Expected Value of Perfect Information: Active Learning
advertisement

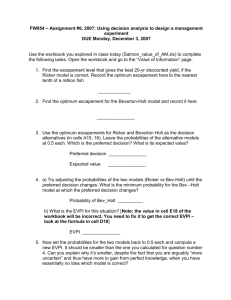
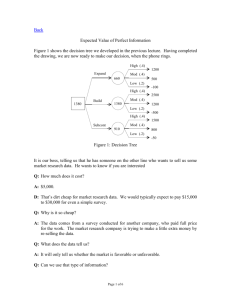
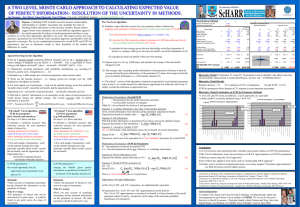
Expected Value of Perfect Information: Active Learning Through User-Friendly Computations, Displays, and Application Discussions R Brett McQueen, PhD1 D. Eldon Spackman, PhD2 Jonathan D. Campbell, PhD1 1. University of Colorado, Aurora, CO 2. University of York, Heslington, York, UK Workshop Objectives • Review theory and concepts of value of information • Expected Value of Perfect Information (EVPI) active learning – Gain understanding through a workshop exercise – Display EVPI case • Discuss EVPI applications Welfare Economics & Bayesian Decision Theory Decision Analytic Model Uncertainty in Net Benefit Mean Net benefit Expected Value of Perfect Information Q1: Adopt Intervention with Present Information? Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. Journal of Health Economics 18 (1999): 341-364. Q2: Generate Future Evidence? Decision Analytic Model (e.g., Population, intervention, comparator(s), outcome(s), time that best represent disease state) Maximize Social Welfare Function (normative weights included) Mean Net benefit Mean Net Benefit = QALYs*Willingness to pay - Costs Positive analysis Q1: Adopt Intervention with Present Information? Answer = maximum mean net benefit Welfare Economics & Bayesian Decision Theory Decision Analytic Model Uncertainty in Net Benefit Mean Net benefit Expected Value of Perfect Information Q1: Adopt Intervention with Present Information? Q2: Generate Future Evidence? Decision Analytic Model Uncertainty analysis (i.e., probabilistic sensitivity analysis) Uncertainty in Net Benefit Decision Uncertainty: probability of error Perfect information (infinite sample) – Present information = E(max net benefits for each iteration) – max of E(net benefits of all iterations) Expected Value of Perfect Information Upper bound on value of generating future evidence Q2: Generate Future Evidence? EVPI Active Learning • Definition: E(max net benefits for each iteration) – max of E(net benefits of all iterations) • Inputs to calculate EVPI: – Willingness to pay (how much society is willing to pay for an extra unit of health i.e., QALY) – QALYs for each intervention and Monte Carlo iteration – Costs for each intervention and Monte Carlo iteration – Net benefit = (QALYs)*willingness to pay - Costs Solution Net Benefit: A $ 25,000.00 $ 75,000.00 $ (50,000.00) $ 50,000.00 $ 25,000.00 Expected Net Benefit: A $ 25,000.00 EVPI $ 10,000.00 Net Benefit: B $ $ 50,000.00 $ 25,000.00 $ 50,000.00 $ 125,000.00 Expected Net Benefit: B $ 50,000.00 Choose Max Net Benefit A or B? $ 25,000.00 A $ 75,000.00 A $ 25,000.00 B $ 50,000.00 B $ 125,000.00 B Expected Max Net Benefit $ 60,000.00 Display EVPI Case $40,000 $35,000 $30,000 $25,000 $20,000 $15,000 $10,000 $5,000 $$25,000 $50,000 $75,000 $100,000 $125,000 $150,000 $175,000 $200,000 $225,000 $250,000 $275,000 $300,000 $325,000 $350,000 $375,000 $400,000 $425,000 $450,000 $475,000 $500,000 EVPI EVPI across varying WTP values Willingness to pay (US dollars) Reason for a Data Table • The EVPI example was based on one willingness-to-pay value • What if we wanted to know what EVPI was at $50,000/QALY or $75,000/QALY? • To answer this we could manually calculate EVPI for different values of willingness-to-pay • Excel can automatically calculate this and record the values in one table using a data table Create the Data Table • Requirements for Data Table – input cell (willingness-to-pay) that is used to calculate the output (net benefit used to calculate EVPI) – A column of varying input values willingness-to-pay of your choosing (e.g., $5,000 - $100,000/QALY) • Highlight cells and click the "Data" tab > "What-If Analysis" > "Data Table" • This will prompt a box with row and column