Optimization Of CT Scan Protocol In Acute Abdomen
advertisement
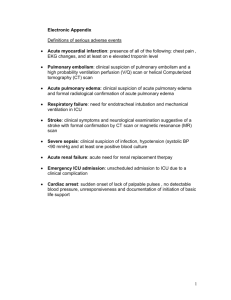
Optimization Of CT Scan Protocol In Acute Abdomen Dr Mohamed El Safwany, MD. Objectives • Learn definition & causes of acute abdomen. • Learn CT scan protocol for acute abdomen • Learn typical CT scan findings in common conditions of AA Acute Abdomen • • • • • Any clinical condition characterized by severe abdominal pain that develops over period of hours ,+l- abdominal tenderness or rigidity Acute Abdomen urgent therapeutic decision Acute Abdomen • Acute Abdomen • Often difficult to diagnose • Clinical presentation, physical examination can be very nonspecific • Laboratory exams: non‐diagnostic or not specific Acute Abdomen • Imaging is the cornerstone of evaluation Acute Abdomen • • • • • Diagnostic work up Acute Abdomen Abdominal plain film Ultrasound CT MRI Which is the best choice? Acute Abdomen Diagnostic work up Acute Abdomen Which is the first line imaging modality used for the upper right quadrant and pelvic pain? 1) CT 2) US 3) MRI 4) Abdominal plain film • • • • Diagnostic work up Acute Abdomen US CT Causes of Acute Abdomen • • • • • • • • • 28% Acute appendicitis 10% Acute cholecystitis 4% Bowel obstruction 4% Gynecologic diseases 3% Acute pancreatitis 3% Renal colic 2% Perforated duodenal ulcer 2% Acute diverticulitis 33% Unknown cause Optimization Of CT Scan Protocol In Acute Abdomen Scan Protocols • core of every CT examination. • protocols should be appropriate for the clinical indication • should include all aspects of the exam such • positioning, • nursing instructions, • scan parameters( including radiation dose) • reconstruction/reformatting instructions, How do you design a CT protocol components •Scanning parameters •contrast when , how •Dose information •filming •network instruction Scanning parameters CT machine • kVp • mAs • Slice collimation • Slice thickness • Interscan spacing • Reconstruction algorithm for different tissues Scanning parameters • multislice CT is better than single slice MSCT : • High quality • Wider range of examination • Thinner slices • Shorter scan time • Multiphases protocol • Better reconstruction kVp • • • • Between 80-140 Higher kVp: in routine CT abdomen Lower KVp: CTA, perfusion studies Manual versus automatic KVp selection Care kV, Siemens machine Tube current • mAs selected should result in diagnostic quality images • Most body CT and even head CT: Use AEC Tube current • For all patients less than 20 years old, set the minimum mA to 80 for all studies Collimation •Narrow collimation and small reconstruction intervals can help detect calculi in the biliary system and genitourinary tract. • Slice thickness: Acquire thins, reconstruct thick: Less noise • Scan coverage: scan length • Rotation speed: Keep fastest…for most regions to allow breath hold tech and more coverage Increment • is the distance between the reconstructed images in the Z direction. • When the chosen increment is smaller than the slice thickness, the images are created with an overlap. Increment • is useful to reduce partial volume effect, giving you better detail of the anatomy and high quality 2D and 3D post-processing . • can be freely adapted from 0.1 - 10 mm. CT Image suitable for diagnostic purpose : • • • • Low noise High contrast resolution Sharpness of image Absence of artifacts Pediatric protocols • should be adjusted regarding exposure parameters • Protocol optimization reducing radiation dose: • mAs according to patient size and weight • Implementation of automatic control system contrast • • • • Oral I.V Rectal Urinary bladder .....etc Oral Contrast • Type of contrast • Volume of contrast • Timing of contrast oral contrast Types • Water neutral: negative contrast used in most cases • Water soluble positive contrast • Ominipaque 350 • Gastrografin agent (2% – 4%) oral contrast Volume • Upper abdomen: • Minimum 700-1000 ml of contrast • divided into 3 cups (approximately 250 – 300 ml) • 1st cup,30 minutes before exam • 2nd cup,15 minutes before exam • 3rd cup , 5 minutes before exam oral contrast Volume Abdomen-Pelvis: • Minimum 1000 ml • divided into 4 cups • 1st cup ,1 hour before exam • 2nd – 4th cups every 15 minutes • Start exam 5 minutes after the 4th cup oral contrast • • • • • • • • • • •Use in –Suspected appendicitis –Fistula –Leakage of contrast anatomosis gastric bypass –Perforation •Not used in –High intestinal obstruction –Ureteric colic –Intestinal bleeding –Vascular