2 MB9_Veensta_Carlson_VOI_CER_symposium_V2
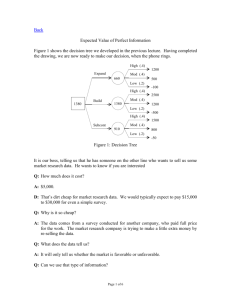
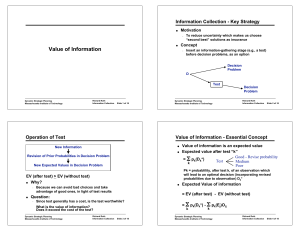
advertisement

Health Economics Tools for Research Prioritization : Value of Information (VOI) Methods and Applications for Comparative Effectiveness Research ITHS Institute Sept. 28, 2010 David Veenstra, PharmD, PhD Josh Carlson, MPH, PhD Pharmaceutical Outcomes Research and Policy Program, University of Washington 1 Agenda • Value of information theory • VOI Examples: – EGFR testing in advanced refractory NSCLC – Lung volume reduction surgery (NETT trial) • Incorporating VOI into research prioritization 2 Scenario • You have been appointed director of the National Heart Lung and Blood Institute. Your budget is $2.9 billion, most of which is devoted to investigatorinitiated projects (R01s). Still there is $14 million in “roadmap funds”, and many researchers have approached you with ideas for large multicenter collaborative projects to address “critical” questions. • Question: How will you allocate this money? A. B. C. D. Your own personal preferences Expert opinion What the political winds dictate is necessary Some other way Expected Value of Information (VOI) • Is there a way to make better decisions about funding future research so that uncertainty is reduced and the greatest number of people benefit from the knowledge that is gained? • VOI is proposed as a structured set of methods to prioritize areas where further research is needed to reduce uncertainty in decision making. Rationale: Expected value of information • Premise: Objective of the health care system is to maximize gains in health subject to a budget constraint • Current decisions are made under uncertainty possible that adopted medical interventions do not maximize net benefits • i.e. We could be making ‘wrong’ decisions about which treatments to use. • Health care system should be willing to pay for additional information if the value of additional information is greater than the cost to generate additional information How do we assess the value of additional information? • Value of additional evidence is evaluated by estimating the expected cost of uncertainty. • Probability decision based on existing information will be wrong (probability of error) • Consequences of a wrong decision (opportunity costs of error). • Applied over the impacted population • Applied over the time horizon for the technology Methods • Utilizes decision analysis – Compares a treatment and an alternative • Calculate the incremental net benefit of the treatment vs. alternative – INB = λ(B1-B0) – (C1-C0) – λ = societal willingness to pay for a unit of health benefit (e.g., a QALY) – OR, – INB = Willingness to pay X Incremental health gain – Incremental Costs Methods • Issue: – The parameters used to inform the model are uncertain (e.g., benefit of screening) – If the wrong decision is made, INB is negative Purpose • Estimate the impact of collecting additional primary data (e.g., clinical trial) on the decision – The additional information reduces the uncertainty regarding the decision – What is the value of this information relative to it’s cost? Expected Value of Perfect Information (EVPI) • If we had perfect information, we would not make a “wrong” decision • EVPI can be thought of as the value of new information obtained from a trial in which we have an infinite number of subjects • An upper bound on the returns from further research Expected Value of Perfect Parameter Information (EVPPI) • If we had perfect information about an individual parameter (e.g. mean survival for intervention) or set of parameters (mean survival for multiple interventions), we would not make a “wrong” decision due to these specific parameter(s). • EVPPI can be used to estimate the value of information about a specific set of parameters that might be collected with a particular type of study. – Clinical parameters (clinical trial) – Cost parameters (costing study) • An upper bound on the returns from further research for the parameter set 11 Expected Value of Sample Information (EVSI) • The value of new research before conducting a trial of a given sample size • Note that EVSI < EVPI • If the cost of research is less than the EVSI, the net benefit from the information is positive • Expected net benefit of sampling (ENBS) – The EVSI less the cost of sampling (i.e., a trial) – ENBS = EVSI – cost of sampling Past EVI studies: • Alzheimer’s disease drugs • Pentoxifylline to treat chronic venous leg ulcers • Preoperative patient management before major elective surgery EXAMPLES 14 Example: Cost-utility of EGFR-guided treatment of refractory NSCLC • Developed a decision analytic model to evaluate the cost-utility of EGFR protein expression or gene copy number testing compared to standard care with erlotinib in refractory advanced NSCLC patients. • Motivation for EVPI: • No clear ‘best’ treatment strategy • High uncertainty in the parameter estimates (especially survival estimates) Carlson JJ, Garrison LP, Ramsey SD, Veenstra DL.Value Health. 