. The body’s destruction of hemoglobin B. The strong affinity of carbon monoxide to hemoglobin C. Formation of cellular toxins D. Inability of form hemoglobin The entire sequence of events involved in the exchange of O2 and CO2 between the body and the external environment is known as A. Internal respiration B. External respiration C. Ventilation D. Breathing E. All of the above are correct The majority of the carbon dioxide in the blood is found in which chemical form? A. Carboxyhemoglobin B. Bicarbonate C. Dissolved carbon dioxide gas D. Carbonic anhydrase Which of the following factors is (are) essential to hemoglobin saturation and the release of oxygen from the heme? A. Hydrogen concentration B. Partial pressure of carbon dioxide C. The amount of 2,3 DPG in the blood D. All of the above What happens to plasma pH during hyperventilation? How does this change in pH affect oxygen binding at the lungs when PO2 is decreased? How does it affect unloading of oxygen at the cells?