input cells. – If your WTP values are set up as columns (inputs moving down) enter the in the column input cell • To update the calculation please press F9 on a PC or CMD += on a mac Excel Screen Shots Adoption and research decisions A number of conceptually distinct but simultaneous decisions must be made: • Which technology should be adopted into clinical practice given the existing evidence base and the uncertainty surrounding outcomes and resource use? • Is additional evidence required to support the use of the technology? - How uncertain are the expected benefits? - Does this uncertainty matter (will it change the adoption decision)? - How much does it matter (consequences of getting it wrong)? • What type of evidence would be most valuable? • Which research designs would be worthwhile? • When to approve the technology? - Early approval? Can the evidence be provided with approval? Using Value of Information Analysis to Prioritise Health Research: Some Lessons from UK Experience Pilot studies for NICE and NCCHTA (Sculpher and Claxton, 2006) • Is further research required – – • What type of research – – • All subgroups should be included in research Only worth while for certain groups Which comparators – – • • RCTs of treatment effect Quality of life and costs Which subgroups – – • Research is not needed Research is a priority Head to head comparisons are needed Some comparators could be ruled out Which endpoints Length of follow-up Is further research required? Physiotherapy for adults with asthma or COPD did not appear to be CE and additional information was unlikely to change this assessment. EVPI is very high and additional evidence should be required to support reimbursement. Is further research required? What type of research? Further evidence about quality of life with influenza which is most important rather than additional evidence about the effect on symptoms which would require an RCT Is further research required? What type of research? Which endpoints and what length of trial is needed? If a RCT is undertaken, they need longer term follow-up than is currently collected. Using Value of Information Analysis to Prioritise Health Research: Some Lessons from UK Experience Conclusions • The results were considered by the NCCHTA and NICE – In general regarded the analysis to be interesting and potentially useful • In both cases the formal analysis failed to have a significant impact on the decisions taken – The NICE Research and Development committee decided to adopt a subjective scoring system • The decisions made by the panels and commissioning board did not seem to be informed by the results of the analysis Formalization of OIR and AWR for NICE • Expected cost-effectiveness • Irrecoverable costs – Costs committed by approval that cannot be recovered – Capital costs of long lived equipment (training and learning) – Initial losses (negative NB) offset by later gains – Significance depends on whether initiation of treatment can be delayed • Value of additional evidence • The need for evidence, type of evidence, design of research • Uncertainty that cannot be resolved by research but only over time • Are the benefits of early approval greater than the opportunity costs? Combined assessments will establish the most appropriate policy option: ‘Approve’, ‘Reject’, ‘Only in Research’, or ‘Approve with Research’ Current projects with EVPI • NIHR HTA: Graduated compression stockings for prevention of deep vein thrombosis in postoperative surgical patients • NIHR HTA: PROMIS trial MRI use for the diagnosis of prostate cancer • Early phase modelling Expected Value of Perfect Information: Active Learning Through User-Friendly Computations, Displays, and Application Discussions R Brett McQueen, PhD1 D. Eldon Spackman, PhD2 Jonathan D. Campbell, PhD1 1. University of Colorado, Aurora, CO 2. University of York, Heslington, York, UK