File
advertisement

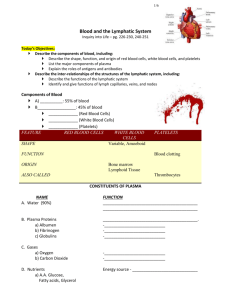
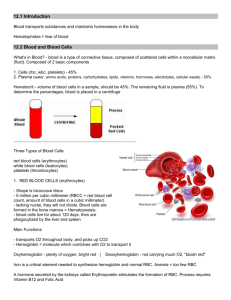
Cerebrum Midbrain Medulla Blood plasma Chapter 17: Blood Blood Formed elements fluid connective tissues plasma o non-living fluid matrix formed element-living blood “cells” suspended in the plasma o erythrocytes (red blood cells, or rbc’s) o leukocytes (white blood cells or wbc’s) o platelets Blood composition: Hematocrit plasma o 55 % of whole blood Buffy coat o Leukocytes and platelets o <1% of the whole blood Erythrocytes o 45% of whole blood o (hematocrit) o Different in both sexes Male: 47% Female: 42% Sticky, opaque fluid with metallic taste Color varies with O2 content o High O2 - scarlet o Low O2 – dark red pH 7.35- 7.45 ~8% of body weught Average volume o Male: 5-6 L o Female: 4-5 L Function of blood Distributing substances Regulating blood levels of substances o Deals with endocrine system Protection o White blood cells o Immune system o Antibody o Clotting factor White blood cells o Complete cells Red blood cells o Have no nuclei or other organelles Platelets are cell fragments Hemoglobin is a protein Polycythemia- body’s compensation of low oxygen Erythrocytes Biconcave discs, anucleate Diameter is larger than some capillaries Contains spectrin o plasma protein filled with >97% hemoglobin (Hb) doesn’t consume oxygen that they carry Hemoglobin structures Physical characteristics and volume 90% water Yellow in color Over 100 dissolved solutes o Nutrients, gasses hormones, wastes, proteins, inorganic ions Globin o composed of 4 polypeptide chains two alpha and two beta chains Heme o pigment bonded to each globin chains o has Fe (Iron) Each HB molecule can transport four 02 Hb can carry 20% CO2 but are dissolved in the plasma Hemoglobin (Hb) O2 loading in lungs o Produces oxyhemoglobin (ruby red) O2 unloading in tissues o Produces deoxyhemoglobin or reduced hemoglobin (dark red) CO2 loading in tissues o 20% of CO2 in blood binds to the Hb carbaminohemoglobin Hematopoiesis: blood cell formation Hematopoietic stem cells (hemocytoblasts) o o Hormones and growth factors push stem cells toward specific blood cell development Committed cells cannot change o Anemia This process can take up to 2 weeks Measure reticulocytes- to measure blood production Hormonal control of erythropoiesis Hormone Erythropoietin (EPO) Direct stimulus for erythropoiesis Always small amount in the blood to maintain basal rate Released by kidneys in response to hypoxia Signals the marrows to produce blood Decreases RBC numbers due to hemorrhage Insufficient hemoglobin per RBC (e.g., Iron deficiency) Reduces availability of O2 (e.g., high altitude) Blood has abnormally low O2 carrying capacity o Three groups Blood loss Low RBC production High RBC destruction Thalassemias o Typically Mediterranean ancestry o One globin chain absent or faulty Sickle- cell anemia o Black people of African malarial belt o One amino acid wrong in a globin beta chain o RBC’s crescent o Causes immunity to malaria Leukocytes Cause of hypoxia Globin metabolized into amino acids Make up <1% of total blood volume Function in defense against disease o Can leave capillaries via diapedesis o Move through positive chemotaxis Taxis- moving Chemo- chemical Positive- moving toward Leukocytes: Two Categories Granulocytes o Neutrophils, eosinophils, basophils Agranulocytes o Lymphocytes, monocytes Neutrophils Most numerous WBCs 3-6 lobes in nucleus; twice size of RBCs Very phagocytic— "bacteria slayers" Eosinophils Fate and destruction of Erythrocytes Bilobed nucleus Role in allergies, asthma and in modulating immune response Life span: 100-120 days Old RBC’s become fragile; Hb begins to degenerate Basophils Get trapped in the spleen Rarest WBCs Macrophages engulf