2009 Jan;12(1):20-7. Example: Cost-utility of EGFR-guided treatment of refractory NSCLC EVPI steps 1. Assign distributions to parameters (95% CI) 2. Run simulations to generate a series of iterations of model outputs (e.g. costs and QALYs) – Possible realization of the true outcomes given uncertainty 3. Calculate the net benefit 4. Generate per person EVPI 5. Calculate effective population • # of patients impacted over lifetime of technology 6. Generate population EVPI • Per person EVPI times effective population Population EVPI EVPI @ $100,000/QALY for US pop. % Incidence of lung cancer (US 2007) Count Source 213,380 SEER (2007) Advanced/Distant stage 41% 87,486 SEER website (1988-2003) NSCLC 80% 69,989 Ramsey et al. (2006) Likely to be treated with chemotherapy 79% 55,151 Ramsey et al. (2006) Likely to receive 2nd line treatment 32% 17,496 Kutakova et al. (2005) EVPI per person @ $100,000/QALY $381 Discounted EVPI in US over 5 years 1 $6,663,196 2 $6,469,122 3 $6,280,701 4 $6,097,768 5 $5,920,163 Total Abbreviations: EVPI=expected value of perfect information, NSCLC=non-small cell lung cancer $31,430,951 Cost-effectiveness frontier CE frontier indicates the probability that the alternative with the highest net-benefit will be cost-effective Next Steps • Expected value of perfect parameter information (EVPPI) • Difference between expected net benefit (ENB) of perfect information about a set of related parameters (e.g. survival estimates) and ENB with current information • Better represents how future research would be conducted • Expected value of sample information (EVSI) • Difference between ENB with increased sample size and ENB with current information • Future research will not provide perfect information, but rather better estimates (smaller confidence intervals) Expected value of perfect parameter information (EVPPI) Effective population* 17,496 Ceiling ratio Cost Safety and survival Utilities $50,000 $0 $76,245,000 $0 $100,000 $0 $9,838,000 $13,193,000 $150,000 $10,894,000 $119,839,000 $101,905,000 21 Assessing the value of a study - EVSI Example: A Multicenter Trial of Lung Volume Reduction Surgery For Patients with Severe Emphysema Lung Volume Reduction Surgery (LVRS) • Palliative surgical treatment for severe emphysema • Multiple wedges resected from damaged lung • Preliminary data show promising results: – Pulmonary function ~ 30% improvement – Reduced need for supplemental oxygen – Exercise capacity (6-minute walk) ~ 25% increase – Improved quality of life (SF-36, lung disease-specific QOL measures) LVRS: Concerns • Morbidity: – 30-50% post-surgery air leaks • Mortality (30 day): 5-10% • Limitations of published clinical trial data: – Unclear & nonstandardized patient selection criteria – Lack of control populations – Small sample size (<50 patients/study) – Short follow-up periods – Limited information on quality of life Economics of LVRS • Mean reimbursement (HCFA): – $25,268 (max $251,222) • Estimated U.S. expenditure, 7/94-12/95 – $100,000,000 ($30m HCFA) • Potential expenditure? – 2 million individuals with COPD – ~150,000 new cases annually National Emphysema Treatment Trial (NETT) • 18 centers throughout U.S. • 2,600 patients to be randomized • Three study arms – Usual care + intensive pulmonary rehab – Pulmonary rehab + LVRS by median sternotomy – Pulmonary rehab + LVRS by thoracoscopy • Follow-up 3-5 years Question • What is the value of an investment in a trial to learn more about the effectiveness and cost-effectiveness of LVRS? Value of Information National Emphysema Treatment Trial • Consider – Impact of LVRS and MT on quality of life, survival – Cost of LVRS and MT – Expected life of the technology – Eligible patients over life of technology – Value of a Quality Adjusted Life Year • $50,000/QALY, $100,000/QALY Inputs for the Expected Value of Information Calculations (1996 dollars) Parameter† Cost Distribution Mean, Lung Volume Reduction Group Normal $53498± $3527 n = 23 $26032 ± $3219 n = 228 $8935±$1105 n = 228 $8935±$1105 n = 228 0.34 0.34 3 3 1.78 ± 0.93 n = 22 1.69 ± 0.82 n = 22 Cost of medical therapy, per year* 2-year perioperative mortality rate** Long term survival (years) Quality of life (utilities) Number of persons in the United States expected to utilize LVRS if found effective, per year Duration of