EKG Self Study Guide
advertisement

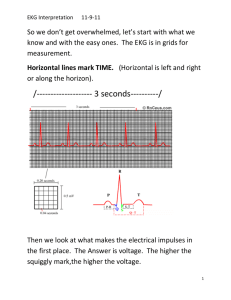
EKG Self Study Guide 1. View the slide show 2. Interpret the EKGs 3. Advance slides to review findings 4. Good luck! Companion to 12-lead EKG Interpretation Ben Lawner, NREMT-P NSUCOM Division of EMS Training Recall the approach 1. Take a deep breath 2. Analyze rate 3. Analyze rhythm 4. Look at axis 5. Look for injury/strain/ischemic patterns 6. Look for conduction defecits (RBBB, LBBB) 7. Hypertrophy, meds, toxic effects 8. Make your measurments (PR, QT/QTc, QRS) Sample EKG #1. Determine rate, rhythm, diagnosis, axis Interpretation EKG#1 Rate: approx 75/min Rhythm: Baseline sinus rhythm, P:QRS is 1:1 Axis: Physiologic Injury: ST elevation is present in the anterior, septal, and literal leads. Massive ST segment elevation is present in V2-V6, with moderate ST elevation that obscures visualization of the QRS complex in lead one. Changes are consistent with LCA occlusion. Other: R wave progression is difficult to determine secondary to the pathological ST-T changes. No evidence of chamber enlargement or hypertrophy. Sample EKG#2 Interpretation EKG#2 The EKG reveals an atrial flutter at a rate of approx 100 per minute. The QRS complexes are narrow and reveal a physiological axis. There is evidence of a premature ventricular complex, readily identifiable in the lateral chest leads. No evidence of ischemia or infarction. No evidence of R or L bundle branch block. Atrial flutter is conducted at approx 3:1. (3 flutter waves to one QRS). Sample EKG#3 Interpretation EKG#3 The EKG reveals an irregularly irregular rhythm suggestive of atrial fibrillation. The rate is variable, with a controlled or slow ventricular response. The axis is physiologic. ST-T changes suggestive of ischemia/injury are present in leads II, III, and aVF. ST elevation of >1mm in limb leads is indicative of a possible inferior wall myocardial infarction. Reciprocal changes are seen in leads one and aVL. Early R wave progression. EKG #4 Interpretation of EKG #4: This EKG reveals a baseline sinus rhythm. Rate cannot be determined definitively. The QRS is wide; V1 reveals an RSR’ pattern consistent with a right bundle branch block. The axis is physiologic but is not easy to determine because of ST elevation present in leads III and aVF (inferior wall). Other abnormal T changes are seen (T wave inversion) in leads V1-V4. ST segment depression is present in the lateral chest leads as well. No evidence of chamber enlargement. ST elevation in III and aVF with reciprocal depression in I and aVL may be consistent with an inferior wall MI (RCA lesion.) EKG #5 Interpretation of EKG#5: Baseline sinus rhythm. Rate appears normal (60-100) Axis is physiologic No evidence of block or conduction abnormality There is widespread ST segment elevation in all leads GLOBAL ST elevation is consistent with pericarditis EKG #6 EKG #6 Interpretation: EKG #6 reveals a baseline sinus rhythm. Rate approximately 80 bpm Axis is physiologic Complexes in V5 greater than 35 mm suggest LVH ST segment depression in leads V4-V6 in the setting of LVH is suggestive of a, “strain pattern”. No evidence of bundle brnach block ST segment depression in inferior chest leads EKG #7 EKG #7 Interpretation: Baseline sinus rhythm. Rate of approx 80/min Axis is physiologic No evidence of ventricular hypertrophy, but RAH is possible due to P wave in lead II >0.5 mm. Possible RBBB because of RSR’ in V1 and QRS >0.10 Note pathologic Q waves in II, III, aVF Pathologic Q waves are >0.04s or >1/3 the height of the R wave. Changes consistent with inferior wall myocardial infarction (old, possibly transmural). R wave progression preserved. EKG #8 Interpretation of EKG #8: Baseline sinus rhythm, rate approx 80. Right axis deviation, as evidenced by a primarily negative complex in lead I. Possible RAH due to large lead II P wave Possible RVH due to R>S in V1 Note pervasive strain pattern due to RVH evidenced in precordial leads. The presence of RAD plus the R>S in V1 is suggestive of RVH. Any drug toxicity? EKG#8 EKG Interpretation #8: Though the picture has poor resolution, it is clear that the lateral leads reveal a pattern of digoxin toxicity. Even though rate is impossible to determine, the “cored-out” and depressed ST segments in the lateral precordial leads suggest digoxin toxicity. Furthermore, the irregular R to R intervals hint at a baseline rhythm of atrial fibrillation. Many patients take digoxin for chronic atrial fibrillation. Moderate left axis deviation. EKG #9 EKG #9: This rhythm strip reveals a profound bradycardia. There