dying RBC’s in spleen Contain histamine Heme and globin are separated in the spleen o acts as vasodilator to attract WBCs to o Iron salvage for reuse inflamed sites o Hehe degraded to yellow pigment bilirubin; liver secretes it in the bile into Are functionally similar to mast cells intestines Agranulocytes Lack visible cytoplasmic granules Have spherical or kidney-shaped nuclei Lymphocytes Second most numerous WBC Mostly in lymphoid tissue; few circulate in blood Two types o T lymphocytes (T-cells) Kills antibodies and virus o B lymphocytes (B-cells) Marks anti bodies Marks virus and antibodies Monocytes Largest leukocytes Leave circulation, enter tissues, and differentiate into macrophages Activate lymphocytes to mount an immune response Leukopoiesis Derive from megakaryoblast o Mitosis but no cytokinesis megakaryocyte Stem cell Developmental pathway Hemostasis -Stoppage of Bleeding Clotting factors and substances released by platelets and injured tissues Three steps 1. Vascular spasm 2. Platelet plug formation 3. Coagulation (blood clotting) Clotting Process Step 1 Vascular spasm Smooth muscle contracts, causing vasoconstriction. Step 2 Platelet plug formation Injury to lining of vessel exposes collagen fibers; platelets adhere. Platelets release chemicals that make nearby platelets sticky; platelet-plug forms. Production of WBCs o Stimulated by Interleukins Step 3 Coagulation Colony-stimulating factors (CSFs) All leukocytes originate from hemocytoblasts Fibrin forms a mesh that traps red blood cells and Lymphoid stem cells lymphocytes platelets, forming the clot. Myeloid stem cells all others o Granulocytes go from Myeloblastmature Coagulation cell Prothrombin activator Granulocytes stored in bone marrow o Prothrombin converted to thrombin o Thrombin converts fibrinogen fibrin Agranulocytes differ Monocytes o live several months o Share common precursor with neutrophils o Myeloid stem cells monocyte Lymphocytes o live few hours to decades o Lymphoid stem cell T lymphocyte and B lymphocyte precursors Platelets Cytoplasmic fragments of megakaryocytes Contain a platelet-derived growth factor (PDGF) Form temporary plug that seals blood vessels Circulating platelets kept inactive Age quickly; degenerate in about 10 days Clot Retraction Stabilizes clot Actin and myosin in platelets contract blood vessels’ smooth muscle tissue within 30–60 minutes Draws ruptured blood vessel edges together Vessel Repair Platelet-derived growth factor (PDGF) stimulates the rebuild of blood vessel wall Vascular endothelial growth factor (VEGF)stimulates endothelial cells to multiply and restore endothelial lining Thromboembolic Conditions Thrombus Type O o clot that develops and persists in unbroken o universal donor blood vessel o No A or B antigens o May block circulation leading to tissue Type AB death o universal recipient Embolus o No anti-A or anti-B antibodies o thrombus freely floating in bloodstream Blood being tested Serum Embolism o embolus obstructing a vessel o e.g., pulmonary and cerebral emboli Human Blood Groups blood cells has protein attached outside the RBC RBC membranes bear 30 types of glycoprotein antigens o Promoters of agglutination; called agglutinogens Mismatched transfused blood perceived as foreign Presence or absence of each antigen is used to classify blood groups : ABO and Rh ABO Blood Groups Types A, B, AB, and O Based on presence or absence of two agglutinogens (A and B) on surface of RBC’s Rh Blood Groups 52 named Rh agglutinogens (Rh factors) C, D, and E are most common Rh+ indicates presence of D antigen o 85% Americans Rh+ Anti-Rh+ antibodies not spontaneously formed in Rh– individuals o form if Rh– individual receives Rh+ blood, or Rh– mom carrying Rh+ fetus Second exposure Transfusions