2.Interstitial Disease Processes PP
advertisement

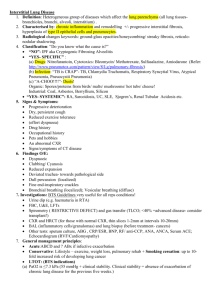
Dr.J.A.Venter
Dept. Imaging Sciences
UFS
2/10/2012
A structured approach to interpretation of HRCT involves the following
questions:
• What is the dominant HR-pattern:
• reticular
• nodular
• high attenuation (ground-glass, consolidation)
• low attenuation (emphysema, cystic)
•
Where is it located within the secondary lobule (centrilobular, perilymphatic
or random)
•
Is there an upper versus lower zone or a central versus peripheral
predominance
•
Are there additional findings (pleural fluid, lymphadenopathy, traction
bronchiectasis).
Correct diagnosis of IIPs can be achieved only by means of interdisciplinary
consensus and stringent correlation of clinical, imaging, and pathologic
findings.
HRCT Basic Interpretation
Dominant pattern
Reticular vs Nodular
High density vs Low density
Distribution in Secondary
Pulmonary Lobule
Centrilobular, Perilymphatic,
Random
Distribution within lung
Upper zones , Lower zones
Central or Peripheral
Chest radiographs : collection of innumerable small
linear opacities that, by summation, produce an
appearance resembling a net .
This finding usually represents interstitial lung
disease.
The constituents of a reticular pattern are more clearly
seen at thin section CT, whether they are interlobular
septal thickening, intralobular lines, or the cyst walls
of honeycombing.
Chest radiograph shows reticular pattern.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Interlobular septum
10–20-mm long forming the
borders of lobules;
perpendicular to the pleura in
the periphery. Composed of
connective tissue and contain
lymphatic vessels and
pulmonary venules.
Thin linear opacities between
lobules Not usually seen in
the healthy lung (normal
septa are approximately 0.1
mm thick) but are clearly
visible when thickened (eg,
by pulmonary edema).
Intralobular lines
visible as fine linear opacities
in a lobule when the
intralobular interstitial tissue
is abnormally thickened .
When numerous, they may
appear as a fine reticular
pattern. Intralobular lines
may be seen in various
conditions, including
interstitial fibrosis and
alveolar proteinosis .
Transverse CT scan shows interlobular septum (arrow) in a healthy individual.
©2008 by Radiological Society of North America
Hansell D M et al. Radiology 2008;246:697-722
Transverse CT scan shows lntralobular lines.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Reticular Pattern
Septal Thickening
Thickened Interlobular Septae
Smooth
Nodular/Irregular
Interstitial pulmonary
edema
Lymphangitic spread
of carcinoma or
lymphoma
Alveolar proteinosis.
Sarcoidosis
Lymphangitic spread of
carcinoma or
lymphoma
Silicosis
Fibrosis
Honeycombing
UIP
Chest radiographs : innumerable small rounded
opacities that are discrete and range in diameter from
2 to 10 mm .
The distribution is widespread but not necessarily
uniform.
CT :classified as one of three anatomic distributions:
centrilobular, perilymphatic, or random.
Magnified chest radiograph shows a nodular pattern.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Multiple Small Nodules: Differential Algorithm
Nodules along the pleura and fissures ?
NO
YES
Centrilobular Nodules
Patchy : + axial
interstitium
(>90% fissures
or
bronchovascula
r)
Diffuse and
Uniform:
Normal axial
interstitium(no
predominance)
Perilymphatic
Distribution
Random
Distribution
Sarcoid
Silicosis/CWP
Lymphangitic Ca
Metastasis
Lymphangitic Ca
Miliary Infection
Tree-in-bud
Tree-in-bud
absent
Bronchiolar
disease
Bronchiolar/
Vascular
Disease
Infectious
Bronchiolitis
Bronchopneumo
nia,TB
Smoker: RB-ILD
Non-smoker:
Subacute HP
BAC,COP,Oedema,
LCH,Vasculitis
Tree in bud
Infection
Tuberculosis
MAC (mycobacterium avium)
Bacterial, Fungal
Airway disease
Cystic Fibrosis or Bronchiectasis
ABPA
Allergic Bronchopulmonary Aspergilosis
(rare)
Ground Glass Opacity
Acute
Chronic
Pulmonary edema
-Heart Failure
- ARDS
Hypersensitivity pneumonia
Pulmonary hemorrhage
Chronic Eosinophilic
Pneumonia
Pneumonia
- Viral
- Mycplasma
- PCP
Acute Eosinophilic
Pneumonia
Organizing pneumonia (COP)
Alveolar Proteinosis
Lung Fibrosis
-UIP
-NSIP
Broncho-Alveolar Carcinoma
Chest radiographs : area of hazy increased lung opacity,
usually extensive, within which margins of pulmonary
vessels may be indistinct.