is no relationship between the atria (P waves) and QRS complexes. This is consistent with complete A-V dissociation, or third degree heart block. This rhythm frequently requires emergent pacing. EKG #10 EKG #10 Interpretation: This EKG reveals a baseline sinus rhythm (p’s are difficult to discern.) The rhythm is a sinus tachycardia at approximately 100 per minute. Massive ST segment elevation is present in leads II, III, and aVF. Reciprocal changes (depression) in leads I and aVL. Note that the precordial chest leads (v4R to V6R) are placed on the right side of the chest. ST segment in a “right-sided” EKG likely indicates an inferior wall MI that involves the RIGHT ventricle. Be careful when giving these patients NTG. Administration of nitrates, due to the alteration of venous preload, can precipitate hypotension. Treat these MI’s with fluid first. The axis is physiologic, no evidence of chamber enlargement. R wave progression is not of value in this EKG because of the right sided chest leads. Final Rhythm Review Rhythm interpretation: -The first strip reveals a prolonged PR interval, with 1:1 conduction. This rhythm is a first degree A/V block. -The second strip is a 4:1 (or 3:1) atrial flutter. -The third rhythm strip reveals the typical atrial fibrillation. Note the fibrillatory baseline with irregular R to R intervals. The QT/QTc Interval: Calculation and Significance Measurement: Parameter: Abnormalities: QTc: Lengthening: From the beginning of the Q wave to the end of the T wave Normal QT intervals range from 0.360.41. Hypercalcemia will shorten the QT interval and yield measurements from 0.26-0.36s. The QT interval varies with heart rate. The corrected QT interval is calculated by adjusting your measurement for the patient’s heart rate. The QT divided by the square root of the R to R interval typically gives a QTc around 0.44 seconds. Diseases, drugs, and toxins can prolong the QT interval and precipitate attacks of lethal ventricular arrhythmias. Long QT syndrome, “Romano-Ward” Syndrome EKG: The QTc, adjusted for rate, would almost certainly be greater than 0.44 seconds. You can see in this example that the QTc is approximately 0.5-0.6 seconds (almost 3 large boxes!) Rate Cheat Sheet Besides calculating the number of R waves in a 3 or 6 second strip and multiplying by 20 or 10 seconds, simply divide the number of small (0.04s) units between consecutive R waves into 1500. -The heart rate can also be calculated from the R to R interval. Simply divide the number of large boxes (0.2s) between consecutive R waves into 300. -15 large boxes is a three second strip! -30 large boxes represents a six second strip! -For irregularly irregular rhythms, try to calculate rate with a decent time interval, preferably greater than a 3 second strip. Potassium summary: Digitalis effect summary: In addition to a wide variety of atrial conduction defects, ventricular ectopy, and heart blocks, early digitalis toxicity manifests itself as: a shortening of the QT interval in addition to scooped-out appearing ST segments. Precise axis calculation, anyone? Remember that it is simply a method of addition. I+III=II. The mean QRS vector will also point 90 degrees away from the most isoelectric lead. Leads with large amplitude R waves will shift the mean QRS vector in their general direction. Remember about dropping those stubborn perpendiculars? Chamber enlargement review: Name that hypertrophy? a) RVH b) LVH c) RAH d) LAH The EKG findings are consistent with: RVH Criteria for right ventricular hypertrophy include: -Tall R wave in lead V1 (R>S) -qR pattern in V1 -Right axis deviation -T wave inversion in right to mid precordial leads possible -Commonly due to ASD! -The pattern of T wave inversion is called, “strain”and is consistent with repolarization problems in hypertrophied muscle. Biphasic P waves, P waves with a terminal negative component or notched P waves are consistent with……..? Left Atrial Hypertrophy! What about the following EKG tracing? Right atrial enlargement: Factors suggesting right atrial enlargement include: -Tall, humped P waves -May be higher than 2.5 mm -Patient history may be significant for asthma, COPD, or pulmonary hypertension A zebra says, “Good-bye” What syndrome is typical of the following EKG features? -Short PR interval -Bouts of tachycardia -Upsloping R wave, “delta”wave -Often abberant conduction through ventricles (wide>0.10s QRS) -The name of this zebra is…. -Next slide for answer and EKG. Lead two reveals the short PR, delta wave, and the widerappearing QRS typical of Wolff-Parkinson-White syndrome.