cuases Rectal contrast may be used in • appendicitis • diverticulitis • leak or perforation • colonography • penetrating injury IV Contrast • opacifies abdominal vasculature and • provides useful information regarding enhancement of the parenchymal organs and intestine • 100-120 mL of iodinated contrast material injected • rate of 3-5 mL per second is adequate IV Contrast • is recommended in most cases. • Exceptions: • include evaluation of suspected ureteral colic, retroperitoneal hge • contraindication to contrast IV contrast • Normal creatinine level , should be within a month • High creatinine level , to be discuss with ordering physician • Look for • renal disease , hypertension, diabetes ,malignancy Premedication Allergy pateints • Oral: 50 mg of prednisone 13 h., 7 h. and 1 h. prior to procedure and • IV: 200mg hydrocortisone 6h and 2h prior to procedure and 50 mg p o of Benadryl 1h prior to procedure Technical aspect of acute abdomen CT Imaging • • • • IV contrast should be given at 3-5 ml/sec total of 100-120 mL, followed by saline Use SMART PREP or threshold tech IV access • • • • • CTA's : high rates of injection, a large bore IV, 18 g or larger is required Do not use hand/forearm veins Antecubital only. IV access CTA's : • During power injections, the site must be closely monitored during the first 15 to 20 seconds to prevent extravasation • Some catheters are designed for use with power injectors, • Check the label of any catheter for maximum flow rate and pressure. • Adjust the settings on the power injector accordingly. Contrast extravasation • most are small & self limited. • Ice pack and elevate for 20 mins. • If swelling/pain resolved patient can be discharged • Advise patient to contact MD if swelling worsen • Skin sloughing is rare, can require a referral to plastic surgeon Contrast extravasation Compartment syndrome : • with large volumes in the forearm/hand. • pain with extension of fingers. • May lose pulses • become cold/discolored. • requires referral to plastic/orthopedic/hand surgeon. Renal Function/Creatinine levels • Patients with pre-existing renal failure or Diabetes Mellitus should have creatinine levels checked when the exam is nonemergent • In general, a creatinine of 1.8 or less is acceptable for non-ionic contrast use Renal Function/Creatinine levels • For Creatinine levels above 1.8 there are several options: • 1. Withhold contrast if indication for contrast use is equivocal • 2. Use a reduced dosage. • 3. If the patient is on dialysis with no renal function, they can be given contrast, preferably prior to dialysis. • 4. If the patient is on dialysis with borderline function, the nephrologist should be consulted prior to contrast use. Contrast Allergy • Patients with prior severe/life threatening reactions should avoid contrast if at all possible • For other prior reactions, pre-medicate with • oral prednisone 50mg 13 hrs,7 hrs & 1 hr prior to injection and oral benadryl 50 mg 1 hr prior General Hints • Topogram : AP, 512 or 768 mm. • Patient positioning: Patient lying in supine position, arms positioned comfortably above the head in the head-arm rest lower legs supported. • Patient respiratory instructions: inspiration • Scout : AP and lateral General Hints • Limit scan to intended anatomic area to cut dose by 10% Abdomen: • Just above diaphragm – Inferior pubic symphysis Chest: • Routine: Apex to adrenals • PE or benign clinical reasons: Apex to lung bases Common causes of acute abdomen Practical aspect Appendicitis • most common causes of acute abdominal pain • Most :1000 cc oral contrast before about 1 hour before • Others give oral & rectal • Scanning after 70 second from IV injection , might need delayed scan Acute Pyelonephritis • Fever, chills, and flank tenderness. • referred for CT when symptoms are poorly localized or suspected complications . • nephrographic phase (70–90 seconds after injection) or • excretory phase (5 minutes after injection). Ureteral Stones • continuous breath-hold acquisition from kidneys to bladder base. • Narrow (3-mm) collimation and small reconstruction intervals (also 3 mm) are essential for optimal detection of small calculi • Prone scans may be needed to differentiate a ureterovesical junction stone from a recently passed stone Acute Pancreatitis Contrast: • Patient should drink water as the oral contrast, OPACIFICATION AND DISTENTION OF DUODENUM IS VERY HELPFUL • IV contrast at 4-5mL/sec for 120 mL Acute Pancreatitis • narrow collimation , thin reconstructions, apply radiation protection facilities in the machine • scan entire pancreas in single breath hold for all phases. Acute Pancreatitis • Acute Pancreatitis • Noncontrast – Liver dome to iliac crests • Arterial phase – Initiate scan at 25 sec. Use “SMART PREP” Aorta (150HU) to monitor those with poor cardiac output. Top to bottom of liver. Ideally obtain excellent pancreatic parenchymal arterial opacification with minimal contrast in portal vein. Acute Pancreatitis • Portal venous phase – 80 sec delay. Scan the entire abdomen in this acquisition (top of the liver to sp). • Delayed 3 minute scan through liver and kidneys. • Coronal and sagittal reformat of portal venous phase Diverticulitis rectal contrast: • is highly accurate for diagnosis • Most use 400–800 mL of 3% iodinated contrast • IV contrast : • helpful in detection & characterization of pericolonic inflammation • recommended in most patients. Small Bowel Obstruction • • • • common cause of acute abdomen adhesions most common (64%–79%) hernia (15%–25%), tumor (10%–15%) Small Bowel Obstruction • high-grade small bowel obstruction : • best performed without oral contrast. • large amounts of fluid in bowel acts as a natural contrast agent, • when combined with IV contrast ,allows opacification of bowel wall & masses Small Bowel Obstruction low-grade obstruction: • oral contrast • improves accuracy in detection of inflammation & abscesses • optimize identification of a transition zone Ischemic Bowel • present with symptoms ranging from relatively minor discomfort to acute abdominal pain, which makes clinical diagnosis difficult • vascular occlusion or thrombosis, whether from arterial or venous disease, and hypoperfusion Ischemic Bowel • rapid (4-5 mL/sec) IV contrast for optimal vascular opacificationi • IV contrast is essential for depiction of the thickened, edematous bowel wall, which can easily be appreciated against the obstructed, fluid-filled intestine • Arterial & venous phases are essential • Water can be used as alternative for bowel lumen Gastrointestinal Perforation • If possible, oral & IV contrast should be used • to help localize perforation & characterize complications • Such as peritonitis and abscess formation. Vascular System • Aortic Aneurysm Rupture • Aortic Dissection • Hemorrhage • rapid (4-5 mL/sec) IV bolus contrast for optimal vascular opacification • Narrow collimation • high-quality 3D images • Oral contrast material is not administered , can interfere with reconstruction AORTIC ANEURYSM • Study should only be performed in hemodynamically stable patients. • Hemodynamically unstable patients with high degree of suspicion of aortic pathology should go directly to OR. • If becomes unstable in CT, a quick non conreast scan may be diagnostic. AORTIC DISSECTION Contrast: • No oral contrast • IV contrast at 4-5mL/sec with 125 mL AORTIC DISSECTION Scan method: • narrow collimation , thin reconstructions, apply radiation protection facilities in the machine. • Non contrast – show intramural hematoma not well seen with contrast. • Top of arch to iliac crests AORTIC DISSECTION • Arterial: Use HiRes HD mode, SMART PREP over aortic arch with threshold 150 HU, Apices to SP • Portal Venous – 80 sec delay from dome of liver to SP to assess organ perfusion. • Coronal and sagittal reformat of arterial phase • Coronal and sagittal MIP of arterial phase LOWER EXTREMITY RUN-OFF • Contrast: • IV contrast at 4-5mL/sec for 125 mL (consider increasing to 150 for very tall patients) LOWER EXTREMITY RUN-OFF Scanning method • narrow collimation , thin reconstructions, apply radiation protection facilities in the machine • Non contrast: From diaphragmatic hiatus through toes • Arterial: LOWER EXTREMITY RUN-OFF • SMART PREP– trigger scan at first blush of contrast. Do not use ROI! • From diaphragmatic hiatus through toes • Coronal and sagittal reformat of arterial phase • Coronal MIP of arterial phase Sharing protocol files • Having hard copy protocol books by body region in all scanner suites • Scan length • Scan phases or passes • Contrast injection details • Shared drive access to protocols with in the intranet from any internal personal computer • Electronic copies of protocols with version date and protocol types Text Book • David Sutton’s Radiology • Clark’s Radiographic positioning and techniques Assignment • Two students will be selected for assignment. Question • Define Technical aspect of acute abdomen CT Imaging? • Thank You