CT : hazy increased opacity of lung, with preservation of
bronchial and vascular margins . It is caused by partial
filling of airspaces, interstitial thickening (due to fluid,
cells, and/or fibrosis),partial collapse of alveoli, increased
capillary blood volume, or a combination of these, the
common factor being the partial displacement of air .
Ground-glass opacity is less opaque than consolidation, in
which bronchovascular margins are obscured.
Transverse CT scan shows ground-glass opacity.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Nonspecific
Highly significant
60-80% : active and potentially
treatable lung disease.
20-40% : fibrosis(associated HRCT
findings of fibrosis, such as
traction bronchiectasis and
honeycombing ).
Patchwork of regions of differing attenuation that may
represent (a) patchy interstitial disease, (b) obliterative
small airways disease or (c) occlusive vascular disease .
Air trapping secondary to bronchial or bronchiolar
obstruction may produce focal zones of decreased
attenuation, an appearance that can be enhanced by
using expiratory CT .
The mosaic attenuation pattern can also be produced
by interstitial lung disease characterized by groundglass opacity; in this situation, areas of higher
attenuation represent the interstitial process and areas
of lower attenuation represent the normal lung.
Density differences between affected and non-affected
lung areas - patchy areas of black and white lung.
The role of the radiologist is to determine which part is
abnormal: the black or the white lung
• Look at expiratory scans for air trapping
• Look at the vessels
Transverse CT scan shows mosaic attenuation pattern caused by obliterative small-airways
disease.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Permanently enlarged airspaces distal to the terminal bronchiole with destruction of
alveolar walls.
Areas of low attenuation without visible walls as a result of parenchymal destruction.
Centrilobular emphysema
Panlobular emphysema
Most common type
Irreversible destruction of alveolar walls in the centrilobular portion of the lobule
Upper lobe predominance and uneven distribution
Strongly associated with smoking.
Affects the whole secondary lobule
Lower lobe predominance
In alpha-1-antitrypsin deficiency, but also seen in smokers with advanced emphysema
Paraseptal emphysema
Adjacent to the pleura and interlobar fissures
Can be isolated phenomenon in young adults, or in older patients with centrilobular
emphysema
In young adults often associated with spontaneous pneumothorax
Lung cysts are defined as radiolucent areas with a wall
thickness of less than 2mm.
Cavities are defined as radiolucent areas with a wall
thickness of more than 2mm and are seen in infection
(TB, Staph, fungal, hydatid), septic emboli, squamous
cell carcinoma and Wegener's disease.
Pathology.—A cyst is any round circumscribed space that is
surrounded by an epithelial or fibrous wall of variable thickness .
Radiographs/CT:Round parenchymal lucency or lowattenuating area with a well-defined interface with normal lung.
Variable wall thickness but are usually thin-walled (2 mm) and
occur without associated pulmonary emphysema .
Usually contain air but occasionally contain fluid or solid
material.
Enlarged thinwalled airspaces in patients with
lymphangioleiomyomatosis or Langerhans cell histiocytosis
Thickerwalled honeycomb cysts are seen in patients with endstage fibrosis .
Coronal CT scan shows a cyst.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
LAM
LCH
LIP
PCP
Honeycombing
Irreversible localized or diffuse bronchial dilatation,usually
resulting from chronic infection, proximal airway
obstruction, or congenital bronchial abnormality .