use of LVRS in clinical practice, years Normal 20,000 10 Mean, Medical Therapy Group Costs Associated with Conducting the National Emphysema Treatment Trial Expense Expenditure (2003 dollars) Study costs (investigators, support staff, clinical study coordinators, etc) $37,225,000 Participant travel costs (paid from study funds) $91,000 Patient evaluation and preparation costs, including the pre-trial rehabilitation program* $2,683,000 Post-therapy rehabilitation $1,052,000 Trial-related treatment costs*† $18,112,000 Total Estimated Expenditure $59,163,000 *Based on CMS claims for NETT participants. VOI for LVRS at WTP Thresholds of $50,000 and $100,000 per QALY assuming 1250 subjects per arm Threshold WTP/QALY Incremental net benefit Expected net benefit of sampling Probability of change in decision WTP = $50,000/QALY WTP = $100,000/QALY $305,000/QALY $305,000/QALY $3.41 billion $7.23 billion 0.04 0.24 Ramsey SD, Blough DK, Sullivan SD.Med Care. 2008 May;46(5):542-8. NETT Outcomes: Mortality and Exercise Capacity† All Patients Mortality RR = 1.01 Exercise OR = 6.27 Non High Risk Patients Mortality RR = 0.89 Exercise OR = 6.78* Upper Lobe Low Exercise Death RR = 0.47* Exercise OR = ∞* Upper Lobe High Exercise Death RR = 0.98 Exercise OR = 5.81* High Risk Patients Mortality RR = 1.82* Exercise OR = 3.48 Non Upper Lobe Low Exercise Death RR = 0.81 Exercise OR = 1.77 Non Upper Lobe High Exercise Death RR = 2.06* Exercise OR = 0.90 †Δ ≥ 10 watts * = p≤0.001 Cost-Effectiveness for Subgroups at 3 Years Cost per QALY Gained at 3 years Subgroup High Risk (n=138) Dominated* Upper Lobe + Low Exercise Capacity (n=137) Upper Lobe + High Exercise Capacity (n=204) Non Upper Lobe and Low Exercise Capacity (n=82) Non Upper Lobe and High Exercise Capacity (n=108) $98,000 $240,000 $330,000 Dominated* *Dominated: higher costs and less favorable outcomes for the LVRS group Ramsey SD, Berry K, Etzioni R, Kaplan RM, Sullivan SD, Wood DE; National Emphysema Treatment Trial Research Group.N Engl J Med. 2003 May 22;348(21):2092-102. VOI and Research Prioritization: CANCERGEN • CER project evaluating genomic tests in cancer • 6 top candidates for RCT selected using landscape analysis • 3 top candidates selected by stakeholder group • Using VOI approaches to help inform final selection for development of CER RCT Candidates • Tumor markers for detection of BrCA recurrence – validity not established – commonly used • EGFR mutation testing for tyrosine kinase inhibitor therapy in lung cancer – mutations relatively rare – large effect on treatment outcomes • ERCC1 testing in early-stage lung cancer – significant side effects of chemo – recurrence clinically impactful Process • Develop disease models – assumptions with expert input • Calculate EVPI and EVPPI – rank tests – identify study types • Calculate EVSI – provide support for study funding – refine study design Conclusions Expected Value of Information • A promising method for allocating scarce research funds to maximize the benefit of each funded study • But – Conceptually difficult – Computationally complex – Requires time consuming simulation modeling • Ongoing research may yield a tractable approach Extra Slides Population EVPI over range of willingness to pay thresholds Population EVPI (Millions) $300 $250 $200 $150 $100 $50 $0 $0 $50,000 $100,000 $150,000 $200,000 $250,000 $300,000 Societal Willingness to Pay (per QALY) • Increasing willingness to pay opportunity cost of wrong decisions is higher higher EVPI • But will also increase the expected net benefit (QALY x WTP) and probability of error will fall which may decrease the EVPI. • EVPI will ultimately increase decision uncertainty falls at a declining rate while the value of opportunity losses increases at a constant rate EVPI per person Value of information • Expected value of perfect information (EVPI) • Difference between the expected net benefit (ENB) of perfect information (no wrong decisions) and the expected net benefit with current information • Provides the upper bound value of additional information • Expected Net Benefits = QALYs x willingness to pay for health gains – costs • Current decision = treatment with highest expected net benefits (i.e. maximum of the average net benefit over all iterations) • Decision with perfect information = average of the maximum net benefits for each iteration Calculating EVPI Treatment Optimal choice Maximum net benefit Opportunity loss A B Iteration 1 9 12 B 12 0 Iteration 2 12 10 A 12 2 Iteration 3 14 20 B 20 0 Iteration 4 11 10 A 11 1 Iteration 5 14 13 A 14 1 Expectation 12 13 13.8 0.8 • Each iteration represents a possible future realization of the model under existing uncertainty