Radiographs and CT :Signet ring sign, lack of tapering of
bronchi, and identification of bronchi within 1 cm of the
pleural surface.
Cylindric, varicose, or cystic, depending on the appearance
of the affected bronchi.
Often accompanied by bronchial wall thickening, mucoid
impaction, and small-airways abnormalities .
May mimic cystic lung disease and bullous emphysema.
Bronchiectasis caused by primary airway disease should be
differentiated from tracion bronchiectasis as a result of
fibrosis.
Transverse CT scan shows varicose bronchiectasis.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Small cystic spaces with irregularly thickened walls
composed of fibrous tissue.
Peripheral and subpleural lung regions regardless of the
cause.
Subpleural several contiguous layers.
Distinguished from paraseptal emphysema in which
subpleural cysts usually occur in a single layer.
Pathology.—Honeycombing represents destroyed and fibrotic lung
tissue containing numerous cystic airspaces with thick fibrous walls,
representing the late stage of various lung diseases, with complete loss
of acinar architecture. The cysts range in size from a few millimeters to
several centimeters in diameter, have variable wall thickness, and are
lined by metaplastic bronchiolar epithelium .
Chest radiographs : closely approximated ring shadows, typically 3–10
mm in diameter with walls 1–3 mm in thickness, that resemble a
honeycomb; the finding implies end-stage lung disease.
CT : the appearance is of clustered cystic air spaces, typically of
comparable diameters on the order of 3–10 mm but occasionally as
large as 2.5 cm . Honeycombing is usually subpleural and is
characterized by well-defined walls . It is a CT feature of established
pulmonary fibrosis .Because honeycombing is often considered specific
for pulmonary fibrosis and is an important criterion in the diagnosis of
usual interstitial pneumonia , the term should be used with care, as it
may directly impact patient care.
Transverse CT scan shows honeycombing.
Hansell D M et al. Radiology 2008;246:697-722
©2008 by Radiological Society of North America
Upper vs Lower zone
Upper zone
Sarcoid
Silicosis
Coalworkers Pneumoconiose
Centrilobular Emphysema
Langerhans Cell Histiocytosis
Chron. Hypersens.
Pneumonitis
Lower Zone
Edema
Panlobular Emphysema
UIP in:
• IPF
* Collagen-vascular
disease
* Asbestosis
Central vs. Peripheral zone
Central zone
Sarcoid
Bronchitis
Pulmonary Edema
Peripheral Zone
COP/OP
Chronic Eosinophilic Pneumonia
Hematogenous Metastases
UIP in:
* IPF
* Collagen - Vascular Disease
* Asbestosis
Pleural effusion is seen in:
1. Pulmonary edema
2. Lymphangitic spread of carcinoma - often unilateral
3. Tuberculosis
4. Lymphangiomyomatosis (LAM)
5. Asbestosis
In sarcoidosis the common pattern is right paratracheal
and bilateral hilar adenopathy ('1-2-3-sign').
In lung carcinoma and lymphangitic carcinomatosis
adenopathy is usually unilateral.
'Eggshell calcification' in lymph nodes commonly occurs
in patients with silicosis and coal-worker's
pneumoconiosis and is sometimes seen in sarcoidosis,
postirradiation Hodgkin disease, blastomycosis and
scleroderma .
Know anatomy of secondary pulmonary lobule
Identify Pattern:
Reticular,Nodular, High Attenuation, Low Attenuation
Distribution
Additional Findings
1.http://www.radiologyassistant.nl/en/42d94cd0c326b
Accessed 2/3/2012
HRCT part I &2
Robin Smithuis, Otto van Delden and Cornelia SchaeferProkop Radiology Department of the Rijnland Hospital,
Leiderdorp and the Academical Medical Centre,
Amsterdam, the Netherlands
2.Diffuse Nodular Lung Disease – A Differential
Alogrith:Naidich - MDCT Congress , Sandton,RSA.
16/08/2011
3. March 2008 Radiology, 246, 697-722. Fleischner
Society: Glossary of Terms for Thoracic Imaging